ERBB2 gene amplification occurs in ∼20% of human breast cancers (BC) and is associated with an adverse clinical prognosis, indicating that it may be playing a critical role in disease pathogenesis. Therapeutic strategies targeting pathologic ERBB2 overexpression have revolutionized the diagnosis and treatment of BC. Indeed, humanized anti-ERBB2 antibodies, small molecule ERBB2 kinase inhibitors and ERBB2-targeting antibody-drug conjugates have proven safety and efficacy based upon evidence from randomized phase III clinical trials. Recent progress in targeting ERBB2 alteration will be reviewed, with focus on data that has informed changes in clinical practice for the treatment of BC.
Key points
- •
Level I evidence from multiple large, prospective, randomized, phase III clinical trials supports the use of trastuzumab in combination with chemotherapy as treatment for early-stage ERBB2-positive breast cancer in the adjuvant or neoadjuvant settings.
- •
For patients with metastatic ERBB2-positive disease, there is level I evidence that pertuzumab in combination with trastuzumab and a taxane (docetaxel) yields superior progression-free and overall survival in the first-line setting compared with docetaxel plus trastuzumab alone. This regimen has secured regulatory approval and is a preferred first-line regimen according to guidelines established by the National Comprehensive Cancer Network.
- •
For patients with metastatic ERBB2-positive disease who have progressed following prior treatment with a taxane and trastuzumab, or relapsed within 6 months of completion of an adjuvant trastuzumab regimen, ado-trastuzumab emtansine (T-DM1) has been shown to be significantly superior (for both progression-free and overall survival) to lapatinib plus capecitabine, and is associated with fewer grade 3/4 clinical adverse events. Ado-trastuzumab emtansine was approved by the U.S. Food and Drug Administration in February 2013.
Introduction
The discovery of ERBB2 gene amplification in ∼20% of human breast cancers (BC) and its association with an adverse clinical prognosis, indicating that it may be playing a critical role in disease pathogenesis, has revolutionized the diagnosis and treatment of BC. In addition to improving overall survival in ERBB2-positive advanced BC, humanized anti-ERBB2 monoclonal antibody trastuzumab, when added to standard adjuvant chemotherapy, reduces relapse risk by approximately one-half and reduces mortality by about one-third in ERBB2-amplified/overexpressed early-stage BC, and, to date, has withstood the test of time. Trastuzumab has established a benchmark for treatment of ERBB2-positive disease and has set a high bar of efficacy to overcome for newer emerging ERBB2-targeted therapeutic approaches. However, within the past year, we have witnessed new paradigms that will challenge the chemotherapy plus trastuzumab “gold-standard” treatment for ERBB2-positive disease. These new approaches include the addition of a “second-generation” humanized anti-ERBB2 antibody (pertuzumab) in combination with trastuzumab plus chemotherapy, and the development of an antibody-drug conjugate (ADC) based on trastuzumab. Each of these new approaches has already proven to be practice changing, once again raising the bar for clinical efficacy (and therapeutic index) against ERBB2-positive BC. Given this rapid pace of discovery research and clinical validation, the past year will likely be remembered as a golden age of ERBB2-targted therapy for BC.
Introduction
The discovery of ERBB2 gene amplification in ∼20% of human breast cancers (BC) and its association with an adverse clinical prognosis, indicating that it may be playing a critical role in disease pathogenesis, has revolutionized the diagnosis and treatment of BC. In addition to improving overall survival in ERBB2-positive advanced BC, humanized anti-ERBB2 monoclonal antibody trastuzumab, when added to standard adjuvant chemotherapy, reduces relapse risk by approximately one-half and reduces mortality by about one-third in ERBB2-amplified/overexpressed early-stage BC, and, to date, has withstood the test of time. Trastuzumab has established a benchmark for treatment of ERBB2-positive disease and has set a high bar of efficacy to overcome for newer emerging ERBB2-targeted therapeutic approaches. However, within the past year, we have witnessed new paradigms that will challenge the chemotherapy plus trastuzumab “gold-standard” treatment for ERBB2-positive disease. These new approaches include the addition of a “second-generation” humanized anti-ERBB2 antibody (pertuzumab) in combination with trastuzumab plus chemotherapy, and the development of an antibody-drug conjugate (ADC) based on trastuzumab. Each of these new approaches has already proven to be practice changing, once again raising the bar for clinical efficacy (and therapeutic index) against ERBB2-positive BC. Given this rapid pace of discovery research and clinical validation, the past year will likely be remembered as a golden age of ERBB2-targted therapy for BC.
