In the past 2 decades, the direct oral anticoagulants (DOACs) have emerged as alternatives to the standard therapy (unfractionated or low-molecular-weight heparin followed by vitamin K antagonists [VKA]), for the acute and extended treatment of venous thromboembolism. The DOACs have a more favorable pharmacologic profile and a predictable anticoagulant response and, therefore, have the potential to overcome some of the limitations associated with the use of VKA. Several ongoing registries are evaluating the use of the DOACs in routine clinical practice and will provide additional information in less selected patient populations.
Key points
- •
The direct oral anticoagulants have favorable pharmacologic profile: specific target on thrombin or factor Xa, rapid onset of action and short half-life, and predictable anticoagulant response.
- •
In the acute treatment of venous thromboembolism, they were noninferior in efficacy compared with the standard treatment and were associated with less major bleeding complications.
- •
In the extended treatment of venous thromboembolism, they showed superior efficacy compared with placebo. Clinically relevant bleeding was increased; however, the number of major bleeding was small.
- •
The benefit of the direct oral anticoagulants was confirmed also in special subgroups (eg, fragile patients) and in preliminary data from real-life clinical practice.
Introduction
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), is the third most common cardiovascular disease, after acute coronary syndromes and stroke. The estimated incidence of VTE is 1 to 2 per 1000 person-years, with DVT accounting for two-thirds and PE accounting for the remaining one-third of the episodes. VTE is a potentially fatal disorder, with an in-hospital case fatality rate associated with PE of approximately 10%, and it also carries a substantial risk of short- and long-term recurrent events as well as morbidities such as the postthrombotic syndrome and postembolic pulmonary hypertension.
For many years, the standard of treatment for the large majority of VTE patients has been based on the use of heparins, either unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH) followed by the oral vitamin K antagonists (VKA). However, all these compounds had some limitations, including parenteral administration for heparins and the need for routine coagulation monitoring and dose adjustments for VKAs. The direct oral anticoagulants (DOACs) have been developed to overcome some of these limitations. The DOACs have a favorable pharmacologic profile (eg, fast onset and offset of action) and a predictable anticoagulant response, thus making their use particularly interesting for both the acute phase treatment and the long-term secondary prevention of VTE.
Introduction
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), is the third most common cardiovascular disease, after acute coronary syndromes and stroke. The estimated incidence of VTE is 1 to 2 per 1000 person-years, with DVT accounting for two-thirds and PE accounting for the remaining one-third of the episodes. VTE is a potentially fatal disorder, with an in-hospital case fatality rate associated with PE of approximately 10%, and it also carries a substantial risk of short- and long-term recurrent events as well as morbidities such as the postthrombotic syndrome and postembolic pulmonary hypertension.
For many years, the standard of treatment for the large majority of VTE patients has been based on the use of heparins, either unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH) followed by the oral vitamin K antagonists (VKA). However, all these compounds had some limitations, including parenteral administration for heparins and the need for routine coagulation monitoring and dose adjustments for VKAs. The direct oral anticoagulants (DOACs) have been developed to overcome some of these limitations. The DOACs have a favorable pharmacologic profile (eg, fast onset and offset of action) and a predictable anticoagulant response, thus making their use particularly interesting for both the acute phase treatment and the long-term secondary prevention of VTE.
Pharmacologic properties of the direct oral anticoagulants
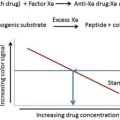
The DOACs act on specific targets in the coagulation cascade. According to their specific target, they are classified as direct thrombin inhibitors (eg, dabigatran) and direct factor Xa inhibitors (eg, apixaban, rivaroxaban, and edoxaban).
