Fig. 1
As the incident wave bounces back and forth between surfaces A and B (yellow arrows), the returning waves are perceived by the probe as returning from reflectors progressively further from the probe face (long red arrows)
This type of artifact is quite common in transrectal scanning of the prostate and often arises from air trapping in the covering used to protect the probe (Fig. 2). It may also arise from gas in the rectum itself.
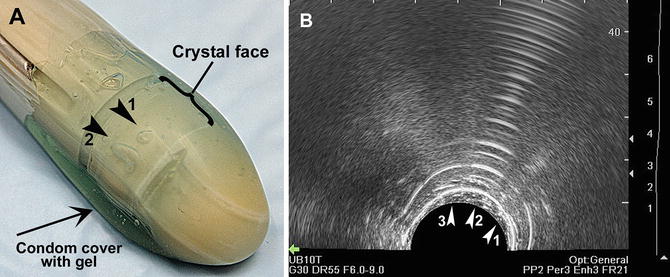
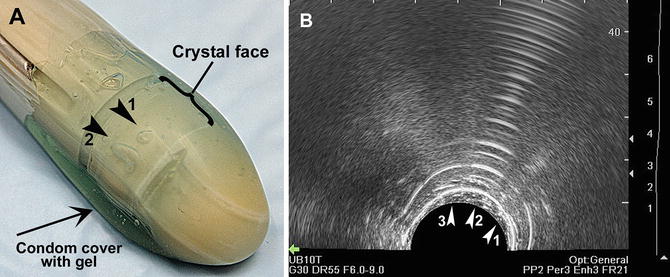
Fig. 2
A biplane probe with air bubbles overlying the transverse crystal (arrowheads 1 and 2 in image a). Arrowhead 1 in image (a) designates a bubble against the crystal surface. This produces a closely spaced reverberation artifact (Arrowhead 1 in image b). Arrowhead 2 in Image (a) designates a bubble trapped beneath the probe cover. This produces a more hyperechoic and widely spaced reverberation artifact (arrowhead 2 in image b). Arrowhead 3 in image (b) represents the gel between the condom cover and the crystal face
In scanning the prostate, the air bubble produces an artifact that may obscure distal anatomy (Fig. 3). This type of artifact can often be corrected by gently pressing the probe against the rectal wall to force the gas away from the crystal face. If that does not work, the probe should be removed and the condom cover re-prepared. Copious gel should be applied to help minimize air between the covering and the probe. Gas or stool in the rectum may also cause this artifact and does not usually respond to probe repositioning. In this circumstance, removing the probe and using a gloved finger to clear the gas and stool can be tried. Another type of reverberation artifact occurs when an ultrasound wave strikes gas and stool in the small intestine (Fig. 4).
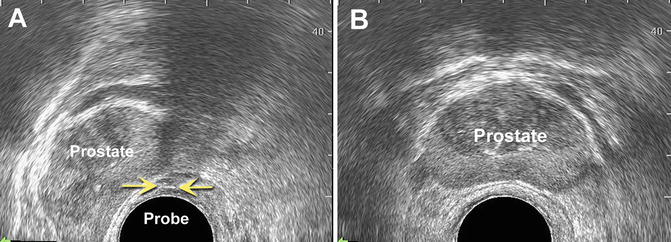
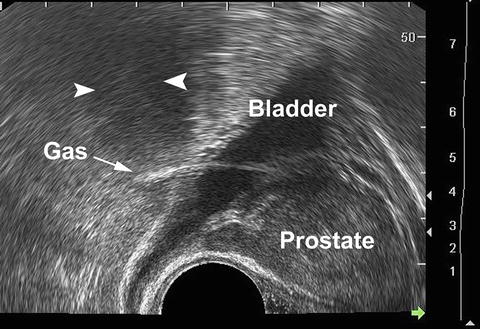
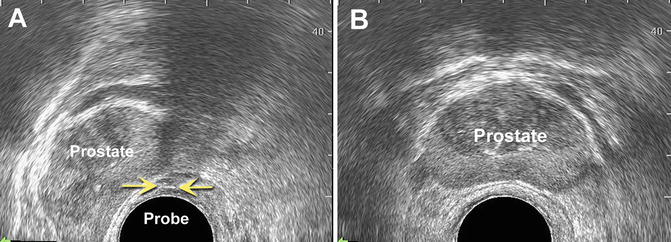
Fig. 3
(a) Reverberation artifact caused by air bubble trapped between probe crystal and probe cover resulting in a reverberation artifact (yellow arrows). If the probe is rotated within the rectum this artifact will remain. However, if air is trapped between the probe cover and the rectal wall the artifact will resolve with rotation or change in probe position. (b) Same prostate after the air bubble removed
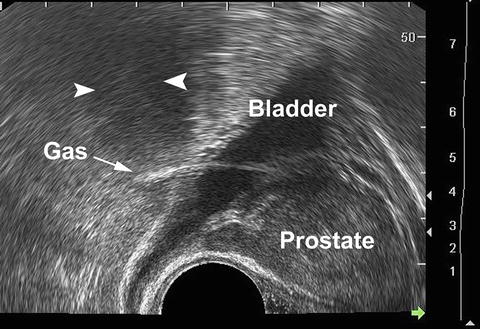
Fig. 4
Reverberation artifact caused by small intestine containing gas in the cul-de-sac posterior to the bladder on this sagittal view of the prostate causes acoustic shadowing (arrowheads) distally because of attenuation
Reverberation artifacts may also be seen when ultrasound waves strike any specular reflector. Examples of such reflectors in the prostate include needles, fiducial markers, and radioactive seeds (Fig. 5). This characteristic artifact is the result of reverberation of the waves between the leading and trailing edges of the structure. That is, for example, the wave strikes the front edge of a hollow needle and bounces back and forth between the front and back edge producing a distal artifact of diminishing echogenicity but equal distance from the needle (Fig. 5a, b). Similar patterns are seen for fiducial markers and seeds (Fig. 5c).
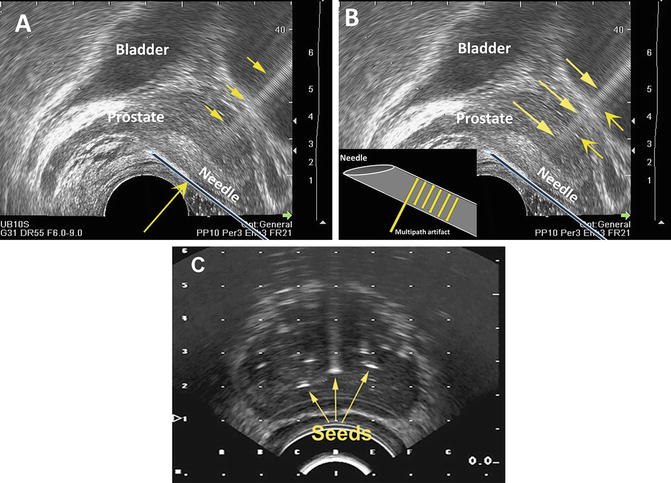
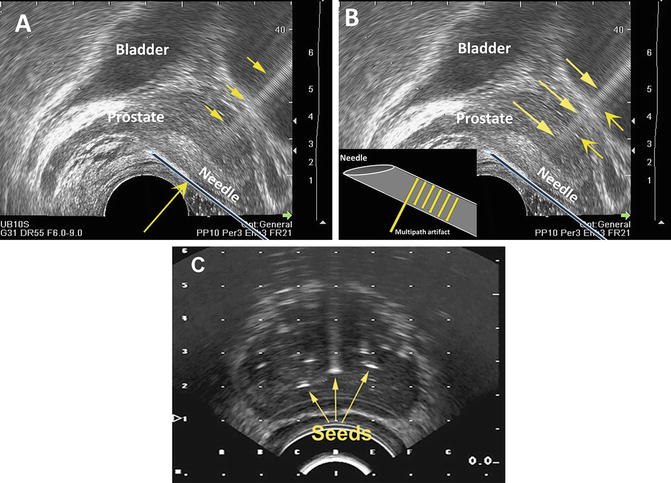
Fig. 5
Specular reflectors have a flat smooth surface. (a) Although sound waves strike the surface of the needle along its entire length, the reverberation artifact (white arrows) is most pronounced when the incident wave (yellow arrows) strikes perpendicular to the object. The inset in (b) shows the multipath artifact within the needle (white arrows). (c) Radioactive seeds also serve as specular reflectors in an ultrasound field. The reverberation artifact is most prominent when the incident wave strikes perpendicular to the reflector
Compression Artifacts
Although compression does not technically produce an artifact (based on our original definition of artifact) it can cause distortions of anatomy and changes in echogenicity and blood flow. As such, compression may cause the sonographer to “misinterpret” the nature of the anatomic structure being interrogated. For example, when the transrectal probe is pressed against the rectal wall it may deform the underlying prostate capsule and peripheral zone of the prostate, producing asymmetry and hypoechogenicity (Fig. 6).
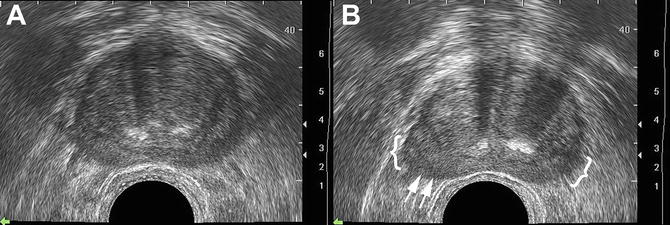
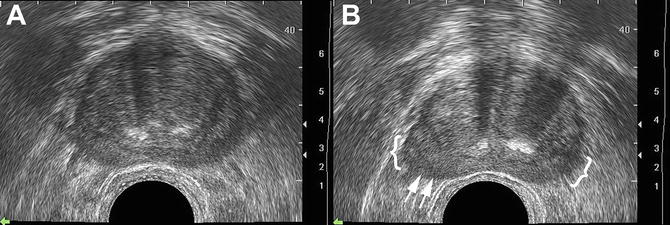
Fig. 6
A transverse ultrasound of the prostate with no compression (a). The same gland with compression of the rectal wall and prostate demonstrates capsular deformity (arrows) and induced hypoechogenicity (brackets) ( b)
Similarly, blood flow may be affected by the amount of force exerted against the rectal wall by the probe. Blood flow in the neurovascular bundle as well as the peripheral zone of the prostate may be diminished by probe pressure (Fig. 7).
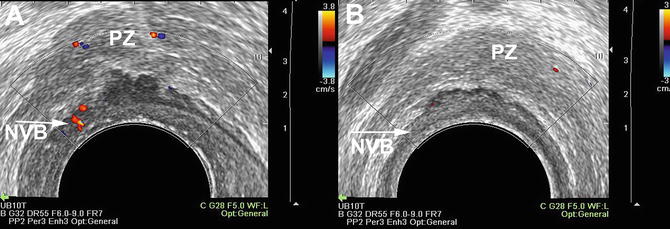
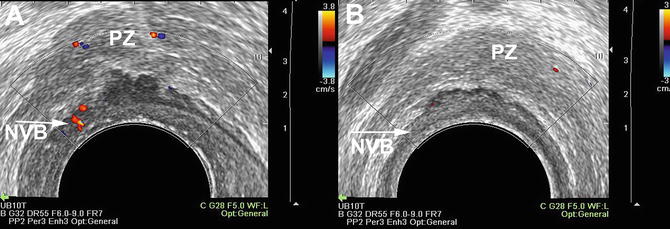
Fig. 7




(a) Normal blood flow on a transverse ultrasound of the prostate showing the expected flow in the peripheral zone (PZ) and the left neurovascular bundle (NVB). (b) Compression of the same prostate on the left side by a probe results in less demonstrated flow in the peripheral zone and left neurovascular bundle
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree