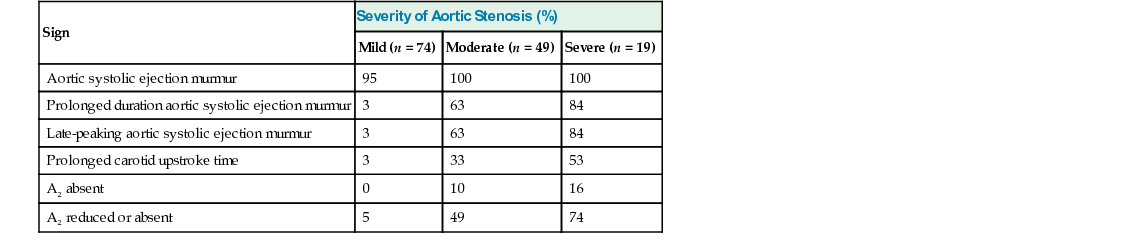
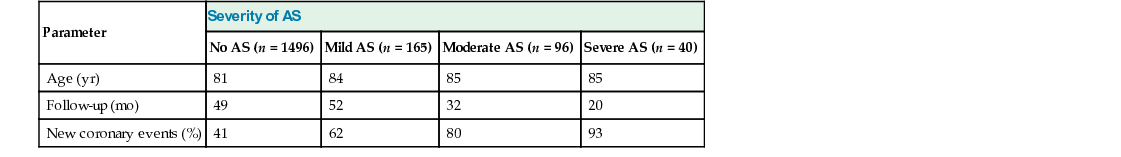
Wilbert S. Aronow Valvular aortic stenosis (AS) in older adults is usually due to stiffening, scarring, and calcification of the aortic valve leaflets. The commissures are not fused, as in rheumatic AS. Calcific deposits in the aortic valve are common in older adults and may lead to valvular AS. Aortic cuspal calcium was present in 295 of 752 men (36%), mean age 80 years, and in 672 of 1663 women (40%), mean age 82 years.1 Of 2358 persons, mean age 81 years, 378 (16%) had valvular AS, 981 (42%) had valvular aortic sclerosis (thickening of or calcific deposits on the aortic valve cusps, with a peak flow velocity across the aortic valve = 1.5 m/sec), and 999 (42%) had no valvular AS or aortic sclerosis.2 Calcific deposits in the aortic valve were present in 22 of 40 necropsy patients (55%) aged 90 to 103 years.3 Calcium of the aortic valve and mitral annulus may coexist.4–7 In the Helsinki Aging Study, calcification of the aortic valve was diagnosed by Doppler echocardiography in 28% of 76 persons aged 55 to 71 years, in 48% of 197 persons aged 75 to 76 years, in 55% of 155 persons aged 80 to 81 years, and in 75% of 124 persons aged 85 to 86 years.8 Aortic valve calcification, aortic sclerosis, and mitral annular calcium (MAC) are degenerative processes,4,3,9–11 accounting for their high prevalence in older adults. Otto and colleagues10 have shown that the early lesion of degenerative AS is an active inflammatory process, with some similarities to atherosclerosis, including lipid deposition, macrophage and T cell infiltration, and basement membrane disruption. In a study of 571 persons, mean age 82 years, 292 (51%) had calcified or thickened aortic cusps or root.12 A serum total cholesterol of 200 mg/dL, a history of hypertension, diabetes mellitus, and a serum high-density lipoprotein cholesterol level less than 35 mg/dL were more prevalent in older adults with calcified or thickened aortic cusps or root than in older adults with normal aortic cusps and root.12 In the Helsinki Aging Study, age, hypertension, and a low body mass index were independent predictors of aortic valve calcification.13 In 5201 persons older than 65 years in the Cardiovascular Health Study, independent clinical factors associated with degenerative aortic valve disease included age, male gender, smoking, history of hypertension, height, and high lipoprotein(a) and low-density lipoprotein (LDL) cholesterol levels.11 In 1275 older adults, mean age 81 years, AS was present in 52 of 202 (26%) with 40% to 100% extracranial carotid arterial disease (ECAD) and in 162 of 1073 (15%) with 0% to 39% ECAD.14 In 2987 older adults, mean age 81 years, symptomatic peripheral arterial disease occurred in 193 of 462 (42%) with AS and in 639 of 2525 (25%) without AS.15 In 290 persons, mean age 79 years, with valvular AS, who had follow-up Doppler echocardiography, older adults with MAC had a greater reduction in aortic valve area per year than older adults without MAC.16 Significant independent risk factors for the progression of valvular AS in 102 older adults, mean age 76 years, who had follow-up Doppler echocardiography were cigarette smoking and hypercholesterolemia.17 Palta and associates18 have also shown that cigarette smoking and hypercholesterolemia accelerate the progression of AS. These and other data suggest that aortic valve calcium, MAC, and coronary atherosclerosis in older adults have similar predisposing factors.10–20 A retrospective analysis of 180 older adult patients with mild AS who had follow-up Doppler echocardiography at 2 or more years showed that significant independent predictors of the progression of AS were male gender, cigarette smoking, hypertension, diabetes mellitus, serum LDL cholesterol level equal to 125 mg/dL at follow-up, serum high-density lipoprotein (HDL) cholesterol level less than 35 mg/dL at follow-up, and use of statins (inverse association).21 A retrospective analysis of 174 older adult patients, mean age 68 years, with mild to moderate AS showed that statin therapy reduced the progression of AS.22 In a retrospective study of 156 older adult AS patients, mean age 77 years, statin therapy decreased the progression of AS by 54% at 3.7-year follow-up.23 In a prospective open-label study of 121 patients with an aortic valve area between 1.0 and 1.5 cm2, 61 patients with a serum LDL cholesterol level greater than 130 mg/dL were treated with rosuvastatin and 60 patients with a serum LDL cholesterol level less than 130 mg/dL did not receive statins.24 At 73-week follow-up, patients treated with rosuvastatin had significantly less progression of AS. These data differ from the results reported in 155 patients in the Scottish Aortic Stenosis and Lipid Lowering Trial, Impact on Regression Study, which included patients with extensive aortic valve calcification.25 Two trials are in progress investigating the effect of statins on AS. The frequency of AS increases with age. Valvular AS, as diagnosed by Doppler echocardiography, was present in 141 of 924 older men (15%), mean age 80 years, and in 322 of 1881 older women (17%), mean age 81 years.26 Severe valvular AS (peak gradient across aortic valve = 50 mm Hg, or aortic valve area < 0.75 cm2) was diagnosed in 62 of 2805 older adults (2%).26 Moderate valvular AS (peak gradient across aortic valve = 26 to 49 mm Hg, or aortic valve area = 0.75 to 1.49 cm2) was present in 149 of 2805 older adults (5%).26 Mild valvular AS (peak gradient across aortic valve =10 to 25 mm Hg, or aortic valve area = 1.50 cm2) occurred in 250 of 2805 older adults (9%).26 In 501 unselected older adults aged 75 to 86 years in the Helsinki Aging Study, critical AS was present in 3% and moderate to severe AS was present in 5% of the 501 older adults.8 In valvular AS, there is resistance to ejection of blood from the left ventricle into the aorta, with a pressure gradient across the aortic valve during systole and an increase in left ventricular (LV) systolic pressure. The pressure overload on the left ventricle leads to concentric LV hypertrophy, with an increase in LV wall thickness and mass, normalizing systolic wall stress, and maintenance of normal LVEF (LVEF) and cardiac output.27,28 A compensated hyperdynamic response is common in older women.29 Older adults with a comparable degree of AS have more impairment of LV diastolic function than younger persons.30 Coronary vasodilator reserve is more severely impaired in the subendocardium in patients with LV hypertrophy caused by severe AS.31 The compensatory concentric LV hypertrophy leads to abnormal LV compliance, LV diastolic dysfunction with decreased LV diastolic filling, and increased LV end-diastolic pressure, further increased by left atrial systole. Left atrial enlargement develops. Atrial systole plays an important role in diastolic filling of the left ventricle in those with AS.32 Loss of effective atrial contraction may cause immediate clinical deterioration in those with severe AS. Sustained LV hypertrophy eventually leads to LV chamber dilation, with reduced LVEF and ultimately congestive heart failure (CHF). The stroke volume and cardiac output decrease, mean left atrial and pulmonary capillary pressures increase, and pulmonary hypertension occurs. Older adults with both obstructive and nonobstructive coronary artery disease have an increased incidence of LV enlargement and LV systolic dysfunction.33 In a percentage of older adults with AS, the LVEF will remain normal, and LV diastolic dysfunction will be the main problem. In 48 older adults with CHF associated with unoperated severe valvular AS, the LVEF was normal in 30 of them (63%).34 The prognosis of those with AS and LV diastolic dysfunction is usually better than that of those with AS and LV systolic dysfunction, but is worse than that of those without LV diastolic dysfunction.34,35 Angina pectoris, syncope or near-syncope, and CHF are the three classic manifestations of severe AS. Angina pectoris is the most common symptom associated with AS in older adults. Coexistent coronary artery disease (CAD) is frequently present in them. However, angina pectoris may occur in the absence of CAD as a result of an increase in myocardial oxygen demand, with a decrease in myocardial oxygen supply at the subendocardial level. Myocardial ischemia in those with severe AS and normal coronary arteries is due to inadequate LV hypertrophy, with increased LV systolic and diastolic wall stresses causing reduced coronary flow reserve.36 Syncope in persons with AS may be caused by decreased cerebral perfusion following exertion when arterial pressure falls because of systemic vasodilation in the presence of a fixed cardiac output. LV failure with a reduction in cardiac output may also cause syncope. In addition, syncope at rest may be caused by a marked decrease in cardiac output secondary to transient ventricular or atrial fibrillation or transient atrioventricular block related to extension of the valve calcification into the conduction system. Coexistent cerebrovascular disease with transient cerebral ischemia may contribute to syncope in older adults with AS. Exertional dyspnea, paroxysmal nocturnal dyspnea, orthopnea, and pulmonary edema may be caused by pulmonary venous hypertension associated with AS. Coexistent CAD and hypertension may contribute to CHF in older adults with AS. Atrial fibrillation may also precipitate CHF in these persons. CHF, syncope, or angina pectoris was present in 36 of 40 older adults (90%) with severe AS, in 66 of 96 older adults (69%) with moderate valvular AS, and in 45 of 165 older adults (27%) with mild valvular AS.37 Sudden death occurs mainly in symptomatic AS older adults.34,37–40 It may also occur in 3% to 5% of asymptomatic older adults with AS.38,41 Marked fatigue and peripheral cyanosis in those with AS may be caused by a low cardiac output. Cerebral emboli causing stroke or transient cerebral ischemic attack, bacterial endocarditis, and gastrointestinal bleeding may also occur in older adults with AS. A systolic ejection murmur heard in the second right intercostal space, down the left sternal border toward the apex, or at the apex is classified as an aortic systolic ejection murmur (ASEM).5,41–43 An ASEM is commonly heard in older adults,4,5,41 occurring in 265 of 565 unselected older adults (47%).5 Of 220 older adults with an ASEM and technically adequate M-mode and two-dimensional echocardiograms of the aortic valve, 207 (94%) had aortic cuspal or root calcification or thickening.5 Of 75 older adults with an ASEM, valvular AS was diagnosed by continuous-wave Doppler echocardiography in 42 of them (56%).43 Table 43-1 shows that an ASEM was heard in 100% of 19 older adults with severe AS, in 100% of 49 older adults with moderate AS, and in 95% of 74 older adults with mild AS.42 However, the ASEM may become softer or absent in persons with CHF associated with severe AS because of a low cardiac output. The intensity and maximal location of the ASEM and transmission of the ASEM to the right carotid artery do not differentiate among mild, moderate, and severe AS.5,42,43 The ASEM may be heard only at the apex in some older adults with AS. The apical systolic ejection murmur may also be louder and more musical than the basal systolic ejection murmur in some older adults with AS. The intensity of the ASEM in valvular AS increases with squatting and by inhalation of amyl nitrite and decreases during the Valsalva maneuver. Prolonged duration of the ASEM and late peaking of the ASEM best differentiate severe AS from mild AS.5,42,43 However, the physical signs do not distinguish between severe and moderate AS (see Table 43-1).42,43 A prolonged carotid upstroke time does not differentiate between severe and moderate AS in older adults.42,43 A prolonged carotid upstroke time was palpable in 3% of older adults with mild AS, in 33% of older adults with moderate AS, and in 53% of older adults with severe AS (see Table 43-1).42 Stiff noncompliant arteries may mask a prolonged carotid upstroke time in older adults with severe AS. The pulse pressure may also be normal or wide rather than narrow in older adults with severe AS because of loss of vascular elasticity. An aortic ejection click is rare in older adults with severe AS because of loss of vascular elasticity and because the valve cusps are immobile.42,43 An absent or reduced A2 occurs more frequently in older adults with severe or moderate AS than in persons with mild AS (see Table 43-1). However, an absent or decreased A2 does not differentiate between severe and moderate AS.42,43 The presence of atrial fibrillation, reversed splitting of S2, or an audible fourth heart sound at the apex also does not differentiate between severe and moderate AS in older adults.43 The presence of a third heart sound in older adults with AS usually indicates the presence of LV systolic dysfunction and elevated LV filling pressure.44 Echocardiography is more sensitive than electrocardiography in diagnosing LV hypertrophy in an older person with AS.42 In 19 older adults with severe valvular AS, LV hypertrophy was diagnosed by electrocardiography in 58% of older adults and by echocardiography in 100% of older adults.42 In 49 older adults with moderate AS, LV hypertrophy was diagnosed by electrocardiography in 31% and by echocardiography in 96%. In 74 older adults with mild valvular AS, LV hypertrophy was diagnosed by electrocardiography in 11% and by echocardiography in 74%.42 Rounding of the LV border and apex may occur as a result of concentric LV hypertrophy. Poststenotic dilation of the ascending aorta is commonly seen. Calcification of the aortic valve is best seen by echocardiography or fluoroscopy. Involvement of the conduction system by calcific deposits may occur in older adults with AS. In a study of 51 older adults with AS who underwent aortic valve replacement, conduction defects occurred in 58% of 31 older adults with MAC and in 25% of 20 older adults without MAC.7 In another study of 77 older adults with AS, first-degree atrioventricular block occurred in 18%, left bundle branch block in 10%, intraventricular conduction defect in 6%, right bundle branch block in 4%, and left axis deviation in 17%.45 Complex ventricular arrhythmias may be detected by 24-hour ambulatory electrocardiography in those with AS. Older adults with complex ventricular arrhythmias associated with AS have a higher incidence of new coronary events than older adults with AS and no complex ventricular arrhythmias.46 M-mode and two-dimensional echocardiography and Doppler echocardiography are very useful in the diagnosis of AS. Of 83 persons with CHF or angina pectoris and a systolic precordial murmur in whom severe AS was diagnosed by Doppler echocardiography, AS was not clinically diagnosed in 28 of them (34%).47 Echocardiography can detect thickening, calcification, and reduced excursion of aortic valve leaflets.5 LV hypertrophy is best diagnosed by echocardiography.42 Chamber dimensions and measurements of LV end-systolic and end-diastolic volumes, LVEF, and assessment of global and regional LV wall motion provide important information on LV systolic function. Doppler echocardiography is used to measure peak and mean transvalvular gradients across the aortic valve and to identify associated valve lesions. Aortic valve area can be calculated by the continuity equation using pulsed Doppler echocardiography to measure LV outflow tract velocity, continuous-wave Doppler echocardiography to measure transvalvular flow velocity, and a two-dimensional long-axis view to measure LV outflow tract area.48,49 Aortic valve area can be detected reliably by the continuity equation in older adults with AS.49 Shah and Graham50 have reported that the agreement in quantitation of the severity of AS between Doppler echocardiography and cardiac catheterization was greater than 95%. Those with a peak jet velocity greater than 4.5 m/sec had critical AS, and those with a peak jet velocity less than 3.0 m/sec had noncritical AS. Slater and coworkers51 demonstrated a concordance between Doppler echocardiography and cardiac catheterization in the decision to operate or not to operate in 61 of 73 older adults (84%) with valvular AS. In 75 older adults, mean age 76 years, with valvular AS, the Bland-Altman plot showed that 4 of the 75 older adults (5%) had disagreement between cardiac catheterization and Doppler echocardiography that was outside the 95% confidence limit.52 Cardiac catheterization was performed in 105 older adults in whom Doppler echocardiography demonstrated an aortic valve area of 0.75 cm2 or a peak jet velocity of 4.5 m/sec, consistent with critical AS.53 Doppler echocardiography was 97% accurate in this subgroup. Cardiac catheterization was performed in this study in 133 older adults with noncritical AS. Doppler echocardiography was 95% accurate in this subgroup. Although most older adults do not require cardiac catheterization before aortic valve surgery, they require selective coronary arteriography before aortic valve surgery. Those in whom Doppler echocardiography shows a peak jet velocity between 3.6 and 4.4 m/sec and an aortic valve area greater than 0.8 cm2 should undergo cardiac catheterization if they have cardiac symptoms attributable to AS.49 Those with a peak jet velocity between 3.0 and 3.5 m/sec and an LVEF less than 50% may have severe AS, requiring aortic valve replacement, and should undergo cardiac catheterization.50 Those with a peak jet velocity between 3.0 and 3.5 m/sec and an LVEF greater than 50% probably do not need aortic valve replacement (AVR) but should undergo cardiac catheterization if they have symptoms of severe AS.50 Ross and Braunwald38 have demonstrated that the average survival rate was 3 years after the onset of angina pectoris in those with severe AS. They reported that their average survival rate after the onset of syncope was 3 years and that the average survival rate after the onset of CHF in those with severe AS was 1.5 to 2 years. Persons with symptomatic severe valvular AS have a poor prognosis.37–40,54 At the National Institutes of Health, 52% of those with symptomatic severe valvular AS not operated on were dead at 5 years.39,40 At 10-year follow-up, 90% of them were dead. At 4-year follow-up of older adult patients aged 75 to 86 years in the Helsinki Aging Study, the incidence of cardiovascular mortality was 62% in those with severe AS and 35% in those with moderate AS.55 At 4-year follow-up, the incidence of total mortality was 76% in those with severe AS and 50% in those with moderate AS.55 In a prospective study, at 19-month follow-up (range, 2 to 36 months), 90% of 30 older adult patients with CHF associated with unoperated severe AS and a normal LVEF were dead.34 At 13-month follow-up (range, 2 to 24 months), 100% of 18 older adult patients with CHF associated with unoperated severe AS and an abnormal LVEF had died.34 Table 43-2 shows the incidence of new coronary events in older adults with no, mild, moderate, and severe AS. Independent risk factors for new coronary events in this study were prior myocardial infarction, AS, male gender, and increasing age.37 In this prospective study, at 20-month follow-up of 40 older adults with severe AS, CHF, syncope, or angina pectoris was present in 36 of 37 (97%) who developed new coronary events and in 0 of 3 (0%) without new coronary events.37 At 32-month follow-up of 96 older adults with moderate valvular AS, CHF, syncope, or angina pectoris was present in 65 of 77 (84%) who developed new coronary events and in 1 of 19 (5%) without new coronary events.37 At 52-month follow-up of 165 older adults with mild AS, CHF, syncope, or angina pectoris was present in 40 of 103 older adult patients (39%) who developed new coronary events and in 5 of 62 older adult patients (8%) without new coronary events.37 In a prospective study of 981 older adults, mean age 82 years, with aortic sclerosis and of 999 older adults, mean age 80 years, without valvular aortic sclerosis, older adults with aortic sclerosis at 46-month follow-up had a 1.8 times higher chance of developing a new coronary event than those without valvular aortic sclerosis.2 Otto and colleagues56 also reported that AS and aortic sclerosis increased cardiovascular morbidity and mortality in 5621 men and women aged 65 years. Kennedy and associates57 followed 66 older adults with moderate AS diagnosed by cardiac catheterization (aortic valve area, 0.7 to 1.2 cm2). In 38 older adults with symptomatic moderate AS and 28 older adults with minimally symptomatic moderate AS, the probabilities of avoiding death from AS were 0.86 and 1.0 for those with minimally symptomatic moderate AS at 1-year follow-up, 0.77 for those with symptomatic AS and 1.0 for those with minimally symptomatic AS at 2 years, 0.77 for those with symptomatic AS and 0.96 for those with minimally symptomatic AS at 3 years, and 0.70 for those with symptomatic AS and 0.90 for those with minimally symptomatic AS at 4 years.57 During the 35-month mean follow-up in this study, 21 older adults underwent aortic valve replacement. The Veterans Administration Cooperative Study on Valvular Heart Disease followed 106 older adults with unoperated AS for 5 years.58 During follow-up, 60 of 106 older adults (57%) died. Multivariate analysis has demonstrated that measures of the severity of the AS, presence of CAD, and presence of CHF were the important predictors of survival in unoperated older adults. Studies have shown that patients with asymptomatic severe AS are at low risk for death and can be followed until symptoms develop.59–62 Turina and colleagues59 followed 17 older adults with asymptomatic or mildly symptomatic AS. During the first 2 years, none died or had aortic valve surgery. At 5-year follow-up, 94% were alive and 75% were free of cardiac events. Kelly and associates60 followed 51 asymptomatic older adults with severe AS. During 17-month follow-up, 21 (41%) of them became symptomatic. Only 2 of 51 (4%) died of cardiac causes. In both of them, death was preceded by the development of angina pectoris or CHF. Pellikka and coworkers61 showed that 113 of 143 older adults (79%), mean age 72 years, with asymptomatic severe AS were not initially referred for AVR or percutaneous aortic balloon valvuloplasty. During 20-month follow-up, 37 of 113 of them (33%) became symptomatic. The actuarial probability of remaining free of cardiac events associated with AS, including cardiac death and aortic valve surgery, was 95% at 6 months, 93% at 1 year, and 74% at 2 years. No asymptomatic older adult with severe AS developed sudden death while asymptomatic. Rosenhek and colleagues62 followed 126 older adults with asymptomatic severe AS for 22 months. Eight of them died and 59 of them developed symptoms necessitating aortic valve replacement. Event-free survival was 67% at 1 year, 56% at 2 years, and 33% at 4 years. Five of the six deaths from cardiac disease were preceded by symptoms. Of those with moderately or severely calcified aortic valves whose aortic jet velocity increased by 0.3 m/sec or more within 1 year, 79% underwent AVR or died within 2 years of the observed increase. However, other studies have demonstrated that those with asymptomatic severe AS should be considered for AVR (AVR).63,64 Of 338 older adult patients with severe asymptomatic AS, mean age 71 years, 99 (29%) had AVR during a mean follow-up of 3.5 years.63 Survival at 1, 2, and 5 years in the nonoperated patients was 67%, 56%, and 38%, respectively, compared with 94%, 93%, and 90%, respectively, in those who underwent AVR (P < .0001).63 In this study, unoperated patients had a 48% significant reduction in mortality if they were treated with statins and a significant 48% reduction in mortality if they were treated with β-blockers.63 Data were analyzed for 622 older adult patients, mean age 72 years, with asymptomatic severe AS at the Mayo Clinic.64 After the initial diagnosis, 166 (27%) developed chest pain, shortness of breath, or syncope and had AVR. Another 97 older adult patients (16%) had AVR in the absence of symptoms. The operative mortality was 2% for the symptomatic patients and 1% for the asymptomatic patients. The survival of the 263 older adult patients who had AVR was not significantly different from an age- and gender-matched population. The 10-year survival was 64% for symptomatic patients and 64% for asymptomatic patients who had AVR.64 At 3 years after the diagnosis of severe AS, 52% of the 622 older adult patients