Fig. 22.1
(a, b) Preset outer-layer U-sutures (three to four sutures) without tying for posterior horizontal mattress sutures on the jejunum
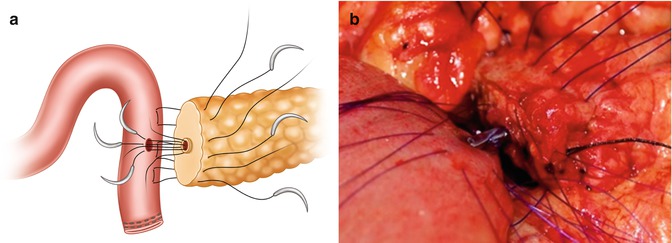
Fig. 22.2
(a, b) Preset inner-layer sutures (six to eight sutures) without tying for duct-to-mucosa anastomosis using pair-watch suturing technique
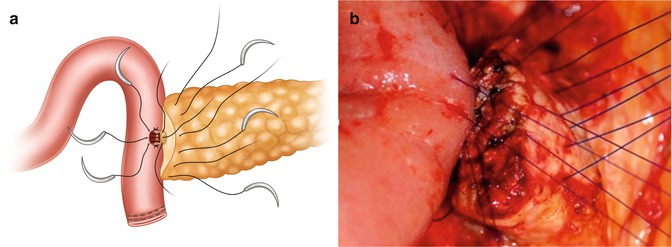
Fig. 22.3
(a, b) Preset inner-layer sutures (six to eight sutures) with partial tying for duct-to-mucosa anastomosis
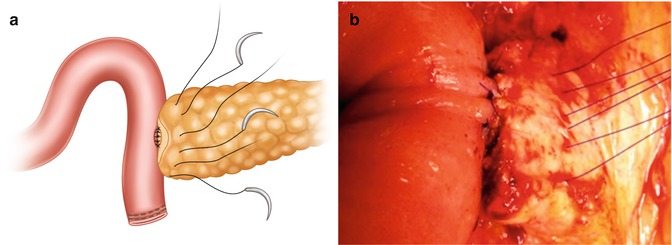
Fig. 22.4
(a, b) Inner-layer sutures with complete tying for duct-to-mucosa anastomosis
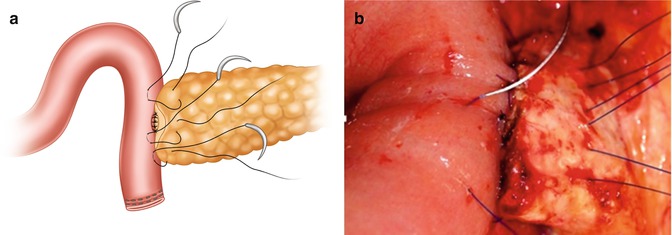
Fig. 22.5
(a, b) Outer-layer U-suturing for anterior horizontal mattress sutures on the jejunum
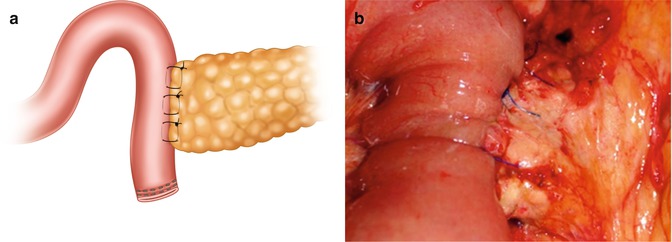
Fig. 22.6
(a, b) Completed outer-layer U-suturing with tying for anterior horizontal mattress sutures on the jejunum
22.1.4 Pancreatic Fistula After Pancreatic Reconstructions
POPF has been the leading cause of postoperative morbidity and mortality after PD. The severity of POPF is classified into grades A, B, and C based on the definition of the International Study Group on Pancreatic Fistula (ISGPF) [18]. Grades B and C are clinically relevant postoperative pancreatic fistula (CR-POPF), and grade A is biochemical leakage without clinically relevance. PG has been claimed to be a better pancreatic reconstruction in reducing the incidence and severity of CR-POPF by most retrospective studies [4, 5, 16, 19]. However, not all of the published randomized controlled trials confirm the superiority of PG (Table 22.1). In recent meta-analysis of published randomized controlled trials, PG has been shown to be associated with lower rate of CR-POPF as compared with classic PJ (Table 22.2). PG had been the procedure of choice for pancreatic reconstruction at the author institute since 1997 [4]. In 2012, the modified Blumgart PJ began to be adopted at our institute and has replaced PG as the technique of choice for pancreatic reconstruction after PD thereafter. With the modified Blumgart PJ, only a 1- to 2-cm free pancreatic stump is needed, as opposed to a 3- to 4-cm free pancreatic stump for PG reconstruction. Moreover, only three or four transpancreatic U-sutures are used for the modified Blumgart PJ, instead of the multiple tangential sutures needed for PG or classic PJ. Blumgart PJ has been reported to decrease the CR-POPF rate to 4.3–6.9%, significantly lower than the 10–20% of other techniques (Table 22.3) [8, 9, 11, 14]. Based on our matched historical control study [33], the modified Blumgart PJ appears to be superior to PG in reducing the incidence and severity of CR-POPF. The modified Blumgart PJ can therefore be recommended as a fast, simple, and safe alternative for pancreatic reconstruction after PD.
Table 22.1
Randomized controlled trials for clinically relevant postoperative pancreatic fistula (CR-POPF) after pancreaticoduodenectomy
CR-POPF | |||||
|---|---|---|---|---|---|
Year | n | PGa | PJb | P value | |
2015 | PG = 149 PJ = 171 | 20% | 22% | NSc | |
Nakeeb et al. [21] | 2014 | PG = 45 PJ = 45 | 15.6% | 8.9% | NSc |
Topal et al. [22] | 2013 | PG = 162 PJ = 167 | 8.0% | 19.8% | 0.002 |
Figueras et al. [23] | 2013 | PG = 65 PJ = 58 | 11% | 33% | 0.006 |
Wellner et al. [24] | 2012 | PG = 59 PJ = 57 | 11% | 33% | NSc |
Fernandez-Cruz et al. [25] | 2008 | PG = 53 PJ = 55 | 4% | 18% | <0.01 |
Duffas et al. [26] | 2005 | PG = 81 PJ = 68 | 16% | 20% | NSc |
Bassi et al. [27] | 2005 | PG = 69 PJ = 51 | 13% | 16% | NSc |
Yeo et al. [28] | 1995 | PG = 73 PJ = 72 | 12.3% | 11.1% | NSc |
Table 22.2
Meta-analysis of randomized controlled trials for clinically relevant postoperative pancreatic fistula (CR-POPF) after pancreaticoduodenectomy
Year | n | PGa | PJb | P value | |
|---|---|---|---|---|---|
Menahem et al. [29] | 2015 | PG = 562 PJ = 559 | 11.2% | 18.7% | 0.0003 |
Hallet et al. [30] | 2015 | PG = 339 PJ = 337 | 8% | 20% | <0.0001 |
Que et al. [31] | 2015 | PG = 384 PJ = 382 | 9.1% | 16.5%
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|