The molecular linkage between ultralarge (UL) von Willebrand factor (VWF) multimers and the alternative complement pathway (AP) has recently been described. Endothelial cell (EC)-secreted and anchored ULVWF multimers (in long stringlike structures) function as both hyperadhesive sites that initiate platelet adhesion and aggregation and activating surfaces for the AP. In vitro, the active form of C3, C3b binds to the EC-anchored ULVWF multimeric strings and initiates the assembly on the strings of C3 convertase (C3bBb) and C5 convertase (C3bBbC3b). In vivo, activation of the AP via this mechanism proceeds all the way to generation of terminal complement complexes (C5b-9).
Key points
- •
The molecular linkage between ultralarge (UL) von Willebrand factor (VWF) multimers and the alternative complement pathway (AP) has recently been described.
- •
Endothelial cell (EC)-secreted and anchored ULVWF multimers (in long stringlike structures) function as both hyperadhesive sites that initiate platelet adhesion and aggregation and activating surfaces for the AP.
- •
In vitro, the active form of C3, C3b binds to the EC-anchored ULVWF multimeric strings and initiates the assembly on the strings of C3 convertase (C3bBb) and C5 convertase (C3bBbC3b).
- •
In vivo, activation of the AP via this mechanism proceeds all the way to generation of terminal complement complexes (C5b-9).
- •
The linkage of EC-secreted and anchored ULVWF multimeric strings, excessive platelet adhesion/aggregation, and activation of the AP explains many of the clinical similarities among (1) severe ADAMTS-13 (a disintegrin and metalloprotease with thrombospondin domains, #13)-deficient thrombotic thrombocytopenic purpura (TTP); (2) TTP-like syndromes associated with only modest deficiencies of ADAMTS-13; (3) enterohemorrhagic Escherichia coli– associated hemolytic-uremic syndrome; and (4) the provocation of episodes of atypical HUS, which are associated with overactivation of the AP.
Thrombotic microangiopathies (TMAs)
Common clinical characteristics of the thrombotic microangiopathies, thrombotic thrombocytopenic purpura (TTP), hemolytic-uremic syndromes associated with enterohemorrhagic Escherichia coli (EHEC-HUS), and atypical hemolytic-uremic syndrome (aHUS), include microvascular platelet adhesion/aggregation, thrombocytopenia, and erythrocyte fragmentation. Excessive platelet adhesion/aggregation and activation of the alternative complement pathway (AP) on endothelial cells (EC)-secreted/anchored ultralarge (UL) von Willebrand factor (ULVWF) multimeric strings are involved in all of these syndromes.
Recent studies have demonstrated the precise molecular linkage between EC-secreted/anchored ULVWF multimers and activation of the alternative AP. This linkage is likely to be of considerable clinical importance in the thrombotic microangiopathies, including TTP and the EHEC-HUS or with overactivation of the AP (aHUS).
Thrombotic microangiopathies (TMAs)
Common clinical characteristics of the thrombotic microangiopathies, thrombotic thrombocytopenic purpura (TTP), hemolytic-uremic syndromes associated with enterohemorrhagic Escherichia coli (EHEC-HUS), and atypical hemolytic-uremic syndrome (aHUS), include microvascular platelet adhesion/aggregation, thrombocytopenia, and erythrocyte fragmentation. Excessive platelet adhesion/aggregation and activation of the alternative complement pathway (AP) on endothelial cells (EC)-secreted/anchored ultralarge (UL) von Willebrand factor (ULVWF) multimeric strings are involved in all of these syndromes.
Recent studies have demonstrated the precise molecular linkage between EC-secreted/anchored ULVWF multimers and activation of the alternative AP. This linkage is likely to be of considerable clinical importance in the thrombotic microangiopathies, including TTP and the EHEC-HUS or with overactivation of the AP (aHUS).
Overview of the thrombotic microangiopathies
A Disintegrin and Metalloprotease with Thrombospondin Domains, #13-Deficient Thrombotic Thrombocytopenic Purpura
During hemostasis and thrombosis, stimulated human vascular ECs secrete and anchor ULVWF multimers in hyperadhesive long stringlike structures that initiate platelet adhesion. Severe TTP is usually associated with less than 10% of plasma ADAMTS-13 (a disintegrin and metalloproteinase with a thrombospondin type-1 motif, member #13), the Ca 2+ /Zn 2+ -metalloprotease responsible for cleaving EC-secreted/anchored ULVWF multimeric strings. Severe ADAMTS-13 deficiency is caused by congenital homozygous or double-heterozygous ADAMTS13 gene mutations, or by the acquired production of polyclonal autoantibodies directed against the spacer domain of the metalloprotease. The result is little or no cleavage of EC-secreted/anchored ULVWF multimeric strings, excessive platelet adhesion/aggregation on the uncleaved hyperadhesive strings, and the formation of microvascular thrombi ( Figs. 1 and 2 A, B ).
More modest deficiencies of ADAMTS-13 may also result in platelet adhesion/aggregation greater than normal in other thrombotic microangiopathies, as described in the sections to follow and depicted in Fig. 2 C.
Enterohemorrhagic Escherichia coli–Associated Hemolytic-Uremic Syndrome
HUS is a leading cause of acute renal failure in children. Most commonly, these HUS cases are associated with inadvertent ingestion of enterohemorrhagic E coli and are characterized by episodes of bloody diarrhea followed by the formation of occlusive glomerular platelet-fibrin thrombi.
EHEC-HUS can also be acquired by ingestion of Shigella dysenteriae serotype 1, which is the prototype Shiga toxin microbe. More frequently, however, the causative organisms belong to one of several strains of enterohemorrhagic E coli (eg, O157:H7; or 0104:H4 [in the 2011 European outbreak]). These E coli strains produce Shiga-like toxin-1 (Stx-1) or Shiga-like toxin-2 (Stx-2). These Shiga toxins are 70-kDa exotoxins, composed of 5 B subunits (7.7 kDa each) and an A subunit (composed of disulfide bonded chains of 28 and 4 kDa). The B subunit mediates attachment and cellular entry through a membrane globotriaosylceramide receptor (Gb3 or CD77) present on ECs—and especially abundant on renal glomerular microvascular ECs. The A subunit is internalized and inhibits protein synthesis.
Atypical Hemolytic-Uremic Syndrome
aHUS is a complication of excessive AP activation. Prominent causes of aHUS are a heterozygous mutation of the complement factor H ( CFH ) gene on chromosome 1; or homozygous deletion in genes for the CFH-related (CFHR)-1 and CFHR-3 proteins of the CFH gene cluster (chromosome 1) plus autoantibody-mediated inhibition of FH (deficiency of CFHR plasma proteins and autoantibody-positive HUS). Other mutations associated with aHUS include heterozygous loss-of-function mutations in complement factor I ( CFI , chromosome 4), in CD46 (membrane cofactor protein; chromosome 1), or in THBD (thrombomodulin or CD141; chromosome 20). Heterozygous gain-of-function mutations in the C3 gene (chromosome 19) or in the complement factor B gene ( CFB ; chromosome 6) have been associated with aHUS. Excessive AP activity in aHUS results in damage or perturbation of renal ECs, resulting in episodes of acute renal failure.
Overview of the alternative complement pathway
The initiation of the AP requires an “activating surface” to cleave and activate C3 to C3b. The process of C3 cleavage generates C3a fragments (∼9 kDa) with histamine-releasing and chemotactic activities. C3b attaches covalently via a cleavage-exposed thioester to carbohydrates or hydroxyl-containing amino acids (threonine, serine, and tyrosine) on activating surfaces. Bound C3b then binds factor B (FB) to produce C3bB. The FB in the C3bB complex is cleaved by factor D (FD) to form C3bBb, the AP C3 convertase that is stabilized by factor P (FP). The Bb in C3bBb on an activating surface cleaves fluid-phase C3 to generate additional surface-bound C3b molecules and rapidly amplify the generation of C3b generation from C3. As the ratio of C3b to Bb increases, C3bBbC3b (the C5 convertase) is formed. C5 convertase binds C5 with high affinity and cleaves/activates C5 to C5b, releasing the peptide fragment, C5a (∼10 kDa). C5a is similar to C3a in also possessing histamine-releasing and chemotactic activity.
Ultralarge von Willebrand factor multimers and initiation of the alternative complement pathway
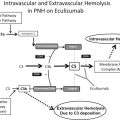
It has been recently discovered that AP initiation occurs on ULVWF multimeric strings that have been secreted by, and are anchored to, the surfaces of stimulated ECs. Human umbilical vein endothelial cells (HUVECs) and other ECs are miniature “factories” that express the mRNA for complement components and synthesize the associated proteins. In these in vitro experiments, there was no requirement for the addition of any additional purified components. Uncleaved ULVWF multimeric strings secreted by, and anchored to, stimulated ECs were found to be “activating surfaces” for C3b binding and AP assembly and activation ( Fig. 3 A, Table 1 ). C3 (as C3b), FB (as Bb), FD, FP, and C5 (as C5b), FH, and FI attached to EC-secreted and anchored ULVWF strings. In contrast, C4 (as C4b) did not attach to the ULVWF strings, indicating that the classical and lectin pathways were not activated (see Fig 3 B, see Table 1 ). The attachment to EC-secreted/anchored ULVWF strings of C3b, Bb, and C5b occurred in quantitative and functional patterns consistent with the assembly of AP components into active complexes of C3 convertase (C3bBb) and C5 convertase (C3bBbC3b) ( Fig. 4 A).
| Complement Component | Mean Intensities ± SD |
|---|---|
| C3 | 4186 ± 2452 |
| FB | 1675 ± 645 |
| FD | 1013 ± 631 |
| FP | 913 ± 1067 |
| C5 | 3128 ± 2087 |
| FH | 2262 ± 1385 |
| FI | 2581 ± 1710 |
| C4* | 31 ± 32 |
The AP negative regulatory components, FH and FI, also bind to EC-secreted/anchored ULVWF strings. The extent of their binding is, however, about one-third less than the binding of C3b (see Table 1 ). FH and FI may, therefore, slow, but not prevent, EC-anchored ULVWF multimeric strings from gating C3 and C5 convertases.
These experiments established the molecular linkage between the AP and the earliest events in hemostasis-thrombosis (ie, the stimulation of vascular ECs to secrete and anchor ULVWF multimeric strings). In the in vitro studies summarized above, the AP was assembled and activated on ULVWF strings that were not rapidly cleaved because of inadequate ADAMTS-13 in the model system. Inflammatory cytokines, bacterial toxins, phosphodiesterase inhibitors, calcium ionophore, and high concentrations of histamine are examples of agents that can cause EC stimulation and increase rates of EC secretion/anchorage of ULVWF strings in vitro. Inflammatory cytokines also have this effect in vivo. If the secretion/anchorage of ULVWF strings at accelerated rates by stimulated ECs (as during the increased cytokine generation with microbial infection or pregnancy) is associated with a reduced level of ADAMTS-13, then excessive numbers of EC-anchored ULVWF strings will form and persist transiently (ie, at least for a few minutes), leading to prolonged AP activation.
Generation of terminal complement complexes
In addition to the complement components that participate in initiation and amplification of the AP, HUVECs and other ECs also synthesize the later-acting terminal pathway (TP) components C6, C7, C8, and C9 (see Fig. 4 B). HUVEC expression of mRNA for each TP component has been detected, although only soluble C7 protein (∼20 ng/10 6 cells) was successfully measured in studies during the early years of this century. C7 was also shown not to be primarily synthesized by hepatocytes and not to be an acute phase reactant. ECs may only express and produce low levels of TP (and other complement) components; however, the human vascular system has an immense quantity of ECs (>10 13 in adults) capable of contributing a considerable portion of each complement protein in circulation.
Active C3 convertase (C3bBb) and C5 convertase (C3bBbC3b) complexes assemble on uncleaved EC-anchored ULVWF strings. C5 convertase generates C5b that can be detected on the ULVWF strings. In our in vitro experiments conducted so far using human ECs, the fluid phase volumes and antibody sensitivities were insufficient to enable the determination if C5b-9 complexes are formed on the EC-anchored ULVWF strings, in the soluble phase, or as complexes inserted into EC membranes. We suspect that C5b molecules generated on the EC-secreted/anchored ULVWF strings combine with soluble C6 and C7 molecules to form C5b-7 complexes that dissociate from the ULVWF strings, escape into the fluid phase, and insert into nearby cell membranes. C8 and multiple C9 molecules may then combine with membrane-imbedded C5b-7 to form C5b-9 complexes. These complexes are even more likely if cells are damaged and deficient in CD59 (which impairs additional C9 molecules from binding to the initial C9 in membrane C5b-9 complexes) (see Fig. 4 B). Measurement of C5b-9 complexes in the plasma of patients with thrombotic microangiopathies supports the probability that the AP is activated to completion in vivo in ADAMTS-13-deficient TTP, EHEC-HUS, and aHUS.
As long as EC-anchored ULVWF strings remain uncleaved, the strings will promote platelet adhesion/aggregation, microvascular thrombosis, and AP assembly-activation. It is likely that cleavage fragments C3a and C5a, both chemotactic and histamine-releasing compounds in an inflammatory response, will be generated (see Fig. 4 ). Possible targets in normal host defense for the lytic C5b-9 complexes generated by activation of the AP on EC secreted/anchored ULVWF strings include potentially harmful microbes or injured/defective cells. C5b-9 complexes inserted into membranes of damaged or defective ECs may also promote the influx of Ca 2+ and the secretion of additional ULVWF multimeric strings from EC Weibel-Palade bodies, and ULVWF string anchorage, to EC surfaces.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree