Surgical mortality with oncologic surgery varies widely in the United States. Patients, providers, and payers are paying closer attention to these variations and a way of reducing them. Although different hospital and surgical technologies and processes of care may account for some of this variation, there is an increasing awareness of the role of hospital safety culture. There is a growing body of evidence suggesting the importance of reducing mortality rates after major complications as a means to reducing the disparate mortality rates with oncologic surgery.
- •
Variations in hospital mortality rates with oncologic resections vary widely.
- •
Failure to rescue seems to play an important role in these differences.
- •
Hospital resources and the attitudes and behaviors among caregivers in inpatient wards and ICUs may affect the ability to effectively rescue patients from major surgical complications.
Mechanisms underlying variations in hospital mortality rates are not well understood. Elucidating the clinical mechanisms underlying these variations is important to develop more effective strategies for quality improvement. That hospitals with high mortality rates simply have higher complication rates is a common notion. Indeed, many organizations, including the Centers for Medicare and Medicaid Services (CMS), focus their quality improvement efforts on reducing complications. However, there is a growing body of evidence suggesting that complications and mortality are not related, that is, hospitals with high rates of complications do not necessarily have high rates of mortality. Thus, there must be other explanations for the existing hospital variations in mortality rates. One such explanation may be that hospitals with high mortality rates may not be proficient at recognizing and managing serious complications once they occur, a phenomenon known as failure to rescue.
Answers to such questions have obvious implications for the types of quality improvements that are likely to be effective in cancer surgery. Evidence that excess mortality is attributable primarily to the development of complications would imply the need for interventions aimed at processes related to perioperative care. Variation in failure to rescue rates would instead suggest the need to focus on processes related to the recognition and management of major postoperative complications.
Understanding wide variations in surgical mortality
More than 100,000 patients undergo major cancer resections each year in the United States. Many of these procedures are complex and associated with high rates of mortality. Previous research suggests that morbidity and mortality rates are strongly influenced by the hospital and by the surgeon who performs the oncologic operation. Although robust, risk-adjusted provider-specific data on performance are generally lacking for cancer surgery, there is little doubt that patient outcomes vary as a function of hospital volume, surgeon volume, and surgical specialty training. Variations in provider performance can have a major cumulative effect on patient prognosis. For example, one analysis estimated that patients undergoing surgery for colon, lung, or pancreatic cancer lose between 6 and 18 months of life expectancy in being treated at low-volume hospitals.
Such data suggest opportunities for improving the quality of cancer surgery in the United States. This could occur by 2 alternative mechanisms: Selective referral, cancer surgery patients could be directed to hospitals (or surgeons) likely to get the best results; Quality improvement, aimed at making cancer surgery safer and more effective in the settings in which it is currently being performed. This article focuses on the latter.
Increased postoperative complication rates are generally attributed to increased mortality. Several studies have found that higher mortality rates at poorly performing hospitals are due to more frequent complications. However, there is a growing body of evidence that complication incidence and mortality do not share a causal pathway at the hospital level. For example, a retrospective study of coronary artery bypass grafting using national hospital discharge data found that after adjusting for patient severity, there were no correlations between hospital complication rates and hospital mortality rates. Furthermore, other investigators have demonstrated through advanced statistical methods that patient characteristics (ie, age, gender, race, and comorbidities) account for postoperative complications and hospital characteristics (ie, number of beds, percentage of board certified surgeons and anesthesiologists, and nurse to bed ratios) account more for hospital mortality. Historically, operative mortality rates and complication rates have been used as quality indicators for the hospital and surgeon; however, there are clearly some pitfalls to using these imprecise measures. Therefore, Silber and colleagues introduced a new measure called failure to rescue. The original description of failure to rescue used a low-mortality operation, open cholecystectomy. Even so, there was a significant association between failure to rescue and variations in mortality rates for open cholecystectomy. More importantly, the investigators found that failure to rescue was associated more with hospital characteristics than patient factors, which provided some insight into the understanding of variations in mortality rates across hospitals.
Recent advances in knowledge
Although previous studies could be criticized by their reliance on administrative data (and their limitations regarding risk adjustment and identification of complications), their main findings were subsequently confirmed by the authors’ study published last year in the New England Journal of Medicine . Based on detailed clinical data from American College of Surgeons National Surgical Quality Improvement Program , the authors’ ranked 186 participating hospitals based on their overall risk-adjusted mortality rates and grouped them into quintiles. As seen in Fig. 2 , hospitals with high mortality rates and those low mortality rates had virtually identical rates of complications and those of major complications. Instead, hospitals with low mortality rates were distinguished by how well they minimized mortality once a complication had occurred, that is, how well they rescued patients ( Fig. 1 ).
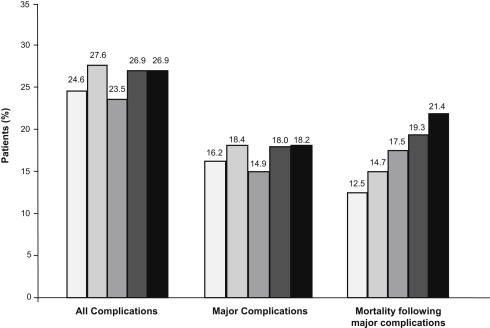
These findings show the importance of timely recognition and effective management of postoperative complications and have obvious implications for the types of strategies likely to reduce surgical mortality.
Understanding failure to rescue
Understanding what leads to increased rates of failure to rescue has yet to be determined. Although recent studies have demonstrated the important association between variations in hospital mortality rates and failure to rescue, there is a scant body of evidence evaluating hospital characteristics associated with failure to rescue. There is some empiric evidence suggesting several candidate factors. Multiple hospital-level resources could provide reasonable insight into failure-to-rescue, such as nurse to patient ratios, hospital size, presence of certified intensivists, availability of cardiac catheterization laboratories, and high-technology equipment. For example, Silber and colleagues recently demonstrated the importance of hospital-teaching intensity in survival after general, vascular, and orthopedic surgery. Patients undergoing surgery at hospitals with high teaching intensity had a 15% lower odds of death. However, although complication rates did not vary widely, the rates of failure to rescue were very important in explaining the differences in outcomes at teaching hospitals. The successful rescue of a patient who develops a postoperative complication relies heavily on hospital systems and teamwork. The sequence of events following the development of a major complication, such as a pulmonary embolism, can be very different depending on established hospital pathways or communication systems. For example, a nurse’s role in identification of a hypoxic patient with dyspnea is an integral sentinel event in the management of this complication. The nurse must then communicate his/her findings to the surgeon effectively and ensure that timely intervention or reassessment occurs. Further, the availability of adjunctive radiologic studies and timely availability and administration of intravenous heparin are some examples of hospital resources and health care team systems that can make the difference between a positive or negative outcome. The importance of such factors has been established in the literature. For example, Pronovost and colleagues identified approximately a 3-fold decrease in postoperative mortality rates of patients with abdominal aortic aneurysm repairs with daily rounds by the physicians in intensive care unit. Furthermore, Friese and colleagues found a 37% increased odds of death for patients undergoing oncologic surgery in hospitals with poor nursing environments. These are just a few examples of possible hospital level factors that may influence the ability of hospitals to rescue patients from major complications.
In addition, although not directly examining failure to rescue, there have been several studies examining hospital attributes associated with surgical mortality. For example, there is a large body of work supporting the notion that favorable nursing environments can help reducing the rates of surgical mortality. In a study of hospitals in Pennsylvania, Aiken and colleagues found that each additional patient per nurse was associated with a 7% increase in the likelihood of dying within 30 days of surgery. The authors’ recent studies build on this existing work by demonstrating that these associations with mortality are likely mediated through an impact on the rates of failure to rescue.
Teaching status, nurse staffing, and hospital technology have been identified as the 3 factors most highly associated with failure to rescue ( Table 1 ). Clinically, it is intuitive that these hospital attributes would provide an environment conducive to timely recognition and management of major complications. For example, first, a nurse who has fewer patients to care for may quickly identify a postoperative patient with acute hypoxia. Next, having house staff present 24 hours a day, 7 days a week would allow for rapid communication of this finding to a physician who could then initiate the appropriate evaluation. Finally, particular hospital systems (ie, electronic medication ordering and availability of advanced radiographic capabilities) may increase the likelihood of this patient receiving the appropriate diagnosis or intervention. Although these are plausible clinical explanations for the observed associations in our study, a causal link cannot be established using these data (see Table 1 ).