had had symptoms develop, had undergone AVR, or had died.64 Absence of AVR was an independent risk factor for mortality, with a hazard ratio of 3.53. Prophylactic antibiotics should not be used to prevent bacterial endocarditis in those with AS regardless of severity, according to current American Heart Association (AHA) guidelines.65 Persons with CHF, exertional syncope, or angina pectoris associated with moderate or severe AS should undergo AVR promptly. Valvular surgery is the only definitive therapy in these older adults.66 Medical therapy does not relieve the mechanical obstruction to LV outflow and does not relieve symptoms or progression of the disorder. Older adults with asymptomatic AS should report the development of symptoms possibly related to AS immediately to their physician. If significant AS is present in asymptomatic older adults, clinical examination and electrocardiography and Doppler echocardiography should be performed at 6-month intervals if AVR is not being considered. Nitrates should be used with caution in those with angina pectoris and AS to prevent the occurrence of orthostatic hypotension and syncope. Diuretics should be used with caution in those with CHF to prevent a decrease in cardiac output and hypotension. Vasodilators should be avoided. Digitalis should not be used for those with CHF and a normal LVEF unless needed to control a rapid ventricular rate associated with atrial fibrillation. Box 43-1 lists four class I indications and one class IIa indication for performing AVR in older adult patients with AS.67 AVR is the procedure of choice for symptomatic older adult patients with severe AS. Other class I indications for AVR in older adult patients with severe AS include patients undergoing coronary artery bypass surgery (CABS), those undergoing surgery on the aorta or other heart valves, and those with an LVEF less than 50%.67 Older adult patients with moderate AS undergoing CABS or surgery on the aorta or other heart valves have a class IIa indication for AVR.67 Although the American College of Cardiology (ACC)/AHA guidelines do not recommend AVR in older adult patients with asymptomatic severe AS and normal LVEF, other studies have suggested otherwise.63,64 The data from these two studies favor AVR in older adult patients with a diagnosis of asymptomatic severe AS when there is a low institutional perioperative mortality. In addition, of 197 consecutive older adult patients with asymptomatic severe AS, early AVR was performed in 102 of them (52%).68 The estimated actuarial 6-year all-cause mortality rates were 2% for AVR and 32% for the conventional treatment group. Despite being asymptomatic, older adult patients with very severe AS have a poor prognosis.69 Early elective AVR should be considered in these patients. Of 73 older adult patients with severe AS who did not undergo AVR, 15 (14%) died at 15-month follow-up.70 Of these 73, symptoms were thought to be unrelated to the AS in 31 patients. Exercise stress tests for symptoms were performed in only 4% of the 42 asymptomatic older adult patients.70 Asymptomatic patients with low-gradient severe AS and normal LVEF with reduced stroke volume index had aortic valve events similar to those with a normal stroke volume index at 46-month follow-up.71 Of 248 older adult patients with severe AS and normal LVEF, 94 had a low gradient (<30 mm Hg mean gradient; group 1), 87 had a moderate gradient (30 to 40 mm Hg mean gradient; group 2), and 67 had a severe gradient (>40 mm Hg mean gradient; group 3).72 Symptoms were present in 49% of group 1 patients, in 55% of group 2 patients, and in 60% of group 3 patients (P not significant). At 45- to 60-month follow-up, the incidence of AVR or death was 71% for group 1, 77% for group 2, and 76% for group 3 (P not significant). Kaplan-Meier survival curves for time to death in all three groups were significantly better for patients with AVR versus no AVR Echocardiography is recommended in asymptomatic patients with AS every year for severe AS, every 1 to 2 years for moderate AS, and every 3 to 5 years for mild AS.64 AVR is the procedure of choice for symptomatic older adults with severe AS. The bioprosthesis has less structural failure in older adults than in younger persons and may be preferable to the mechanical prosthetic valve for AS replacement in older adults due to the anticoagulation issue.73–76 Persons with mechanical prostheses need anticoagulant therapy indefinitely. Those with porcine bioprostheses may be treated with aspirin, 75 to 100 mg daily, unless he or she has atrial fibrillation, abnormal LVEF, previous thromboembolism, or a hypercoagulable condition.67,76 Box 43-2 lists four class I indications and two class IIa indications for antithrombotic therapy in older adult patients with AVR.67 Arom and associates77 performed AVR in 273 older adults aged 70 to 89 years (mean age, 75 years), 162 with AVR alone, and 111 with AVR plus CABS. Operative mortality was 5%. Late mortality at 33-month follow-up was 18%. At 5-year follow-up, actuarial analysis showed that overall survival was 66% for those with AVR alone, 76% for those with AVR plus CABS, and 74% for a similar age group in the general population. Culliford and coworkers75 performed AVR in 71 older adults aged 80 years, in 35 with AVR alone, and in 36 with AVR plus CABS. Hospital mortality was 6% in older adults s with AVR alone and 19% in older adults with both AVR plus CABS. At 1-year follow-up, survival from late cardiac death was 100% for older adults who had AVR alone and 96% for older adults who had AVR plus CABS. At 3-year follow-up, survival from late cardiac death was 100% for older adults who had AVR alone and 91% for older adults who had AVR plus CABS. Freedom from all valve-related complications (e.g., thromboembolism, anticoagulant-related complications, endocarditis, reoperation, prosthetic failure) was 93% at 1-year follow-up and 80% at 3-year follow-up. At follow-up, 65% of survivors were in New York Heart Association (NYHA) functional class I or II, 31% in NYHA functional class III, and 4% in NYHA functional class IV. Levinson and colleagues78 performed AVR in 71 octogenarians, mean age 82 years. The operative mortality was 9% in these older adults . At 28-month follow-up, 100% of the survivors were in NYHA functional class I or II. Actuarial 1-, 5-, and 10-year survival rates were 83%, 67%, and 49%, respectively. A U.K. heart valve registry has indicated that 30-day mortality was 6.6% in 1100 older adults aged 80 years (56% women) who underwent AVR.79 The actuarial survival was 89% at 1 year, 79% at 3 years, 69% at 5 years, and 46% at 8 years. AVR is associated with a reduction in LV mass and in improvement of LV diastolic filling.80,81 Hoffman and Burckhardt82 performed a prospective study in 100 older adults who had AVR. At 41-month follow-up, the yearly cardiac mortality rate was 8% in those with electrocardiographic LV hypertrophy and repetitive ventricular premature complexes (two couplets/24 hr during 24-hour ambulatory monitoring) and 0.6% in older adults without either of these findings. If LV systolic dysfunction in those with severe AS is associated with critical narrowing of the aortic valve rather than myocardial fibrosis, it often improves after successful AVR.83 In 154 older adult patients, mean age 73 years, with AS and LVEF of 35% who underwent AVR, the 30-day mortality was 9%. The 5-year survival was 69% in those without significant CAD and 39% in those with significant CAD. NYHA functional class III or IV was present in 58% of them before surgery versus 7% of them after surgery. Postoperative LVEF was measured in 76% of survivors at a mean of 14 months after surgery; improvement in LVEF was found in 76%.83 AVR was a procedure for symptomatic older adults with severe AS. In a Mayo Clinic study, the actuarial survival of 50 older adults, mean age 77 years, with symptomatic severe AS in whom AVR was refused (45 persons) or deferred (5 persons) was 57% at 1 year, 37% at 2 years, and 25% at 3 years.84 Because of the poor survival rate in this group, balloon aortic valvuloplasty should be considered when operative intervention is refused or deferred. Balloon aortic valvuloplasty is effective palliative therapy for some older adults with symptomatic AS, although restenosis with recurrence of symptoms is common.85–94 Rodriguez and associates91 found that in 42 older adults undergoing aortic valvuloplasty, mean age 78 years, the 2-year survival was 36% in those with an LVEF less than 40% and 80% in those with an LVEF greater than 40%. The 2-year event-free survival (freedom from aortic valve surgery or severe CHF) was 0% in persons with an LVEF less than 40% and 34% in persons with an LVEF greater than 40%.91 Block and Palacios86 found recurrence of symptoms, death, or hemodynamic evidence of restenosis in 56% of 90 older adults, mean age 79 years, an average of 5.5 months after aortic valvuloplasty. Kuntz and coworkers92 found immediate clinical improvement after successful aortic valvuloplasty in most of 205 older adults, mean age 78 years, but restenosis in more than 50% of the persons within 1 to 2 years. On the basis of the available data, balloon aortic valvuloplasty should be considered for older adults with symptomatic severe AS who are not candidates for aortic valve surgery and possibly for persons with severe LV dysfunction as a bridge to subsequent valve surgery.92–94 The European Society of Cardiology/European Association for Cardio-Thoracic Surgery 2012 guidelines stated that class I indications for AVR include the following: (1) symptomatic severe AS; (2) asymptomatic patients with severe AS undergoing CABS, surgery of the ascending aorta, or surgery of another valve; (3) asymptomatic severe AS with an LVEF less than 50%; and (4) asymptomatic severe AS with an abnormal exercise test showing symptoms on exercise clearly related to AS.95 Class IIa indications for AVR include the following: (1) high-risk patients with severe symptomatic AS suitable for transapical AVR but in whom AVR is favored by a heart team based on the risk profile and anatomic suitability; (2) asymptomatic severe AS and an abnormal exercise test showing a fall in blood pressure below baseline; (3) moderate AS in patients undergoing CABS, surgery of the ascending aorta, or surgery of another valve; (4) symptomatic patients with severe AS, normal LVEF, and a low gradient (<40 mm Hg); (5) symptomatic patients with severe AS, reduced LVEF, low gradient, and evidence of flow reserve; and (6) asymptomatic severe AS with none of the above if the surgical risk is low, and the peak transvalvular velocity is greater than 5.5 m/sec (very severe AS) or there is severe aortic valve calcification and a rate of peak transvalvular velocity progression of 0.3 m/sec/year. Transapical AVR should be considered in patients with severe symptomatic AS who are considered unsuitable for surgical AVR because of severe comorbidities.95 Follow-up was performed at a mean of 12.6 years in older adult patients aged 65 to 80 years undergoing AVR with a biologic (24,410 patients) or mechanical (14,789 patients) prosthesis.96 Long-term mortality rates were similar for both types of prostheses. Bioprostheses were associated with a higher risk of reoperation (255%) and endocarditis (60%) but a lower risk of stroke (13%) and hemorrhage (34%).96 Transcatheter aortic valve implantation (TAVI) may be performed in nonsurgical older adult patients with end-stage calcific AS.97,98 Eighteen high-risk older adult patients, mean age 76 years, with severe AS and moderate CAD amenable to percutaneous coronary intervention (PCI) had combined PCI followed by minimally invasive AVR.99 One of 18 of them (6%) died postoperatively, with no late mortality, after a mean follow-up of 19 months.99 Of 442 older adult patients with severe AS at increased surgical risk, mean age 82 years, 78 were treated with medical management, 107 with AVR, and 257 with TAVI.100 At 30-month follow-up, adjusted mortality was 49% significantly lower for AVR compared with medical treatment and 62% significantly lower for TAVI compared with medical treatment. At 1-year, 92.3% of AVR patients, 93.2% of TAVI patients, and 70.8% of medically treated patients were NYHA functional class I or II.100 In the Placement of Aortic Transcatheter Valves (PARTNER) trial, 699 high-risk older adult patients with severe AS, mean age 84 years, were randomized to AVR or TAVI.101 All-cause mortality was 3.4% for the TAVI group versus 6.5% for the AVR group at 30 days (P not significant) and 24.2% for the TAVI group versus 26.8% for the AVR group at 1 year (P not significant). Major stroke was 3.8% for the TAVI group versus 2.1% for the AVR group at 30 days (P not significant) and 5.1% for the TAVI group versus 2.4% for the AVR group at 1 year (P not significant). Major vascular complications at 30 days were 11.0% for the TAVI group versus 3.2% for the AVR group. New-onset atrial fibrillation was 16.0% after AVR and 8.6% after TAVI. Major bleeding was found in 19.5% after AVR and 9.3% after TAVI. At 1-year follow-up, there were similar improvements in cardiac symptoms for both groups.101 In the PARTNER trial, among inoperable patients with severe AS, TAVI caused significant improvements in health-related quality of life maintained for at least 1 year compared with standard care.102 At 2-year follow-up of 699 high-risk patients with severe AS in the PARTNER trial, all-cause mortality was 33.9% for TAVI and 35.0% for AVR (P not significant).103 The incidence of stroke was 7.7% for TAVI and 4.9% for AVR (P not significant). Moderate or severe paravalvular aortic regurgitation was 6.9% for TAVI and 0.9% for AVR and was associated with increased late mortality.103 At 2-year follow-up of 358 older adult patients, mean age 83 years, with inoperable severe AS in the PARTNER trial randomized to transcatheter AVR (TAVR) or to standard therapy with balloon aortic valvuloplasty performed in 82% of this group, 43% of the TAVR patients and 68% of the standard therapy patients were dead.104 The rates of cardiac death at 2 years were 31% for the TAVR group versus 62% for the standard therapy group. The rates of stroke at 2 years were 14% for the TAVR group versus 6% for the standard therapy group. The rates of rehospitalization at 2 years were 35% for the TAVR group versus 73% for the standard therapy group. Echocardiographic data showed a sustained increase in aortic valve area and a reduction in aortic valve gradient, with no worsening of paravalvular aortic regurgitation.104 These data suggest that the mortality benefit in patients with TAVR may be limited to older adult patients without extensive comorbidities. Low flow in patients with severe AS independently predicts mortality.105 At 2-year follow-up of 180 older adult patients, mean age 84 years, with low-flow inoperable severe AS in the PARTNER trial, the mortality was 76% in the standard therapy group versus 46% in the TAVR group.105 At 2-year follow-up of 350 older adult patients, mean age 84 years, with low-flow severe AS in the PARTNER trial, the mortality was 40% in the AVR group versus 38% in the TAVR group (P not significant).105 In the inoperable group in the PARTNER trial, at 2-year follow-up, all-cause mortality in older adult patients with a normal stroke volume index was 38% with TAVR versus 53% in those who had undergone medical management.105 One third of 270 patients undergoing a CoreValve TAVI needed a permanent pacemaker implanted within 30 days.106 Periprocedural atrioventricular block, balloon predilation, use of the larger CoreValve prosthesis, increased interventricular septum diameter, and prolonged QRS duration were independently associated with the need for implantation of a permanent pacemaker.106 At 42-month follow-up of 339 older adult patients, mean age 81 years, who had TAVI because they were considered to be inoperable or at very high surgical risk, 188 (56%) had died.107 The causes of late death in 152 patients were noncardiac comorbidities in 59%, cardiac death in 23%, and unknown in 18%.107 TAVI results in similar hemodynamic and long-term clinical outcomes for high-risk surgical patients with low-gradient severe AS as for those with typical severe AS.108 In the United States, the Society of Thoracic Surgeons (STS)/American College of Cardiology Transcatheter Valve Therapy Registry showed that 7,710 older adult patients underwent TAVR (20% who were inoperable and 80% who were high risk but operable).109 The median age was 84 years, 49% were women, and the median STS predicted risk of mortality was 7%. A transfemoral approach was used in 64%, a transapical approach in 29%, and other alternative approaches in 7%. In-hospital mortality was 5.5% and major vascular injury was 6.4%. At 30- day follow-up, the incidence of mortality was 7.6% (52% due to a noncardiovascular cause), of stroke was 2.8%, of dialysis-dependent renal failure was 2.8%, and of re-intervention was 0.5%.109 The 2012 ACCF/American Association for Thoracic Surgery/Society for Cardiovascular Angiography and Interventions/STS expert consensus document on TAVR recommended TAVR for patients with severe symptomatic calcific stenosis of a trileaflet aortic valve who have aortic and vascular anatomy suitable for TAVR and a predicted survival longer than 1 year and who have a prohibitive surgical risk. This was defined by an estimated 50% or greater risk of mortality or irreversible morbidity at 30 days or other factors such as frailty, prior radiation therapy, porcelain aorta, and severe hepatic or pulmonary disease.110 These guidelines also stated that TAVR is a reasonable alternative to AVR in patients at high surgical risk (PARTNER trial criteria: STS = 8%). These guidelines stated that major complications from TAVR are mortality (3% to 5%), stroke (6% to 7%), access complications (17%), pacemaker insertion (2% to 9% for Sapien and 19% to 43% for CoreValve), bleeding, prosthetic dysfunction, paravalvular aortic regurgitation, acute kidney injury, coronary occlusion, valve embolization, and aortic rupture.110 The European Society of Cardiology/European Association for Cardio-Thoracic Surgery guidelines have stated that TAVR is indicated for patients with severe symptomatic AS who are considered unsuitable for AVR as assessed by a heart team and who are likely to gain improvement in their quality of life and have a life expectancy of more than 1 year after consideration of their comorbidities (class I indication).95 TAVR should be considered for high-risk older adult patients with severe symptomatic AS who may still be suitable for AVR but for whom TAVR is favored by a heart team based on their individual risk profile and anatomic suitability (class IIa indication).95 Clinical absolute contraindications to TAVR include absence of a heart team and no cardiac surgery on site, estimated life expectancy less than 1 year, improvement of quality of life by TAVR unlikely because of comorbidities, severe primary associated disease of other valves with major contribution to symptoms that can be treated only by surgery, and anatomic contraindications (e.g., inadequate annulus size, thrombus in left ventricle, active endocarditis, increased risk of coronary ostium obstruction, plaques with mobile thrombi in the ascending aorta or arch, inadequate vascular access).95 Relative contraindications include bicuspid or noncalcified valves, untreated coronary artery disease requiring revascularization, hemodynamic instability, LVEF less than 20% and, for the transapical approach, severe pulmonary disease or the LV apex is not accessible.95 After TAVI, treatment with clopidogrel for 3 months in addition to aspirin is widely practiced. Acute aortic regurgitation (AR) in older adults may be due to infective endocarditis, rheumatic fever, aortic dissection, trauma following prosthetic valve surgery, or rupture of the sinus of Valsalva and causes sudden severe LV failure. Chronic AR in older adults may be caused by valve leaflet disease (secondary to any cause of AS, infective endocarditis, rheumatic fever, congenital heart disease, rheumatoid arthritis, ankylosing spondylitis, following prosthetic valve surgery, or myxomatous degeneration of the valve) or by aortic root disease. The cause of aortic root disease causing chronic AR in older adults includes association with systemic hypertension, syphilitic aortitis, cystic medial necrosis of the aorta, ankylosing spondylitis, rheumatoid arthritis, Reiter disease, systemic lupus erythematosus, Ehler-Danlos syndrome, and pseudoxanthoma elasticum. Mild or moderate AR was also diagnosed by Doppler echocardiography in 9 of 29 persons (31%) with hypertrophic cardiomyopathy. The prevalence of AR increases with age.111–113 Margonato and colleagues112 linked the increased prevalence of AR with age to aortic valve thickening. In a prospective study of 450 unselected older adults, mean age 82 years, AR was diagnosed by pulsed Doppler echocardiography in 39 of 114 men (34%) and in 92 of 336 women (27%).114 Severe or moderate AR was diagnosed in 74 of 450 older adults (16%). Mild AR was diagnosed in 57 of 450 older adults (13%). In a prospective study of 924 men, mean age 80 years, and 1881 women, mean age 82 years, valvular AR was diagnosed by pulsed Doppler recordings of the aortic valve in 282 of 924 men (31%) and in 542 of 1881 women (29%).26 The primary determinants of AR volume are the regurgitant orifice area, transvalvular pressure gradient, and duration of diastole.115 Chronic AR increases LV ventricular end-diastolic volume. The largest LV end-diastolic volumes are seen in those with chronic severe AR. LV stroke volume increases to maintain the forward stroke volume. The increased preload causes an increase in LV diastolic stress and the addition of sarcomeres in series, which results in an increase in the ratio of the LV chamber size to wall thickness. This pattern of LV hypertrophy is termed eccentric left ventricular hypertrophy. Primary myocardial abnormalities or ischemia due to coexistent CAD decrease the contractile state. LV diastolic compliance decreases, LV end-systolic volume increases, LV end-diastolic pressure rises, left atrial pressure increases, and pulmonary venous hypertension result. When the LV end-diastolic radius-to-wall thickness ratio rises, LV systolic wall stress increases abnormally because of the preload and afterload mismatch.28,116 Additional stress then decreases the LVEF response to exercise.117 Eventually, the LVEF, forward stroke volume, and effective cardiac output are decreased at rest. My colleagues and I have demonstrated that an abnormal resting LVEF occurs in 8 of 25 older adults (32%) with CHF associated with chronic severe AR.118 In those with acute severe AR, the left ventricle cannot adapt to the increased volume overload. Forward stroke volume falls, LV end-diastolic pressure increases rapidly to high levels,119 and pulmonary hypertension and pulmonary edema result. The rapid rise of the LV end-diastolic pressure to exceed the left atrial pressure in early diastole causes premature closure of the mitral valve.120 This prevents backward transmission of the elevated LV end-diastolic pressure to the pulmonary venous bed. Persons with acute AR develop symptoms due to the sudden onset of CHF, with marked dyspnea and weakness. Persons with chronic AR may remain asymptomatic for many years. Mild dyspnea on exertion and palpitations, especially on lying down, may occur. Exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, fatigue, and edema are common clinical symptoms when LV failure occurs. Syncope is rare. Angina pectoris occurs less often in older adult patients with AR than in older adult patients with AS and may be due to coexistent CAD. However, nocturnal angina pectoris, often accompanied by flushing, diaphoresis, and palpitations, may develop when the heart rate slows and arterial diastolic pressure falls to very low levels. Most of those with severe AR who do not have surgery die within 2 years after CHD develops.121
Valvular Heart Disease
Aortic Stenosis
Causes and Prevalence
Pathophysiology
Symptoms
Signs
Diagnosis
Electrocardiography and Chest Roentgenography
Echocardiography and Doppler Echocardiography
Natural History
Treatment
Medical Management
Surgical Treatment
Aortic Valve Replacement.
Balloon Aortic Valvuloplasty.
Transcatheter Aortic Valve Implantation.
Aortic Regurgitation
Causes and Prevalence
Pathophysiology
Symptoms
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Valvular Heart Disease
43