The onset of action ranges between 1 and 4 hours, thus allowing their use in the acute phase treatment of VTE, and the half-life ranges between 9 and 14 hours, thus allowing for a sufficiently rapid disappearance of the anticoagulant effect after discontinuation. When compared with the VKAs, the DOACs have also a lower potential for food and drug interactions and a lower interindividual and intraindividual variability in dose response; thus, routine coagulation monitoring is not needed. The pharmacologic characteristics of the DOACs are summarized in Table 1 .
| Dabigatran | Rivaroxaban | Apixaban | Edoxaban | |
|---|---|---|---|---|
| Mechanism of action | Direct thrombin inhibitor | Direct factor Xa inhibitor | Direct factor Xa inhibitor | Direct factor Xa inhibitor |
| Administration | Oral BID | Oral OD | Oral BID | Oral OD |
| Oral bioavailability | ∼ 6.5% | 66% (without food) >80% (with food) | 50% | 62% |
| Time to peak plasma concentration | 0.5–2 h | 2–4 h | 1–3 h | 1–2 h |
| Mean half-life | 12–14 h | 5–9 h (young adult) 11–13 h (elderly) | ∼12 h | 10–14 h |
| Renal clearance | 85% | 66% (only half as inactive metabolite) | 27% | 35% |
| Plasma protein binding | 35% (dialyzable) | ∼90% | 87% | ∼ 55% |
| Cytochrome P450 metabolism | No | Yes | Yes | Minimal |
| P-gp transport | Yes | Yes | Yes | Yes |
Dabigatran binds to the active site of the thrombin molecule, therefore inactivating both free and fibrin-bound thrombin; in contrast, the indirect inhibitors of thrombin and factor Xa (such as UFH or LMWH) do not inactivate fibrin-bound thrombin, which can continue to stimulate thrombus expansion. Dabigatran is orally administered as a prodrug, dabigatran etexilate. This formulation contains pellets of tartaric acid core coated with dabigatran etexilate and aims to create an acidic environment in the gastrointestinal tract, in order to reduce the variability in the absorption of the drug. Dabigatran etexilate is hydrolyzed into the active form, dabigatran, by nonspecific esterase in the gut, plasma, and liver. Steady state is achieved after 3 days of multiple-dose administration in healthy volunteers. Dabigatran has a low percentage of plasma protein binding of about 35%; therefore, it can be removed through dialysis. Approximately 80% is excreted unchanged through the kidney, while the remaining 20% is conjugated with glucuronic acid and excreted through the biliary system. Dabigatran is not metabolized by the cytochrome P450 enzymes and is a substrate of the efflux transporter P-glycoprotein (P-gp), located in the intestine and kidneys. Therefore, potent inhibitors (eg, quinidine, ketoconazole, amiodarone, and verapamil) can increase dabigatran absorption and potent inducers (eg, rifampicin) can decrease dabigatran absorption.
Rivaroxaban, apixaban, and edoxaban are direct inhibitors of the activated factor X (FXa), whereas the indirect inhibitors of thrombin and factor Xa require the cofactor antithrombin in order to inhibit factor Xa. They can bind directly not only free FXa but also FXa within the prothrombinase complex.
The bioavailability of rivaroxaban after oral administration is dose-dependent: 80% to 100% is reported for the 10-mg dose and 66% for the 20-mg dose in the fasted state. The administration with food results in delayed absorption but increased peak concentrations and is therefore recommended for therapeutic dosages. One-third of the drug is excreted unchanged through the urine, while the other two-thirds are transformed into inactive metabolites and eliminated half by the renal route and half by the fecal route. Rivaroxaban is a substrate for both cytochrome P450 enzymes and for P-gp transporter.
The bioavailability of apixaban is approximately 50% after oral administration, and plasma protein binding in humans is 87%. Several pathways are involved in the elimination of apixaban, each accounting for approximately one-third of the drug: hepatic metabolism, biliary and intestinal secretion, and renal clearance. Apixaban is a substrate of both cytochrome P450 and P-gp. However, apixaban has multiple elimination pathways, which can reduce the extent of drug-drug interaction. Conversely, apixaban does not significantly modulate the function of cytochrome P450 enzymes or P-gp transporter.
Bioavailability of edoxaban after oral administration is 62%. Edoxaban is transformed into several metabolites, mainly through hydrolysis; however, more than 70% is excreted unchanged. Approximately 35% of edoxaban is eliminated in the urine and 60% in the feces. Edoxaban is a substrate of the P-gp transporter, while only a very small percentage (approximately 4%) is metabolized by cytochrome P450.
Being substrates of P-gp transporter and cytochrome P450 3A4, factor Xa inhibitors share common drug-drug interactions. Strong P-gp and CYP3A4 inhibitors, such as azole-antimycotics (ketoconazole, itraconazole, posaconazole, voriconazole) and HIV protease inhibitors (ritonavir), may increase their plasma concentration, whereas potent P-gp inducers, such as some antiepileptic drugs (carbamazepine, phenytoin, phenobarbital) and some antibiotics (rifampicin), may reduce their plasma concentration.
Treatment of acute venous thromboembolism
Several randomized controlled trials investigated the use of the DOACs in patients with VTE. In the acute phase of treatment, dabigatran and edoxaban were administered after an initial course of parenteral anticoagulation, while rivaroxaban and apixaban were directly started as single drugs, using loading doses for the first few weeks.
Dabigatran was evaluated in the RE-COVER I and II trials, 2 randomized, double-blind and double-dummy trials in which more than 5000 patients with acute VTE, initially treated with parenteral anticoagulation (UFH or LMWH) for a median of 9 days, were randomized to fixed-dose dabigatran 150 mg twice daily (BID) or warfarin dose-adjusted to maintain an international normalized ratio (INR) between 2.0 and 3.0. In both trials, dabigatran was noninferior to warfarin in the primary efficacy outcome of recurrent symptomatic VTE or VTE-related death, which occurred in 2.4% of patients treated with dabigatran versus 2.1% of patients treated with warfarin in RE-COVER I (hazard ratio [HR] 1.10, 95% confidence interval [CI] 0.65–1.84) and in 2.3% versus 2.2%, respectively, in RE-COVER II (HR 1.08, 95% CI 0.64–1.80). When the results of the 2 trials were pooled, the incidence of major bleeding and of major or clinically relevant nonmajor bleeding during the double-dummy period was significantly lower with dabigatran (1.0% vs 1.6%; HR 0.60, 95% CI 0.36–0.99, and 4.4% vs 7.7%; HR 0.56, 95% CI 0.45–0.71, respectively). Dyspepsia was the only relevant side effect that emerged from these trials, reported in 1.0% to 2.9% of patients receiving dabigatran.
Rivaroxaban was evaluated in 2 open-label randomized controlled trials. The EINSTEIN-DVT trial enrolled 3449 patients with acute DVT, whereas the EINSTEIN-PE trial enrolled 4833 patients with acute symptomatic PE, regardless of the concomitant presence of DVT. In both trials, rivaroxaban was administered at a dosage of 15 mg BID for 21 days, followed by 20 mg once daily (OD) for 3, 6, or 12 months, and was compared with enoxaparin followed by VKAs. Rivaroxaban was noninferior to VKA with regard to the primary efficacy outcome of recurrent fatal or nonfatal VTE, which occurred in 2.1% patients on rivaroxaban and 3.0% patients on VKA in the EINSTEIN-DVT trial (HR 0.68, 95% CI 0.44–1.04) and in 2.1% and 1.8%, respectively, in the EINSTEIN-PE trial (HR 1.12, 95% CI 0.75–1.68). The principal safety outcome, a composite of major and clinically relevant bleeding, was similar in the 2 groups, occurring in 8.1% patients on rivaroxaban and 8.1% patients on VKA in the EINSTEIN-DVT trial (HR 0.97, 95% CI 0.76–1.22) and in 10.3% and 11.4%, respectively, in the EINSTEIN-PE trial (HR 0.90, 95% CI 0.76–1.07). However, in the EINSTEIN-PE trial, major bleeding complications were significantly less common with rivaroxaban (1.1% vs 2.2%; HR 0.49, 95% CI 0.31–0.79), and this was also observed in a pooled analysis of the 2 EINSTEIN trials (1.0% vs 1.7%; HR 0.54, 95% CI 0.37–0.79). Furthermore, in a post-hoc analysis of the EINSTEIN program, rivaroxaban was also associated with shorter hospital stay than enoxaparin/VKA (mean length of stay 4.5 vs 6.1 days).
Apixaban was evaluated in the AMPLIFY trial, a double-blind double-dummy trial in which 5400 patients with acute VTE were randomized to apixaban 10 mg BID for 7 days, followed by 5 mg BID, or subcutaneous enoxaparin followed by warfarin (INR target range 2.0–3.0), for a total duration of 6 months. Apixaban showed similar efficacy compared with warfarin, and the primary outcome of recurrent symptomatic VTE and VTE-related death occurred in 2.3% and 2.7%, respectively (relative risk [RR] 0.84, 95% CI 0.60–1.18). In addition, apixaban was associated with significantly less hemorrhagic complications, both major (0.6% vs 1.8%; RR 0.31, 95% CI 0.17–0.55) and major or clinically relevant nonmajor bleeding (4.3% vs 9.7%; RR 0.44, 95% CI 0.36–0.55).
Edoxaban was evaluated in the Hokusai-VTE trial, a double-blind double-dummy trial in which 8292 patients with acute VTE, initially treated with enoxaparin or UFH, were randomized to edoxaban 60 mg OD or warfarin, dose adjusted in order to maintain the target INR 2.0 to 3.0. The dose of edoxaban was reduced to 30 mg OD in the case of creatinine clearance 30 to 50 mL/min, body weight less than 60 kg, or concomitant treatment with potent P-gp inhibitors. The primary efficacy outcome was recurrent VTE or VTE-related death, and it was evaluated at the end of the whole 12-month study period, regardless of treatment duration. Edoxaban was noninferior to warfarin in the primary efficacy outcome, which occurred in 3.2% versus 3.5% (HR 0.98, 95% CI 0.70–1.13). The respective rates during the on-treatment period were 1.6% versus 1.9% (HR 0.82, 95% CI 0.60–1.14). Edoxaban showed a trend toward less major bleeding complications (1.4% vs 1.6%; HR 0.84, 95% CI 0.59–1.21) and was associated with lower rates of the composite safety outcome of major or clinically relevant bleeding (8.5% vs 10.3%; HR 0.81, 95% CI 0.71–0.94).
The results of the pivotal randomized controlled trials for the treatment of acute VTE with the DOACs are summarized in Fig. 1 .
Several systematic reviews and meta-analyses pooled the results of these randomized controlled trials. Compared with the standard regimen (LMWH followed by VKA), the DOACs were confirmed to be noninferior in terms of efficacy and showed a more favorable safety profile. The RR of major bleeding with the DOACs was approximately two-thirds of heparin/VKA, while the risk of fatal and intracranial bleeding was approximately one-third. Although a trend toward more gastrointestinal bleeding with the DOACs was observed in trials conducted in patients with atrial fibrillation, the rate of major gastrointestinal bleeding did not appear to be increased in patients with acute VTE. Indeed, the overall number of gastrointestinal bleeding in VTE trials was smaller, and the baseline characteristics of the population were different (eg, younger age and lower prevalence of concomitant antiplatelet therapy). Finally, the rate of clinically relevant nonmajor bleeding was also slightly reduced with the DOACs.
Extended treatment of venous thromboembolism
Several randomized controlled trials evaluated the DOACs for the extended treatment of VTE. Most of them compared the DOACs with placebo and aimed to demonstrate the superior efficacy of the active treatment in patients with clinical equipoise regarding the maintenance or discontinuation of the anticoagulant treatment. Only one compared a DOAC, dabigatran, with warfarin.
In the RE-MEDY trial, 2866 patients who had completed at least 3 months of anticoagulant treatment were randomized to dabigatran 150 mg BID or warfarin (INR target range 2.0–3.0). The incidence of the primary endpoint of recurrent or fatal VTE was similar in the 2 groups (1.8% vs 1.3%, respectively; HR 1.44, 95% CI 0.78–2.64). Dabigatran showed a tendency toward a safer profile, with regards to major bleeding (0.9% vs 1.8%; HR 0.52, 95% CI 0.27–1.02) and the composite outcome of major or clinically relevant bleeding (5.6% vs 10.2%; HR 0.54, 95% CI 0.41–0.71). However, more acute coronary syndromes were reported with the use of dabigatran (0.9% vs 0.2%), a finding that emerged also in studies evaluating patients with atrial fibrillation. In the RE-SONATE trial, 1353 patients were randomized to dabigatran or placebo. Dabigatran met the criterion for superior efficacy in the primary outcome, a composite of recurrent or fatal VTE or unexplained death, which occurred in 0.4% and 5.6% of patients, respectively (HR 0.08, 95% CI 0.02–0.25, P <.001). As expected, major or clinically relevant bleeding was higher with dabigatran (5.3% vs 1.8%; HR 2.92, 95% CI 1.52–5.60), although the actual number of major bleeding events was small (2 vs 0 patients, respectively).
The EINSTEIN-Extension trial evaluated rivaroxaban 20 mg OD compared with placebo in 1197 patients who had completed 6 to 12 months of acute treatment of VTE. Rivaroxaban was superior to placebo in the primary outcome of recurrent fatal or nonfatal VTE (1.3% vs 7.1%; HR 0.18, 95% CI 0.09–0.39). Major or clinically relevant bleeding occurred in 6.0% versus 1.2%, respectively (HR 5.19, 95% CI 2.3–11.7), whereas major bleeding occurred in 4 patients receiving rivaroxaban (0.7%) and 0 patients receiving placebo. Most of the clinically relevant nonmajor bleeding events were from mucosal sites and did not requires permanent discontinuation of anticoagulant treatment. A lower dose of rivaroxaban (10 mg OD) for the extended treatment of VTE is currently being evaluated in the EINSTEIN-CHOICE trial, in comparison with the approved dose of rivaroxaban (20 mg OD) and with aspirin 100 mg daily.
The AMPLIFY-EXT trial evaluated 2 doses of apixaban (2.5 mg and 5 mg BID) compared with placebo in 2486 patients who had completed 6 to 12 months of anticoagulant treatment. In this trial, the primary efficacy outcome was a composite of recurrent VTE and all-cause mortality and was significantly reduced with both dosages of apixaban (3.8% vs 11.6% for apixaban 2.5 mg BID and placebo, respectively, RR 0.33, 95% CI 0.22–0.48; and 4.2% vs 11.6% for apixaban 5 mg BID and placebo, respectively, RR 0.36, 95% CI 0.25–0.53). Furthermore, apixaban also reduced the rate of recurrent VTE or VTE-related death (1.7% vs 8.8% for apixaban 2.5 mg BID and placebo, respectively, RR 0.19, 95% CI 0.11–0.33; and 1.7% vs 8.8% for apixaban 5 mg BID and placebo, RR 0.20, 95% CI 0.11–0.34). No difference in efficacy emerged between the 2 apixaban dosages. The rate of major bleeding was not increased with apixaban (0.2% vs 0.5% for apixaban 2.5 mg BID and placebo, respectively, RR 0.49, 95% CI 0.09–2.64; and 0.1% vs 0.5% for apixaban 5 mg BID and placebo, respectively, RR 0.25, 95% CI 0.03–2.24). Conversely, the composite safety outcome of major or clinically relevant bleeding showed a trend toward increased hemorrhagic risk with the higher dose of apixaban (2.7% in the placebo group, 3.2% in the apixaban 2.5 mg BID, and 4.3% in the apixaban 5 mg BID; RR 1.20, 95% CI 0.69–2.10, for the comparison apixaban 2.5 mg BID vs placebo; RR 1.62, 95% CI 0.96–2.73, for the comparison apixaban 5 mg BID vs placebo; and RR 0.74, 95% CI 0.46–1.22, for the comparison apixaban 2.5 mg BID vs 5 mg BID).
The results of the pivotal randomized controlled trials for the extended treatment of VTE with the DOACs compared with placebo are summarized in Fig. 2 . When the results of these 3 randomized controlled trials were pooled, recurrent VTE or VTE-related death occurred in 1.3% of patients receiving DOACs versus 7.3% of patients receiving placebo (odds ratio [OR] 0.16, 95% CI 0.11–0.24; number needed to treat 17), whereas major bleeding events occurred in 0.3% and 0.2%, respectively (OR 1.87, 95% CI 0.19–17.96). However, the rate of major or clinically relevant bleeding was significantly increased with the DOACs (4.6% vs 2.0%; OR 2.69, 95% CI 1.25–5.77; number needed to harm 39).