Investigation of a second-generation anti-ERBB2 antibody, pertuzumab: an ERBB2 dimerization inhibitor
In an early screening of a panel of murine monoclonal anti-ERBB2 antibodies, 2 antibodies stood apart from others in terms of demonstration of preclinical efficacy in cell proliferation assays in vitro, and in primary human tumor xenotransplants grown in the subrenal capsule of athymic mice in vivo (D. Slamon, personal communication, 1991). Two of the most promising murine antibodies to emerge from such screens were 4D5, which, when humanized, became trastuzumab, and 2C4, which, following humanization, is now called pertuzumab. Experimentally, it became evident that these 2 anti-ERBB2 antibodies were distinct, both functionally as well as structurally. In contrast to trastuzumab, which binds to a juxtamembrane epitope in subdomain IV of the ERBB2 extracellular domain (ECD), pertuzumab binds to the dimerization interface contained in subdomain II of the ERBB2 ECD ( Fig. 1 ). This distinction is biologically relevant in that pertuzumab disrupts the ability of ERBB2 to dimerize with any other ERBB receptor family member, thus attenuating signaling events triggered by ERBB receptor family ligands. For a time it was hoped that this could set the stage for pertuzumab treatment of ERBB2 nonamplified tumor types, if their pathogenesis proved to be driven by ligand-activated heterodimeric complexes containing ERBB2 as a co-receptor. Unfortunately, with the possible exception of platinum-refractory ovarian cancer, this hypothesis was not supported by early clinical trial data of single-agent pertuzumab in ERBB2-negative malignancies; thus, focus returned to the development of pertuzumab in ERBB2-positive disease states, in particular, BC. In preclinical models, a combination of trastuzumab plus pertuzumab synergistically inhibited the survival of ERBB2-amplified breast cancer cells. Combination drug treatment reduced levels of total and phosphorylated ERBB2 protein and blocked receptor signaling through Akt, resulting in induction of apoptosis, but did not affect mitogen-activated protein kinase. These results suggested the possibility that combining ERBB2-targeting agents may be a more effective therapeutic strategy than treating with a single ERBB2-directed antibody alone. Consequently, following phase II proof of concept clinical studies, randomized pivotal trials designed to explore the paradigm of dual antibody therapy for ERBB2-positive breast cancer ensued. In a clinical evaluation of pertuzumab and trastuzumab (CLEOPATRA) combination in first-line metastatic disease, 808 ERBB2+ patients were randomized to receive docetaxel plus trastuzumab and placebo versus docetaxel and trastuzumab plus pertuzumab. In an independently assessed analysis of clinical efficacy, the median progression-free survival (PFS) in the control arm was 12.4 months, compared with 18.5 months in the pertuzumab arm (hazard ratio [HR] = 0.62; P <.001). An interim analysis of overall survival (OS) also showed a strong trend in favor of pertuzumab plus trastuzumab plus docetaxel; however, although the P value was .005, it did not cross the prespecified O’Brien-Flemming value of P = .001. More recently, a confirmatory OS analysis has been presented. In this analysis, the hazard ratio was 0.66 (95% confidence interval [CI] = 0.52–0.84) in favor of the experimental arm, and the P -value (.0008) has achieved statistical significance. Notably, the safety profile was generally similar in the 2 treatment groups, and there was no increase in left ventricular systolic dysfunction, although the rates of febrile neutropenia and diarrhea of grade 3 or greater were higher in the pertuzumab-treated group. These data suggested that further exploration of this approach in the early disease setting was warranted. Accordingly, a randomized phase II trial of pertuzumab/trastuzumab combination in the neoadjuvant setting has been conducted (NeoSphere). In this multicenter, open-label, phase II study, treatment-naive women with ERBB2-positive BC were randomly assigned to receive 4 neoadjuvant cycles of trastuzumab plus docetaxel, or pertuzumab and trastuzumab plus docetaxel, or pertuzumab and trastuzumab, or pertuzumab plus docetaxel. Patients given pertuzumab and trastuzumab plus docetaxel had a significantly improved pathologic complete response (pCR) rate (45.8%) as compared with those given trastuzumab plus docetaxel (29%; P = .0141), without substantial differences in tolerability. It should be noted, however, that the time-to-relapse event data have not yet been reported in this study; therefore, it is not yet known whether improved pCR rates for the combination arm will translate into improved relapse-free or overall survival. Therefore, in contrast to the CLEOPATRA study in advanced disease, the NeoSphere data cannot yet be considered to be practice changing, although under a new guidance issued recently by the US Food and Drug Administration (FDA), pertuzumab could in theory be considered for accelerated regulatory approval in the neoadjuvant setting on the basis of the NeoSphere data, coupled with the ongoing commitment to a randomized phase III adjuvant pertuzumab study. Taken together, the findings from CLEOPATRA and NeoSphere suggest that targeting ERBB2-positive tumors with 2 anti-ERBB2 monoclonal antibodies that have complementary mechanisms of action results in a more comprehensive blockade of ERBB2 and highlights the clinical importance of preventing the ligand-dependent formation of ERBB2-containing dimers (particularly ligand-activated heterodimers) to best silence ERBB2-driven downstream signaling events. A study of pertuzumab plus trastuzumab adjuvant therapy in patients with newly diagnosed ERBB2-positive early breast cancer has been initiated and is currently underway (Adjuvant Pertuzumab and Herceptin in Initial Therapy in Breast Cancer; APHINITY; NCT01358877 ).
Antibody-drug conjugate ado-trastuzumab emtansine: synergy between trastuzumab and a cytotoxic via covalent conjugation
Antibody-drug conjugates can be constructed by direct covalent linkage of a therapeutic drug (often a cytotoxic/chemotherapeutic species) directly to a monoclonal antibody backbone. By design, the antibody component of the ADC is merely being used as a delivery vehicle to transport a cytotoxic payload selectively to tumor cells. In ADC constructs the linker chemistry is critical to the success of the approach, because if the chemistry is too labile, the molecule will be unstable in the circulation and could lead to excessive toxicity if the cytotoxic species is liberated in normal tissue compartments. On the contrary, in theory if the linker chemistry is too stable, then the cytotoxic species may not be appropriately liberated in situ in the tumor microenvironment, thus limiting its potential for antitumor efficacy. Accordingly, fine-tuning of linker chemistry is required for optimization of ADC efficacy and may be unique to each target, especially considering pharmacologic properties of the cytotoxic moiety. For example, different results may be observed with targets that are internalized following antibody binding to tumor cells as compared with those that are not. The author previously reported preclinical efficacy of an ADC based on trastuzumab. For these experiments, a bifunctional linker was used to create a targeted prodrug that links to the chemotherapeutic agent paclitaxel, via an energy-reversible ester bond. This study demonstrated in vivo efficacy of a single treatment of trastuzumab-paclitaxel ADC in decreasing tumor volume and tumor cell density of human ERBB2-positive BT-474 mammary tumor cells implanted in severe combined immunodeficiency mice. Moreover, the ADC was more effective in killing tumor cells than equivalent concentrations of coadministered trastuzumab and paclitaxel. Thus the therapeutic index (efficacy ÷ toxicity) could be increased markedly by an ADC approach.
Another trastuzumab-based ADC is trastuzumab-DM1 (T-DM1; ado-trastuzumab emtansine), which is composed of a maytansinoid derivative, linked with a nonreducible thioether linker termed [N-maleimidomethyl] cyclohexane-1-carboxylate. As a result, derivatization of trastuzumab occurs predominantly on the epsilon amino groups of lysines, which are abundant (N = 91) and distributed throughout the antibody sequence. Interestingly, the binding affinity, specificity, signal perturbation capability, and effector functions of trastuzumab remain intact despite DM1 conjugation. Maytansinoids are natural products that are potent antimitotic agents, which, like the vinca alkaloids, prevent microtubule assembly. It is postulated that following receptor-mediated endocytosis, T-DM1 undergoes intralysosomal proteolytic degradation resulting in the release of Lys-MCC-DM1 and subsequent antitubulin-associated cell death ( Fig. 2 ). In the phase I dose escalation study of T-DM1, thrombocytopenia was found to be a dose-limiting toxicity. In 2 phase II studies in patients with heavily pretreated ERBB2-positive advanced cancers who had progressed on trastuzumab and chemotherapy, or both trastuzumab and lapatinib-based regimens in the metastatic setting, T-DM1 produced response rates between 33.8% and 41%. In one study, higher response rates and longer response durations were seen in patients with centrally confirmed ERBB2-amplified disease, once again reinforcing the importance of accurate ERBB2 testing in patients receiving ERBB2-targeted therapies. In a randomized study in previously untreated metastatic patients with ERBB2-positive breast cancer, T-DM1 also produced higher response rates and had a favorable toxicity profile compared with free trastuzumab given in combination with free docetaxel. Importantly, in terms of therapeutic index, the incidence of grade ≥3 adverse events in the T-DM1 arm was just half that observed in the trastuzumab plus docetaxel arm (37% vs 75%). No grade 3 neutropenia was observed with T-DM1, and remarkably just 1.5% of patients experienced alopecia. Fortunately, in this study trastuzumab-DM1 was not associated with an increased risk of cardiotoxicity compared with trastuzumab plus docetaxel.
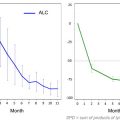
EMILIA ( NCT00829166 ) is a phase 3, multinational, multicenter, open-label study evaluating the efficacy and safety of T-DM1 versus capecitabine plus lapatinib (XL), an approved combination for trastuzumab-refractory ERBB2-positive metastatic BC. Upon informed consent, patients were randomized to receive T-DM1 (3.6 mg/kg IV every 3 weeks) or X (1000 mg/m 2 twice a day, days 1–14 evert 3 weeks) + L (1250 mg PO every day, days 1–21) until disease progression. Key eligibility criteria included central confirmation of ERBB2 status (IHC 3+ or FISH-positive) and prior treatment with trastuzumab and a taxane. Primary endpoints were PFS by independent review, OS, and safety. Baseline demographics, prior therapy, and disease characteristics were balanced between the T-DM1 (n = 495) and XL (n = 496) arms. Median durations of follow-up were 12.9 (T-DM1) and 12.4 (XL) months. Patients in the T-DM1 arm had significantly longer median PFS than those in the XL arm (9.6 vs 6.4 mo; HR = 0.650 [95% CI, 0.549–0.771]; P <.0001). Median OS was not reached in the T-DM1 arm versus 23.3 mo in the XL arm (HR = 0.621 [95% CI, 0.475–0.813]; P = .0005); however, the interim efficacy O’Brien-Flemming statistical boundary was not crossed. More recently, in an updated OS analysis, the O’Brien-Flemming boundary was met in this study (stratified HR = 0.682; 95% CI = 0.548–0.849, P = .0006), confirming improved OS in the T-DM1 experimental arm. Moreover, in the planned analysis, 1-year (85% [95% CI, 81%–89%] vs 77% [72%–82%]) and 2-year (65% [59%–72%] vs 48% [39%–56%]) survival rates were greater with T-DM1. There were fewer grade ≥3 adverse events with T-DM1 (41% vs 57%) and fewer dose reductions (16% with T-DM1 vs 53% with X and 23% with L). This impressive result from an ADC therapeutic approach offers a new paradigm for the treatment of ERBB2-positive advanced BC and suggests that further exploration of this ADC is warranted in (1) earlier lines of treatment for advanced disease, and (2) early-stage ERBB2-positive breast cancer. The Marianne study (BO22589/TDM4788g) is an ongoing randomized, phase III, placebo-controlled study in first-line ERBB2-positive metastatic BC (N = 1092) that randomizes patients to receive trastuzumab plus a taxane versus T-DM1 plus placebo versus T-DM1 plus pertuzumab. Primary endpoints are PFS assessed by independent review and safety, whereas secondary endpoints include OS, patient-reported outcomes, and an exploratory biomarker analysis. It is hoped that the result of this trial will help to inform potential regimens to be considered for future adjuvant T-DM1 campaigns. Meanwhile, a randomized, multicenter, open-label phase III study is underway (NSABP B-50) to evaluate the efficacy and safety of T-DM1 versus trastuzumab as adjuvant therapy for patients with ERBB2-positive primary breast cancer whose tumors fail to achieve a pathologic complete response in the breast or axillary lymph nodes following neoadjuvant trastuzumab-based induction therapy. Such patients have a particularly high relapse risk; thus, this clinical setting is ideally suited for testing adjuvant T-DM1, because these patients have high unmet need for improved outcomes.
