Neuroendocrine tumors are rare and slow-growing malignancies that commonly metastasize to the liver, resulting hormonal syndromes and death from liver failure. Surgical consultation and liver debulking are key components in management. Traditional surgical resection guidelines do not apply to these tumors as with other cancers. Surgical resection has shown survival benefit even in the event of an incomplete resection. Ablation may be used as an adjunct to resection or in patients who are not candidates for resection. Asymptomatic patients with high-volume disease do as well with intra-arterial therapy as with surgery.
Key points
- •
Traditional hepatic surgical resection guidelines are not applicable to resection of neuroendocrine tumors, and all patients with metastases should have a surgical consultation.
- •
Patients with neuroendocrine liver metastases benefit from an aggressive surgical approach even if they do not receive a complete resection and have extrahepatic disease.
- •
Radiofrequency ablation is an important adjunct to resection and can be used in patients that are not surgical candidates.
- •
Patients with function tumors and who have R0 and R1 resection derive the most benefit from surgical resection.
Introduction: nature of the problem
Neuroendocrine tumors are rare and slow-growing tumors that arise from neuroendocrine cells, with approximately 70% arising in the gastrointestinal tract. They have a high propensity to spread to the liver. They are also capable of producing hormones that when released from the liver cause hormonal syndromes that reduce quality of life. The vast majority of patients who die of disease will die of liver failure. Therefore, a thorough understanding of treatment options for patients with neuroendocrine liver metastases is essential to achieving the best possible outcomes for symptom control and survival.
Introduction: nature of the problem
Neuroendocrine tumors are rare and slow-growing tumors that arise from neuroendocrine cells, with approximately 70% arising in the gastrointestinal tract. They have a high propensity to spread to the liver. They are also capable of producing hormones that when released from the liver cause hormonal syndromes that reduce quality of life. The vast majority of patients who die of disease will die of liver failure. Therefore, a thorough understanding of treatment options for patients with neuroendocrine liver metastases is essential to achieving the best possible outcomes for symptom control and survival.
Treatment options: liver resection and debulking
Because neuroendocrine liver metastases are usually numerous and bilobar, it has often been estimated only 20% of patients are eligible for liver resection. Even if this percentage is correct, hepatic resection is still being vastly underused. Patients are often not even referred for surgical consultation. A lack of understanding of major differences in eligibility criteria between patients with neuroendocrine tumors and other types of cancers may be responsible for much of the discrepancy.
With other types of cancer, the eligibility criteria for liver resection are fairly strict. Primary tumors must be resected or potentially resectable. Patients with extrahepatic disease are considered ineligible. Even if patients have no extrahepatic disease on preoperative staging scans, if it is discovered at operation, they become ineligible. All liver disease must be completely resectable. Generally, disease should be limited to one portion of the liver, so it can be completely resected via wedge resection, lobectomy, trisegmentectomy, or combinations thereof, leaving an adequate hepatic remnant free of disease. Wide margins of resection are also required because primary liver tumors and colorectal metastases are infiltrative, with microscopic extensions continuing a considerable distance beyond the grossly visible tumor. Positive margins of resection lead to rapid recurrence and poor outcomes.
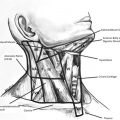
However, as seen from the following review of the literature, these principles are hardly applicable to neuroendocrine liver metastases. In some patients, the primary tumor may never be found. They have still been considered eligible for liver surgery and included in the published major series. Negative margins are not required. Neuroendocrine liver metastases are not infiltrative, but expansive. They push the surrounding liver parenchyma aside rather than invade it, making it possible to separate many tumor masses from the surrounding liver tissue and essentially enucleating them ( Fig. 1 ). This is borne out by the fact that the published series generally show no difference in survival outcomes between R0 and R1 resections. Complete resection of all liver disease is not required. Several series have shown that the results of surgically debulking most of the liver metastases yields survival results equivalent to those obtained with complete resection. Even the presence of extrahepatic disease is not a contraindication to liver resection. The vast majority of patients with metastatic neuroendocrine tumors die of liver failure and not from the extrahepatic disease, and many series show no difference in survival between those with and those without extrahepatic disease.
Liver resection and debulking: review of the literature
Prospective randomized data on the outcomes of surgical treatment of neuroendocrine liver metastases are lacking. Surgical treatment recommendations were initially based on single-institution experiences compared with historical controls. Published series between 1990 and 2001 had small numbers of patients, ranging from 4 to 34, with a mean of 19, and patients usually had complete resections of all liver disease. Reported rates of symptomatic relief were high (88%–100%) and survival rates at 3 to 5 years were encouraging.
Because complete resection of all disease was often not possible, McEntee and colleagues were among the first, in 1990, to advocate surgical debulking when at least 90% of the grossly visible tumor could be resected. Relief of hormonal symptoms in patients with functional tumors was considered the chief justification for proceeding with less than complete resection.
In 2003, Sarmiento and colleagues published a landmark retrospective series of 170 patients who underwent surgical resection with a debulking threshold of 90% of the grossly visible disease. The investigators pointed out that it was difficult to justify incomplete surgical resection solely on the basis of symptom management, particularly for patients with nonfunctional tumors, and endeavored to see if a survival advantage could also be demonstrated. They further endeavored to determine if the operations could be done with acceptable morbidity and mortality.
Their series included patients with liver metastases from carcinoid and pancreatic neuroendocrine primaries and both functional and nonfunctional tumors. The series also included patients with unknown primary tumors and patients with extrahepatic disease. Seventy-six percent had bilobar liver metastases, and 54% underwent some form of major hepatic resection. Forty-four percent of patients had complete resection of all known disease and, among the remainder, 96% had residual disease in the liver, either alone or in combination with other sites. Median blood transfusion was 0 units, ranging up to 17 units. The major and minor complication rates were 17% and 4%, respectively, and the mortality was 1.2%.
Ninety-six percent of patients had improvement or complete relief of their hormonal symptoms. These responses were durable with a median time to recurrence of 45.5 months and a recurrence rate of 59% at 5 years. In carcinoid patients, the improvement in symptoms correlated strongly with a marked reduction in preoperative versus postoperative urinary 5’-hydroxy-indole acetic acid (5′-HIAA) levels from a mean of 585 to a mean of 21 mg per 24 hours. Symptom recurrence rates were lower in patients with compete resection.
Tumor progression and recurrence rates, based on imaging or recurrence of symptoms, were high at 84% at 5 years and 95% at 10 years. There were no differences in recurrence rates between carcinoid and pancreatic neuroendocrine tumor patients.
The 5-year and 10-year overall survival rates were 61% and 35%, respectively, and the median survival was 81 months. No significant differences in survival rates were noted between patients with pancreatic neuroendocrine tumors and carcinoid tumors or between patients who had functional and nonfunctional tumors. The investigators compared their results to historical data from patients with untreated neuroendocrine liver metastases showing 5-year survival rates of 30% to 40% and median survival times of 24 to 48 months. The investigators concluded their data provided evidence that surgical debulking doubles the survival of patients with neuroendocrine liver metastases, with acceptable morbidity and mortality rates, and is therefore justified.
A similar series was published by Glazer and colleagues in 2010. The series included 182 patients with carcinoid and pancreatic neuroendocrine liver metastases, 140 of whom who underwent some type of hepatic resection. Some patients had radiofrequency ablation (RFA) of some lesions. Forty-nine percent had bilobar disease. No patients had extrahepatic disease. The complication rate was 24%, and there were no perioperative deaths. Forty-seven percent had recurrence of their disease. The 5-year and 10-year survival rates were 77% and 50%, respectively, and the median survival was 9.6 years.
The investigators noted that positive margins (R1 or R2) were not associated with significantly worse recurrence-free or overall survival. Thus, the investigators concluded that patients with neuroendocrine liver metastases benefit from an aggressive surgical approach, even if they do not receive a complete resection.
Also in 2010, Mayo and colleagues published a review of surgical treatment of neuroendocrine liver metastases by compiling the databases of 8 international major hepatobiliary centers. This large cohort included 339 patients, of whom 40% had pancreatic primaries and 25% had small bowel primaries. Seventy-eight percent of patients had hepatic resection; 3% had ablation, and 19% had hepatic resection combined with ablation. Forty-five percent of hepatic resections were major resections. Sixty percent of patients had bilobar disease. The debulking threshold was not defined, but patients were divided into groups based on whether they had R0, R1, or R2 resections; 19% had R2 resections.
Ninety-four percent of patients had recurrence at 5 years. The 5-year and 10-year overall survival rates were 74% and 51%, respectively, and the median survival was 125 months. This median survival time was therefore more than 3 times that of the historical median survival times in patients with untreated neuroendocrine liver metastases to which Sarmiento and colleagues compared their results. Patients with functional tumors and R0 or R1 resections derived the most benefit from surgery. On multivariate analysis, synchronous liver metastases, nonfunctional tumors, and extrahepatic disease were significantly associated with decreased survival. However, survival rates for those groups were still very good. Median survival time for patients with extrahepatic disease was 85 months. The median survival time for patients with nonfunctional tumors and R2 resections, a combination of 2 adverse factors, was in excess of 84 months.
In an effort to expand the pool of patients with neuroendocrine liver metastases eligible for liver debulking, the authors’ institution published a series of 52 carcinoid patients in whom the eligibility criteria were expanded to include a debulking threshold of 70%, allowing positive margins and extrahepatic disease. Ninety percent of patients had bilobar disease. Sixty-five percent had extrahepatic disease, and 35% still had extrahepatic disease after operation. The mean number of tumors resected per patient was 22 and ranged from 1 to 131. More than 200 resected metastases were histologically graded and 33% of patients had at least one intermediate grade metastasis despite all reviewed primary tumors being low grade.
The median time to liver progression was 71.6 months. Progression did not correlate with the number or size of tumors resected, grade of metastases, type of hepatic resection, percentage of disease debulked, or the presence of extrahepatic disease. The only factor that correlated with time to liver progression was age. Patients less than 50 years of age had a median time to liver progression of 39 months, whereas the median time to liver progression in patients age 50 and older has not yet been reached.
The 5-year disease-specific survival rate was 90%. All disease-specific deaths were due to liver failure; no patient died of extrahepatic disease. Again, none of the clinical or pathologic factors correlated with survival, except age. Patients less than 50 years of age had a 5-year survival rate of 73%, similar to the overall 5-year survival rates reported in many of the series above. However, the 5-year survival rate for patients age 50 and older was a remarkable 97%.
The complication rates for hepatic resection have generally been reported to be 16% to 24%. The most commonly reported complications are hemorrhage, bile leak, intra-abdominal abscess, pleural effusion, cardiac arrhythmia, and urinary tract infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree