Induction regimens containing a proteasome inhibitor and/or immunomodulatory agent with dexamethasone result in rapid disease control before autologous stem cell transplantation (ASCT). ASCT followed by consolidation and/or maintenance further improves depth of response following effective induction. Overall survival of transplant-eligible patients has been extended with modern therapeutic strategies. The optimal timing of ASCT and methods to prevent relapse following ASCT are under active investigation. Different patient populations may benefit differentially from currently available treatments.
Key points
- •
Induction regimens containing a proteasome inhibitor and/or immunomodulatory agent with dexamethasone result in rapid disease control before autologous stem cell transplantation (ASCT).
- •
ASCT followed by consolidation and/or maintenance further improves depth of response following effective induction.
- •
Overall survival of transplant-eligible patients has been extended with modern therapeutic strategies.
- •
The optimal timing of ASCT and methods to prevent relapse following ASCT are under active investigation.
- •
Different patient populations may benefit differentially from currently available treatments.
Introduction
High-dose melphalan therapy (HDT) with autologous stem cell transplant (ASCT) has been an integral component of myeloma therapy for close to 3 decades after McElwain and Powles demonstrated the clinical relevance of melphalan dose and disease response in patients with relapsed and refractory disease. These results led to the exploration of HDT-ASCT as consolidation of initial remission in newly diagnosed multiple myeloma (MM). Compared with conventional chemotherapy, HDT and ASCT were associated with improved outcomes including event-free, progression-free (PFS), and overall survival (OS). Depth of response, particularly achievement of a complete response (CR), was associated with longer PFS and OS in MM and was likely responsible for the initial success of HDT and SCT.
Novel induction regimens incorporating proteasome inhibitors (bortezomib and carfilzomib) and the immunomodulatory drugs (IMIDs) (thalidomide and lenalidomide) have demonstrated very high CR rates that compare to those produced with HDT and ASCT. Proteasome inhibitors and IMIDs have changed the context in which patients are receiving HDT and ASCT. Ongoing studies are investigating in transplant-eligible patients whether HDT is required early in the course of the disease or can be used as salvage therapy. In patients who received alkylator-based induction, early ASCT was associated with better quality-of-life (QOL) parameters such as time without symptoms and therapy-related toxicity. As myeloma therapy evolves to include post-ASCT consolidation and maintenance, it will be important to incorporate QOL measurements into the current studies. Herein the authors describe the treatment of newly diagnosed transplant-eligible MM patients based on currently available data and highlight important studies that will instruct us as the field continues to move forward.
Introduction
High-dose melphalan therapy (HDT) with autologous stem cell transplant (ASCT) has been an integral component of myeloma therapy for close to 3 decades after McElwain and Powles demonstrated the clinical relevance of melphalan dose and disease response in patients with relapsed and refractory disease. These results led to the exploration of HDT-ASCT as consolidation of initial remission in newly diagnosed multiple myeloma (MM). Compared with conventional chemotherapy, HDT and ASCT were associated with improved outcomes including event-free, progression-free (PFS), and overall survival (OS). Depth of response, particularly achievement of a complete response (CR), was associated with longer PFS and OS in MM and was likely responsible for the initial success of HDT and SCT.
Novel induction regimens incorporating proteasome inhibitors (bortezomib and carfilzomib) and the immunomodulatory drugs (IMIDs) (thalidomide and lenalidomide) have demonstrated very high CR rates that compare to those produced with HDT and ASCT. Proteasome inhibitors and IMIDs have changed the context in which patients are receiving HDT and ASCT. Ongoing studies are investigating in transplant-eligible patients whether HDT is required early in the course of the disease or can be used as salvage therapy. In patients who received alkylator-based induction, early ASCT was associated with better quality-of-life (QOL) parameters such as time without symptoms and therapy-related toxicity. As myeloma therapy evolves to include post-ASCT consolidation and maintenance, it will be important to incorporate QOL measurements into the current studies. Herein the authors describe the treatment of newly diagnosed transplant-eligible MM patients based on currently available data and highlight important studies that will instruct us as the field continues to move forward.
Defining an optimal induction regimen
Response before SCT has been shown to improve outcomes, but the optimal type and duration of induction has not been well defined. In responding patients, treatment with a fixed number of induction cycles or treatment until best response is the common strategy. Randomized trials comparing conventional chemotherapy with a regimen that contains thalidomide, lenalidomide, and/or bortezomib along with corticosteroids have established that induction with an IMID, proteasome inhibitor, or both is the standard of care. Deeper and quicker responses are typically achieved with 3-drug regimens such as thalidomide-bortezomib-dexamethasone, cyclophosphamide-bortezomib-dexamethasone, bortezomib-adriamycin-dexamethasone, or lenalidomide-bortezomib-dexamethasone versus 2-drug regimens, thalidomide-dexamethasone, lenalidomide-dexamethasone, or bortezomib-dexamethasone (VD), although the impact on OS has not been established ( Table 1 ). Attempts to increase to a 4-drug regimen are associated with increased toxicity and no clear advantage over 3-drug regimens.
| Reference | Regimen | a ORR (%) | a CR (%) | Common Toxicities |
|---|---|---|---|---|
| VD | 79 | 15 | PN, GI toxicity, low PLTs | |
| TD | 79 | 11 | Constipation, sedation, PN | |
| b Ld | 70 | 4 | VTE, neutropenia | |
| VTD | 93 | 31 | PN, GI toxicity, infection | |
| RVD | 74 | 6 | PN, myelosuppression | |
| VCD | 96 | 46 | Myelosuppression |
a Response rates following 4 cycles (unless otherwise indicated).
Notably few randomized studies comparing modern induction regimens have been performed to date; and lenalidomide-based combinations have not been compared with either bortezomib- or thalidomide-based combinations. A trial of VD versus reduced-dose bortezomib-thalidomide-dexamethasone (VTD) as induction pre-SCT conducted by the Intergroupe Francophone du Myelome (IFM) did not suggest a benefit of the 3-drug combination over the 2-drug combination in terms of the frequency of CR after 4 cycles (13% and 12%, P = .74), which was their primary end point. However, higher very good partial response (VGPR) rates were noted with VTD compared with VD both before (49% vs 36%, P = .05) and after SCT (74% vs 58%, P = .02). In addition, lower doses of bortezomib and thalidomide in the 3-drug combination translated into less grade 2 or higher neuropathy compared with the 2-drug regimen (14% and 34%, P = .001). A randomized phase II study examined the efficacy and tolerability of bortezomib-dexamethasone combined with lenalidomide (VDR) or cyclophosphamide (VDC) as well as the 4-drug regimen bortezomib-dexamethasone-cyclophosphamide-lenalidomide (VDCR). After an interim analysis, VDC was modified (VDC-mod) to include 3 rather than 2 doses of cyclophosphamide based on results from a phase II trial investigating the same regimen. After 4 cycles, 33%, 32%, and 41% of patients receiving VDCR, VDR, or VDC-mod achieved VGPR or better, respectively. VDCR was associated with more toxicity leading the investigators to conclude that the VDR and VDC-mod regimens should be evaluated further. Ongoing randomized studies include the large randomized Southwest Oncology Group trial of lenalidomide and dexamethasone with or without bortezomib as initial therapy for untreated MM patients. The results of this trial will be instructive with respect to rate and depth of response as well as safety profiles. Indeed lenalidomide-dexamethasone has the benefit of being an oral regimen and is well tolerated.
Newer combinations include MLN-9708 (ixazomib), an oral proteasome inhibitor in combination with lenalidomide-dexamethasone, which is an entirely oral 3-drug regimen. Preliminary data were presented at the American Society of Hematology meeting in December 2013 and suggested promising activity in 64 previously untreated patients with an overall response rate of 93%, including 67% with at least a VGPR. On this study, SCT-eligible patients underwent stem cell collection after 4 cycles of induction without difficulty (Paul G. Richardson, unpublished data, 2013). Carfilzomib, a second generation proteasome inhibitor, has also been combined with lenalidomide-dexamethasone (CRD), and in 53 newly diagnosed patients with MM, 38% achieved at least a near CR (nCR) after 4 cycles. Stem cells were successfully collected in 34 of 35 patients but only 7 patients chose to undergo SCT after initial induction. The favorable toxicity profile of CRD, particularly the lack of neuropathy, allowed prolonged administration with deeper responses over time. However, carfilzomib is administered intravenously on days 1, 2, 8, 9, 15, and 16, which can be burdensome to patients.
Most but not all studies indicate that achieving CR is a surrogate for OS, although a patient’s risk category is likely to play a role. Patients with low-risk disease may not require CR for prolonged survival, whereas the goal for patients with high-risk disease is not only to achieve but sustain a CR. With the exception of using bortezomib-based treatment of patients with the t (4;14) abnormality, there is not sufficient data to support using specific therapy for patients in different risk groups. As molecular techniques evolve, the goal is to individualize therapy based on predictive markers that provide insight into the likelihood of response and/or toxicity to certain drugs or regimens.
Role of HDT and SCT
Based on superior outcomes when compared to conventional alkylator-based therapy, HDT and ASCT has become the standard approach to maximize response following an initial response to induction therapy. The unprecedented responses to initial therapy with IMIDs and proteasome inhibitors, especially in combination, have called into question the role of HDT and SCT in MM. Yet, even in the context of modern induction regimens where more than 90% respond, the quality of response continues to improve following HDT and PFS approaches or exceeds 3 years. Palumbo and colleagues have presented the preliminary results of a prospective phase III trial that randomized 402 patients to consolidation with oral melphalan-prednisone-lenalidomide (MPR) versus HDT after 4 cycles of induction with lenalidomide-dexamethasone (LD). With relatively short follow-up of 26 months, there is a significant PFS benefit for patients randomized to transplant compared with those who received MPR with 73% versus 54% (HR 0.506, P = .0002) PFS at 2 years, but no difference in OS. Similarly, following 4 cycles of LD induction, 195 patients randomized to HDT and SCT had longer PFS compared with 194 patients randomized to consolidation with cyclophosphamide-lenalidomide-dexamethasone (CRD) with respective 3 years PFS 60% versus 38% (HR 0.62, P = .003). After median follow-up of 31 months, there was no difference in OS. In contrast, among 53 newly diagnosed MM patients who received lenalidomide-bortezomib-dexamethasone (RVD) as initial therapy and had not progressed, a post-hoc landmark analysis at 1 year following treatment initiation showed no difference in PFS according to whether or not patients chose to pursue HDT and SCT ( P = .38) after at least 4 cycles of induction. The retrospective nature of the latter experience does not allow for conclusions to be drawn but has led to the Intergroup Francophone du Myeloma-Dana-Farber Cancer Institute (IFM-DFCI) study of RVD with or without HDT and SCT.
Two studies have suggested that 2 courses of high-dose melphalan are superior to a single SCT, but the benefit appears to be limited to patients who had not achieved VGPR after the first transplant. Neither of these studies included induction therapies with either an IMID or proteasome inhibitor and therefore, may not be relevant today. More recently, patients who received bortezomib-based induction therapy and either single or double SCT on European phase III trials were analyzed. In comparison with patients for whom a single SCT was planned by study design, those who were assigned to receive tandem SCT had significantly longer PFS (median: 38 vs 50 months, P <.001) and OS (5-year estimates: 63% vs 75%, P = .002). From this dataset, the benefit of tandem ASCT was greatest for patients with high-risk cytogenetics defined as t (4;14) and/or del 17p and also for those who had not attained CR following bortezomib-based induction. These data need to be confirmed by prospective, randomized phase III studies that are currently ongoing.
Fermand and colleagues reported in 1998 that patients who receive ASCT as consolidation of initial remission have similar survival to those who were assigned to transplant at the time of relapse. However, early ASCT was associated with more time without symptoms, less therapy-related toxicity, and better QOL parameters, favoring this approach. With more effective induction therapies that are relatively well tolerated, many patients and physicians have deferred HDT with ASCT. A landmark analysis of the E4AO3 trial that compared lenalidomide-low-dose dexamethasone with lenalidomide-high-dose dexamethasone included patients who completed 4 cycles of induction therapy. Patients who elected to receive HDT at that time (N = 90) had an estimated 3-year OS of 92% versus 79% for those who continued on primary therapy (N = 248). In an attempt to abrogate the selection bias inherent in this comparison, Siegel and colleagues analyzed the data according to age and found that early ASCT was associated with better outcomes in all age groups. The Mayo group recently published their experience on 290 newly diagnosed patients with MM who received induction therapy with either thalidomide-dexamethasone or lenalidomide-dexamethasone and had stem cells collected. One hundred seventy-eight patients who underwent HDT and ASCT within 12 months of diagnosis made up the early ASCT group; their outcomes including response rates, time to progression (TTP), and OS were no different than the outcomes of the 112 patients who made up the delayed ASCT group. However, the retrospective nature of these data and lack of QOL measurements, again limit the utility of these findings. Indeed the results from the Intergroup Francophone du Myeloma-Dana-Farber Cancer Institute (IFM-DFCI) study of RVD with or without HDT and ASCT as well as others using lenalidomide-dexamethasone as induction followed by early versus delayed ASCT are eagerly awaited.
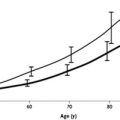
Although the timing of HDT and ASCT remains an area of active debate and investigation, patients who are eligible and responding to initial therapy should have stem cells mobilized and collected after 3 to 6 cycles of therapy. Prolonged therapy, especially with lenalidomide increases the risk of insufficient collection. Age also appears to be a strong predictor of inadequate collection, but age in and of itself does not define eligibility for transplant that is more dependent on comorbidities and performance status. Although phase III trials restricted enrollment to patients aged less than 65 years, retrospective studies suggest that selected patients even in the 8th decade of life may benefit from ASCT with a similarly low risk of treatment toxicity and equivalent remission rates and PFS as seen in younger patients.
Preventing relapse
Despite effective induction and HDT, myeloma recurrence occurs almost universally in patients who do not receive post-transplantation therapy. A defined course of often intensive treatment designed to maximize the depth of response after SCT is considered “consolidation” therapy, whereas “maintenance” typically includes a planned treatment that should be effective, well-tolerated with manageable toxicities, simple to administer, and can be given for an extended period of time. Both strategies have been used to improve outcomes after a single or tandem ASCT and in general deepen responses with variable effect on time-to-event data.
The benefits of consolidation were reported by Ladetto and colleagues who showed that 4 cycles of VTD consolidation following tandem ASCT in patients with MM who achieved at least a VGPR (N = 39) increased the frequency of CR from 15% to 49% and molecular remissions from 3% to 18%. Phase III data included 480 newly diagnosed MM patients who received induction with VTD or TD, that was followed by tandem ASCT and 2 cycles of VTD or TD consolidation according to the induction arm. Although CR rates were not statistically different in the VTD versus TD arms following HDT, the CR rate was 61% after VTD and 47% after TD consolidation ( P = .012). To date, PFS but not OS is longer in the VTD arm. A retrospective study examined the outcomes of newly diagnosed MM patients who received either VTD followed by single SCT (N = 96) or the same induction, a single ASCT, and 2 cycles of VTD consolidation (N = 121). Similar to the phase III trial, an increased proportion of patients who received VTD consolidation achieved CR (52% vs 30%, P = .001); longer TTP (estimated 4-year TTP 62% vs 29%, P = .005) was also evident in patients receiving consolidation. The Nordic Myeloma Study Group randomized 370 bortezomib-naïve patients to 20 weekly doses of bortezomib or no consolidation at 3 months post-transplantation. Again, response rates improved in patients who received consolidation with 71% versus 57% ( P <.01) achieving at least VGPR and PFS was extended (27 vs 20 months, P = .05), but the advantage was only seen in patients with less VGPR rates after ASCT. There was no difference in OS between the groups.
Several studies have examined the role of different types of maintenance including interferon-α, glucocorticoids, and low-dose melphalan to improve response and outcome. However, these agents had limited efficacy and tolerability. Thalidomide maintenance after HDT and ASCT improved the quality of response and increased PFS in 6 studies and OS in 3 of them. However, thalidomide maintenance has been limited by toxicity, namely neuropathy and fatigue, which have made it difficult for physicians and patients to adopt. Lenalidomide has a more favorable side-effect profile and was a logical candidate drug to study as posttransplantation maintenance therapy. Two phase III trials examining the role of lenalidomide maintenance following SCT in newly diagnosed MM patients have been performed and reported. The CALGB 100104 study examined 462 MM patients who were randomized to lenalidomide or placebo without consolidation until disease progression. A significant increase in TTP was seen for patients in the lenalidomide arm compared with those receiving placebo (46 vs 27 months, P <.0001). With a median follow-up of 34 months, 3-year OS was 88% for patients receiving lenalidomide and 80% for those receiving placebo ( P = .028). All patients benefitted from lenalidomide maintenance regardless of remission status or prior exposure to IMID therapy; there was evidence that induction therapy with lenalidomide was associated with improved OS in the group that received lenalidomide maintenance ( P = .03). An updated analysis was performed at 48 months of follow-up and shows that despite cross-over of 71% of placebo patients, the risk of death on lenalidomide maintenance (20%) is lower than on placebo (30%) (hazard ratio [HR] 0.61, P = .008). The IFM 2005-02 trial reported on 614 patients who were randomized to lenalidomide or placebo after single (79%) or tandem (21%) and 2 cycles of lenalidomide consolidation (25 mg × 21 days). Similar to the CALGB study, lenalidomide improved median PFS (41 months vs 23 months) compared with placebo (HR 0.50, P <.001). However, the 5-year post-randomization OS is similar (68% vs 67%, HR 1) due to a shorter median OS after the first progression in the lenalidomide group (29 months) versus those who received placebo (48 months) ( P <.0001). In both studies a higher incidence of secondary primary malignancies (SPMs) in the lenalidomide arm was detected ( Table 2 ). Yet analysis of CALGB 100104 showed that despite a higher cumulative incidence risk (CIR) of developing a second primary malignancy (SPM) in the lenalidomide arm ( P = .03), the CIR of progression ( P = .001) or death ( P = .002) is higher for placebo. One major difference between the CALGB study and the IFM study is that maintenance lenalidomide was continued in the US study, whereas it was stopped at a median of 2 years due to concerns regarding SPM. The benefit of prolonged lenalidomide maintenance on PFS and more recently OS has been shown by the Italian group in both transplant-eligible and transplant-ineligible patients.