Combinations of ERBB2-targeting agents with endocrine therapy
Approximately half of ERBB2-positive breast cancers are also hormone receptor (estrogen receptor and progesterone receptor) positive. Women with disease coexpressing both ERBB2 and hormone receptors may be relatively resistant to endocrine therapies compared with those with ERBB2-negative, hormone receptor-positive disease. Preclinical studies suggest that there is cross-talk between cell signaling pathways activated by ERBB2 and ER. Overexpression of ERBB2 was demonstrated to cause ligand-independent down-regulation of estrogen receptor in association with suppression of ER transcripts. Given this association, it was hypothesized that inhibition of ERBB2 activity may augment response to endocrine therapy by enhancing ER expression. To explore this hypothesis, the phase III TAnDEM trial randomized ERBB2-overexpressing, HR-positive postmenopausal patients to anastrozole alone, or the combination of anastrozole and trastuzumab. Patients in the trastuzumab plus anastrozole arm experienced significant improvements in PFS compared with patients receiving anastrozole alone (HR = 0.63; 95% CI, 0.47 to 0.84; median PFS, 4.8 vs 2.4 months; log-rank P = .0016). At the time of progression, patients were given the option to begin trastuzumab therapy if they were previously randomized to the monotherapy arm. Despite the crossover allowance, a modest (statistically insignificant) trend in OS was noted from combination therapy (28.5 vs 23.9 mo; P = .325). Interestingly, in a post-hoc exploratory analysis assessing the effects of crossover, median OS was significantly less in the group that received no trastuzumab therapy (ie, anastrozole alone with no crossover; median OS, 17.2 months) versus survival in groups receiving anastrozole and trastuzumab initially (median OS 28.5 months) or at the time of crossover (median OS 25.1 months).
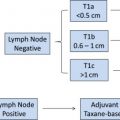
Direct ERBB2-tyrosine kinase inhibition with the small molecule ERBB2 kinase inhibitor lapatinib in combination with endocrine therapy has also been investigated. A phase I trial using the combination of lapatinib and letrozole suggested that the combination was safe and tolerable. Subsequently, a phase III trial was undertaken that compared the combination of letrozole plus lapatinib with letrozole plus placebo as first-line treatment of patients with hormone receptor-positive metastatic breast cancer, some with ERBB2-positive disease. Seventeen percent of the total study population (N = 1286) had centrally confirmed ERBB2-positive disease with roughly equal distribution in the lapatinib and placebo groups (n = 111 and n = 108, respectively). In a preplanned analysis of the ERBB2-positive population, the median PFS increased from 3 months for letrozole-placebo to 8.2 months for letrozole-lapatinib (HR = 0.71; 95% CI 0.53 to 0.96; P = .019). Clinical benefit, defined as objective response or stable disease for ≥6 months, was also significantly improved (29%–48%; OR = 0.4; 95% CI, 0.2 to 0.8; P = .003) for the combined receptor blockade arm. There was also a (nonsignificant) trend toward improvement in OS. This regimen won regulatory approval by the US FDA in 2010. In summary, because ER signaling has been suggested as an escape mechanism causing resistance to ERBB2 targeting agents, it is important to remember that ER+ tumors in the setting of ERBB2+ disease should also be treated with ER-directed therapies. This paradigm is also suggested by recent results from the TBCRC 006 trial, in which letrozole was used in addition to trastuzumab and lapatinib in 64 evaluable patients with ERBB2+/ER+ stage II/III tumors. Overall, in-breast pathologic complete response ( yp T 0-is ) was 27% (ER+, 21%; ER−, 36%). The rate of low-volume residual disease ( yp T 1a-b ) was 22% (ER+, 33%; ER−, 4%). Thus, in these patients with locally advanced ERBB2-positive breast cancer, this approach resulted in a high pCR rate even in the absence of chemotherapy. These data support the hypothesis that selected patients with ERBB2-positive tumors may not require chemotherapy. Consequently, multifaceted blockade of ERBB family receptors and ER is an effective strategy worthy of further study.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree