This article reviews translational research in endocrine surgery, with a focus on disorders of the thyroid, parathyroids, adrenals, and endocrine pancreas. Discovery of genes responsible for heritable endocrine cancer syndromes has increased knowledge of the causes and mechanisms of endocrine cancer and has refined surgical treatment options. Knowledge of mutations in sporadic cancer has led to rapid progress in small-molecule kinase inhibitor strategies. These breakthroughs and their influence on current therapy are discussed to provide surgeons with an overview of the basic science research currently creating new clinical treatments and improving patient care.
Key points
- •
Basic science research has identified the genes responsible for several hereditary endocrine tumor syndromes, and has elucidated the cell-signaling pathways critical to development of endocrine cancer.
- •
Genetic testing for these mutations allows identification of at-risk individuals for screening before the onset of symptoms, and in some cases permits prophylactic surgery.
- •
Mutations in genes of the MAP-kinase signaling pathway (most commonly RET or BRAF ) are found in most familial and sporadic thyroid cancers and cause constitutive proliferative signaling, leading to malignancy.
- •
Small-molecule kinase inhibitors block aberrant promalignant signaling in several endocrine cancers, and represent an active area of research with great potential. Improvements in progression-free survival have been reported with these drugs for thyroid, adrenal, and endocrine pancreatic cancer, but responses are usually not durable, and efforts to understand and overcome inhibitor resistance are ongoing.
- •
In pancreatic neuroendocrine tumors, drugs targeting somatostatin receptors alleviate symptoms, are useful for imaging, and can prolong life. Targeted radiotherapy directed toward these receptors and the development of additional receptor targets promise to improve the treatment of these tumors in the future.
Introduction
The past 30 years have seen astounding advances in the science of endocrine surgery. From early successes in mapping and cloning genes responsible for heritable endocrine cancer syndromes, to sequencing the human genome, to adoption of next-generation sequencing techniques, a broad understanding of genes responsible for familial and sporadic endocrine cancers now exists. This development has enabled genetic testing of at-risk family members and even prophylactic surgery for some carriers of mutant genes. Parallel efforts to determine the function of these altered genes have defined cell-signaling pathways susceptible to treatment. High-throughput gene expression methodologies now give insight into entire networks of cellular processes perturbed in endocrine malignancy. The knowledge gained has led to development of small-molecule kinase inhibitors and other therapies that are able to specifically target the genes, pathways, and cells responsible for disease. New treatments based on rational drug development and targeted therapies continue to be the focus of aggressive investigation and ongoing clinical trials. Diagnosis and prognostication in endocrine cancer has likewise been improved using the results of mutation and gene-expression data. The aim of this article is to review advances in the basic science of endocrine cancer, and highlight how these discoveries are being translated into real-world tests and therapies that will affect the practice of endocrine surgery today and in the near future. Heritable and sporadic tumors of the thyroid, parathyroids, adrenals, and pancreas are emphasized. It is expected that familiarity with these breakthroughs and with the ongoing challenges in endocrine cancer surgery will enhance clinicians’ ability to apply the latest scientific developments to the optimal care of their patients.
Introduction
The past 30 years have seen astounding advances in the science of endocrine surgery. From early successes in mapping and cloning genes responsible for heritable endocrine cancer syndromes, to sequencing the human genome, to adoption of next-generation sequencing techniques, a broad understanding of genes responsible for familial and sporadic endocrine cancers now exists. This development has enabled genetic testing of at-risk family members and even prophylactic surgery for some carriers of mutant genes. Parallel efforts to determine the function of these altered genes have defined cell-signaling pathways susceptible to treatment. High-throughput gene expression methodologies now give insight into entire networks of cellular processes perturbed in endocrine malignancy. The knowledge gained has led to development of small-molecule kinase inhibitors and other therapies that are able to specifically target the genes, pathways, and cells responsible for disease. New treatments based on rational drug development and targeted therapies continue to be the focus of aggressive investigation and ongoing clinical trials. Diagnosis and prognostication in endocrine cancer has likewise been improved using the results of mutation and gene-expression data. The aim of this article is to review advances in the basic science of endocrine cancer, and highlight how these discoveries are being translated into real-world tests and therapies that will affect the practice of endocrine surgery today and in the near future. Heritable and sporadic tumors of the thyroid, parathyroids, adrenals, and pancreas are emphasized. It is expected that familiarity with these breakthroughs and with the ongoing challenges in endocrine cancer surgery will enhance clinicians’ ability to apply the latest scientific developments to the optimal care of their patients.
Thyroid
Overview of Mitogen-Activated Protein Kinase
The mitogen-activated protein kinase (MAPK) cascade is a cellular signaling pathway now established as central to thyroid cancer. In this cascade, extracellular signals such as vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), and many others activate membrane-bound receptor tyrosine kinases, including RET, which cause RAS activation and induction of the RAS-RAF-MEK-ERK-MAP signaling cascade ( Fig. 1 ). Activation of the MAPK pathway influences diverse cellular processes including cell-cycle control, proliferation, differentiation, motility, and apoptosis. The pathway is highly regulated through expression of multiple isoforms of component proteins and cross-talk with related pathways, such as phosphatidylinositol-3-kinase/Akt/mammalian target of rapamycin (PI3K/Akt/mTOR), Janus-kinase, PKC/NF-κB, and Wnt/β-catenin, each contributing to different functional roles in different tissues and contexts. Apart from its physiologic role in thyroid differentiation, growth, and function, the MAPK pathway can also contribute to development of thyroid cancer by aberrant activation at several points. In sporadic and hereditary medullary thyroid cancer (MTC), mutant RET activates RAS, causing constitutive MAPK signaling, while mutations in both RET and RAS are common in follicular thyroid cancer. Downstream in the pathway, mutation in the BRAF serine/threonine kinase has emerged as the most common genetic abnormality in papillary thyroid cancer (PTC), and is also present in anaplastic thyroid cancer (ATC). In total, mutation in some element of the MAPK pathway is present in more than 70% of thyroid cancers, marking this as the central cellular control element in thyroid oncogenesis. Over the past 25 years, basic and translational research has defined the role of the MAPK pathway in thyroid cancer and has produced promising new diagnostic and therapeutic strategies for this heterogeneous disease.
RET Proto-Oncogene
Although the phenotype and autosomal dominant inheritance pattern of multiple endocrine neoplasia type 2 had been recognized for some time, it was not until 1987 that genetic linkage analysis mapped the causative locus for MEN2A to near the centromere of chromosome 10. Other heritable MTC phenotypes, such as MEN2B and familial medullary thyroid cancer (FMTC), were subsequently linked to the same region. A gene known to map to this part of chromosome 10 was the RET proto-oncogene. RET (REarranged during Transfection) was first identified as a human lymphoma oncogene capable of transforming cells in vitro. A gene isolated from papillary thyroid cancer specimens ( PTC) had the same effect and also mapped to chromosome 10. Further investigation showed that this PTC oncogene was actually chimeric RET rearranged and fused with another gene to form the RET/ PTC proto-oncogene. In 1993, linkage narrowed the MEN2A locus to a small area near the RET proto-oncogene, and RET was identified as the causative gene in MEN2A and FMTC, with 2 groups reporting heterozygous germline mutations in affected patients, but not in normal controls and unaffected family members. Description of RET mutations in MEN2B kindreds followed soon thereafter.
Genetic tests to presymptomatically identify affected individuals in families with MEN2 and FMTC became more directed after identification of these mutations. Wells and colleagues became the first to use a genetic test to recommend prophylactic surgery, performing total thyroidectomy and parathyroidectomy in asymptomatic patients within MEN2A families found to carry RET mutations. Of interest is that even in patients with normal calcitonin levels, all of the thyroidectomy specimens contained evidence of precancerous C-cell hyperplasia or overt MTC.
With RET identified as the mutation responsible for MEN2A, MEN2B, and FMTC, it became clear that disease features varied according to the specific mutations present. In 1994, Mulligan and colleagues reported that MEN2A families with parathyroid hyperplasia and pheochromocytoma carried the C634R RET mutation much more frequently than families lacking these disease features. In 1996, the International RET Consortium pooled sequencing and clinical data from 477 MEN2 and FMTC families to catalogue the various mutations’ phenotypic associations ( Table 1 ). These data revealed that codon-634 mutations accounted for 85% of MEN2A cases, and that the C634R mutation was significantly more likely to lead to hyperparathyroidism and pheochromocytoma. Families with the less aggressive FMTC had mutations in several codons including 634, but none carried the C634R mutation. Finally, 75 of 79 MEN2B families had the same M918T mutation. These results and others demonstrated the robustness of the genetic diagnoses, provided valuable information regarding which patients were at highest risk for additional disease features beyond MTC, and provided a strong rationale for very early surgery in the highest-risk patients to preempt development of metastatic MTC.
| Codon, No. (%) of Families with Mutations | ||||||||
|---|---|---|---|---|---|---|---|---|
| 609 | 611 | 618 | 620 | 634 | 768 | 804 | 918 | |
| MEN2B | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 75 (100) |
| MEN2A(1) | 0 | 0 | 5 (6) | 2 (2) | 84 (92) | 0 | 0 | 0 |
| MEN2A(2) | 0 | 3 (3) | 4 (4) | 12 (13) | 76 (80) | 0 | 0 | 0 |
| MEN2A(3) | 1 (8) | 2 (15) | 1 (8) | 0 | 9 (69) | 0 | 0 | 0 |
| FMTC | 2 (7) | 1 (3) | 10 (33) | 5 (17) | 9 (30) | 3 (10) | 0 | 0 |
| Other | 2 (1.5) | 7 (5) | 18 (13) | 13 (10) | 93 (68) | 1 a (<1) | 2 a (1.5) | 0 |
a Families with medullary thyroid carcinoma (FMTC) but too few cases (≤3) per family to exclude other MEN2A disease features.
Consensus guidelines grouping all known mutations into risk categories with recommendations for screening and age of thyroidectomy were developed in 2001, and updated by the American Thyroid Association (ATA) in 2009. For the highest-risk MEN2B mutations, thyroidectomy is recommended as soon as possible and ideally before 1 month of age, with central node dissection recommended if surgery is delayed beyond 1 year of age ( Table 2 ). For the next highest risk group, thyroidectomy is recommended before 5 years, and for some lesser high-risk mutations, patients and surgeons may consider delaying thyroidectomy to before age 10 in the setting of normal calcitonin and ultrasonography, less aggressive family history, and strict compliance with screening. Certain MEN2A mutations, such as C609Y, lead to MTC usually only after age 20 to 40 years, and thyroidectomy between ages 5 and 10 for these patients can be acceptable under the ATA guidelines. Nevertheless, rare examples of MTC in very young patients with mutations thought to confer lower risk do exist, and therefore early thyroidectomy (before age 5 years) remains a reasonable option for these groups. With the high sensitivity and specificity of genetic testing, and the fact that 98% of MEN2 patients have a known RET mutation, genetic testing is now the standard to determine prophylactic surgical therapy in MEN2.
| Recommended Age for Thyroidectomy | MTC Risk Category | Codons |
|---|---|---|
| Before 1 y (preferably before 1 mo) | D | 883, 918, 922, compound 804 a |
| Before 5 y | C | 634 |
| Consider surgery before 5 y | B | 609, 611, 618, 620, 630 |
| Consider delaying to before 5–10 y b | A | 768, 790, 791, 804 a , 891 |
a Compound 804+(778, 805, 806, or 904) mutations have higher risk than isolated codon 804 mutations.
b With less aggressive family history and appropriate negative screening.
RET in Sporadic MTC
RET mutations are found with high frequency in sporadic MTC. A study of 100 sporadic MTC patients with 10-year median follow-up identified somatic RET mutations in 43%, and found that their presence strongly correlated with lymph node and distant metastases (70% and 30% vs. 26% and 12% in RET -positive and RET -negative patients, P <.0001). Of patients with mutations, 79% had the same M918T mutation found in most MEN2B cases. Sporadic RET mutations also independently predicted worse outcomes, with significantly reduced disease-free and overall survival. In a separate study of 36 patients with sporadic and 21 with familial MTC, 75% of tumors had RET mutations and 16% had RAS mutations. Knowledge of mutational status in sporadic MTC will likely become increasingly important for stratification in clinical trials, or in directing therapy toward specific pathways.
Overview of BRAF
RAF kinase is normally activated by RAS, and in turn activates MEK in the MAPK pathway (see Fig. 1 ). Three genes encode different isoforms of RAF (A-RAF, B-RAF, and C-RAF), and of these, BRAF has proved to be important in several human cancers. In 2002, a genome-level screen for cancer-related mutations found activating somatic BRAF mutations in many human tumor cell types, including 59% of melanoma lines studied. Although more than 30 BRAF mutations have been described, a single base-pair substitution (T1799A) replacing valine with glutamate at residue 600 (V600E) is both the most common and most potent mutation, leading to a 700-fold increased kinase activity, constitutive activation of the MAPK pathway, transformation of cells in vitro, and growth of tumors in mice in vivo.
Soon after the initial report of BRAF mutations in human cancer, the V600E mutation was reported in a high percentage of human PTCs. Kimura and colleagues found the BRAF mutation in 28 of 78 (36%) adult, non–radiation-exposed PTC specimens, whereas RET and RAS mutations accounted for only 16% of cases each. Concurrently, another group reported the V600E mutation in 24 of 35 (69%) PTC specimens in a screen of 476 samples from diverse types of primary tumors. BRAF mutation was determined to occur more frequently in tall-cell and less commonly in follicular variants of PTC, and a recent meta-analysis established a 45% overall prevalence of the V600E mutation in papillary thyroid cancer (1118 of 2470 published cases). Whereas MTCs do not carry BRAF mutations, 24% to 40% of ATCs do, and BRAF mutations are common in poorly differentiated, recurrent, and radioiodine-resistant thyroid cancers.
Intense research in the past decade revealed much about the molecular, cellular, and clinical effects of BRAF mutation. Determination of the crystal structure of mutant BRAF protein showed how the V600E mutation, nestled between activating phosphorylation sites at T599 and S602, disrupts the hydrophobic interactions that stabilize the inactive form of the protein, and mimics the conformation of a phosphorylated state. This change creates a pseudophosphorylated conformation, leading to constitutive pathway activation and tumorigenic behavior. Consistent with this model, invasiveness of thyroid cancer cell cultures expressing BRAF V600E was found to require signaling via the MAPK pathway. Thyroid cells with the V600E mutation also show reduced markers of differentiation. Using inducible BRAF V600E mutant rat thyroid cell lines, Mitsutake and colleagues showed suppressed expression of genes necessary for iodine handling and thyroid differentiation, such as thyrotropin receptor ( TSHR ), sodium-iodine symporter ( NIS ), and thyroglobulin ( Tg ), as well as increased chromosomal instability. In both rat and human thyroid cell lines, these phenotypes could be corrected by treatment with the MAPK inhibitor U0126.
Despite the clear importance of the MAPK pathway, there is a growing understanding that BRAF mutations also influence related pathways. In thyroid cell culture with an inducible V600E mutation, Palona and colleagues showed upregulation of matrix metalloproteinases and inhibitors of apoptosis. The upregulation was not blocked by inhibitors of the MAPK pathway, but instead depended on NF-κB. Similarly, Liu and Xing showed that while a MEK kinase inhibitor led to reduced invasiveness and cell-cycle arrest in thyroid lines harboring BRAF mutations, this effect was potentiated by concurrent blockade of the NF-κB pathway. Wild-type BRAF must form homodimers or heterodimers with CRAF to signal, and it forms these dimers only in response to RAS signaling. By contrast, BRAF V600E is always active, and forms homodimers or heterodimers in the absence of RAS signaling, and can additionally activate MEK as a monomer. Monomers and homodimers of mutant BRAF as well as heterodimers with wild-type RAF proteins may participate in MEK-independent signaling with the PI3K/AKT/mTOR, NF-κB, and other pathways. Through both direct activity of mutant BRAF and feedback from the constitutively active MAPK pathway, mutant BRAF may contribute to cross-talk effects in other pathways. These complex interactions belie the standard linear depiction of the MAPK pathway and have frustrated the development of some pathway inhibitor–based therapeutics.
BRAF in Clinical Risk
As data accumulated to elucidate the molecular effects of the BRAF V600E mutation in thyroid cancer, clinical data have similarly accrued to support a picture of uncontrolled promalignant signaling. Tumors with the BRAF V600E mutation show increased risk for recurrence, lymphatic and distant metastases, and unfavorable pathologic characteristics predictive of more aggressive disease. In one study, 76% (24 of 34) of BRAF V600E–positive ( BRAF+) PTC primary tumors had positive sentinel lymph nodes, whereas only 17% (12 of 69) of BRAF V600E–negative ( BRAF −) primary tumors did. In another series, correlation of outcomes with retrospective BRAF testing of 190 PTC fine-needle aspiration (FNA) specimens showed that patients with BRAF + FNAs had higher rates of unfavorable pathologic characteristics, with more frequent recurrence (36% vs 12%), more lymph node metastases (39% vs 19%), and more capsular invasion (29% vs 16%) than BRAF − FNAs. A long-term study of 203 PTC patients with median follow-up of more than 7 years found significant association between BRAF + status and recurrence (21 vs 7%, P = .04), but BRAF status itself was not an independent predictor of recurrence on multivariate analysis. Pooling 2470 patients from 452 studies regarding BRAF mutational status and clinical outcomes in PTC, Tufano and colleagues determined that BRAF mutation correlates with a higher risk of recurrence and metastasis. Overall, BRAF positivity was associated with significantly higher relative risk (RR) of tumor recurrence (24.9% vs 12.6%, RR 1.93), lymph node metastasis (54.1% vs 36.8%, RR 1.32), stage III or IV disease (35.4% vs 19.6%, RR 1.70), and extrathyroidal extension (46.2% vs 23.6%, RR 1.71) compared with BRAF − PTCs. There was no difference in distant metastasis (8.0% vs 7.9%). Testing for BRAF mutation informs risk estimates for resected thyroid cancer, and inclusion of BRAF status modestly improves performance of the AMES, MACIS, TNM, and ATA risk scores. Likewise for thyroid papillary microcarcinoma (TPMC), a risk score incorporating BRAF status allowed identification of high-risk cancers that would not be identified by histology alone in a small study of 29 aggressive TPMCs matched to 30 nonaggressive cancers and validated in 40 others. Although PTC has a favorable prognosis with greater than 90% survival at 10 years, the BRAF V600E mutation puts patients at higher risk for recurrence, subjecting them to additional treatments and interventions, and likely causing worse quality of life, even if it does not cause decreased survival.
While knowledge of mutations in resected cancers improves prognostication, some have sought to apply molecular testing to prospective surgical decision making. Based on their results correlating BRAF + FNAs with higher recurrence risk even after correcting for unfavorable tumor characteristics, Xing and colleagues suggested that preoperative knowledge of BRAF status by FNA could help surgeons choose whether to perform prophylactic central neck dissection. The place for lymphadenectomy in well-differentiated thyroid cancer remains controversial. Some retrospective studies have suggested incremental improvements in recurrence and survival, but these are balanced against higher rates of hypocalcemia and nerve injury. Prospective studies to determine whether preoperative BRAF testing of FNA specimens is useful for predicting occult lymph node metastases have yielded conflicting results. One study (N = 51) found that BRAF positivity in excised tumors did not correlate with nodal metastases, but did not test for BRAF preoperatively and had a low rate of BRAF mutation (29%). A larger study (N = 148) found that BRAF + FNA specimens were significantly associated with occult lymph node metastases after prophylactic central neck dissection, and concluded that BRAF status may be helpful in the decision whether to perform nodal dissection in a clinically node-negative neck. Unless a prospective randomized trial with long-term follow-up is conducted, the optimal extent of nodal dissection will likely remain uncertain.
Chemotherapeutics Targeting BRAF and MAPK
Multiple proteins in the BRAF-MAPK pathway have been targeted for the treatment of thyroid cancer, and these pathways remain among the most active areas of pharmaceutical research. In 2008, a phase I trial showed promise for selumetinib/AZD6244, a selective MEK1/2 inhibitor, which included a patient with metastatic MTC with a prolonged period of stable disease. In BRAF -mutated metastatic melanoma, a phase III trial of the MEK inhibitor trametinib demonstrated significantly prolonged progression-free and overall survival in the treatment group. More recently, researchers completed an early phase trial of selumetinib in metastatic, radioiodine-refractory thyroid cancer. Applying the preclinical observation that treatment with MEK inhibitors seemed to restore thyroid differentiation and iodine uptake in thyroid cells, they treated 20 patients with well-differentiated, metastatic, radioiodine-refractory, follicular-origin thyroid cancer with selumetinib. After 4 weeks iodine uptake was reassessed with 124 I positron emission tomography scans, and 12 of 20 patients had increased uptake. Of these patients, 8 had enough uptake to justify treatment with 131 I, and of these, 5 had partial responses and 3 had stable disease 6 months after treatment. Cancers with RAS mutations responded best to selumetinib (5 of 5), whereas only 1 of 9 cancers with BRAF V600E had enough uptake to warrant treatment with 131 I. Although limited in size, this rapid translation of cell culture and mouse data to human clinical trials may herald a new approach to kinase-inhibitor treatment in thyroid cancer.
Sorafenib, a multikinase inhibitor, has some activity in thyroid cancer, but early human use has shown low response rates. In 2008, sorafenib was shown to more potently inhibit thyroid cancer cells harboring the RET/PTC1 gene rearrangement than those with BRAF V600E. In a phase II trial of sorafenib for ATC, only 2 of 20 patients showed a partial response, and another 5 had stable disease; median progression-free survival was only 1.9 months. Despite these modest results, there is growing evidence that response to treatment might be improved by prospective tumor genotyping, allowing improved selection of patients most likely to respond. In a trial of another multikinase inhibitor, Piscazzi and colleagues analyzed results according to gene expression, finding no relationship between response to sunitinib treatment and tumor expression of traditional sunitinib targets VEGF receptor (VEGFR), c-KIT, and PDGF receptor (PDGFR). Response did correspond to expression of mutant RET , whereby mutation-positive patients enjoyed higher response rates than those with BRAF or RAS mutations, providing further enthusiasm for prospective genetic profiling of thyroid cancers in future trials. Yet another multiple tyrosine kinase inhibitor, cabozantinib/XL184, showed improved progression-free survival of 11.2 months, versus 4.0 months with placebo, in a phase III trial of the drug in progressive MTC. Cabozantinib was approved by the Food and Drug Administration for the treatment of advanced MTC in November, 2012.
Kinase inhibitors specifically targeting BRAF have also been developed. One such is PLX4720, which inserts into the adenosine triphosphate (ATP)-binding site of mutant BRAF, stabilizing its inactive state. In vitro, the inhibitor blocks phosphorylation of downstream BRAF targets and leads to upregulation of suppressed markers of thyroid differentiation. In a mouse model, Nehs and colleagues injected V600E ATC cells into mouse thyroids and then treated the animals with PLX4720. Treated mice had resectable tumors after 7 days and lived to the end point of 50 days, whereas untreated mice were found to have unresectable tumors at 7 days and were euthanized by day 35 because of tumor burden. To more closely mimic the advanced stage at which ATC usually presents, this group next started inhibitor treatment at 28 days after administration of tumor cells to allow metastatic disease to become established, and still demonstrated tumor regression. Based on these studies and data in melanoma with the similar but orally available BRAF inhibitor vemurafenib, Rosove and colleagues reported a complete response to vemurafenib in a critically ill patient with metastatic BRAF + ATC, providing clinical evidence of the promise of this approach in human ATC.
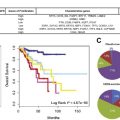
In one of the most encouraging inhibitor trials to date, a phase III, manufacturer-sponsored trial of the RET inhibitor vandetanib recently showed efficacy in patients with advanced MTC. Treatment with vandetanib was associated with median progression-free survival time of 30.5 months, versus 19.3 months for placebo (hazard ratio 0.46, 95% confidence interval 0.31–0.69), and objective response rates by RECIST criteria (Response Evaluation Criteria in Solid Tumors) of 45% versus 13% ( P <.001, with high placebo response rate attributable to 93% cross-over to open-label vandetanib treatment among patients who progressed on placebo). Mild toxicities were common and serious toxicities occurred, including grade 3 or 4 diarrhea, hypertension, and QTc prolongation in 11%, 9%, and 8%, respectively, of treated patients. These results suggest that this drug will play a role in the treatment of MTC in the future.
Translational Research in Thyroid Nodules
An area of persistent clinical interest is the thyroid nodule with indeterminate cytology by FNA. Around 30% of all nodules have indeterminate FNA results, and of these around 30% harbor malignancy. Because of the risk of malignancy, most patients with indeterminate nodules undergo surgery. Several novel methods have recently emerged to derive additional information from FNA specimens to select patients at low risk of malignancy who do not need surgery and to identify those likely to have cancer who will benefit from total thyroidectomy. McCoy and colleagues studied 670 patients at a single institution in cohorts before and after the introduction of routine molecular testing of all nonbenign thyroid FNA specimens. These investigators reported that testing for mutations in RET , RAS , BRAF , and PAX8/PPAR-γ (a fusion of the thyroid transcription factor PAX8 promoter with the peroxisome proliferator-activated receptor-γ1 gene, which is found in some follicular thyroid cancers ) identified mutations in 15% of indeterminate or nondiagnostic FNAs. Of 25 patients with positive molecular testing and no other indication for thyroidectomy, all were ultimately found to have some malignant changes, and 22 of 25 (88%) required total thyroidectomy based on current guidelines. With knowledge of the molecular testing results, 18 of these patients elected to undergo total thyroidectomy at their initial surgery. Concurrently, owing to the increased preoperative knowledge, the sensitivity of intraoperative frozen section dropped to only 1.7% and was abandoned at their institution. The investigators concluded that routine molecular testing (at an additional $104 per specimen) adds valuable knowledge, helps to select the correct initial surgery more often, and is cost-effective by limiting the need for later reoperation for completion thyroidectomy. Overall, detecting a known malignant mutation on thyroid FNA has a positive predictive value for malignancy of nearly 100% for BRAF , RET , or PAX8/PPAR-γ , and 74% to 87% for RAS , and these patients should undergo total thyroidectomy.
Although testing for mutations of known malignant potential can identify patients who should undergo total thyroidectomy, with its low negative predictive value it cannot rule out malignancy. An emerging approach to this challenge uses differences in microRNA (miRNA) expression to separate benign and malignant thyroid nodules. miRNA can distinguish benign from malignant thyroid FNA specimens with high accuracy; however, when applied to indeterminate nodules the negative predictive values remain below 90%, and are insufficient to recommend against surgery. Nevertheless, potential discovery of additional informative miRNA or improvements in classification algorithms make this a promising avenue of research.
Another strategy assesses differential mRNA expression by quantitative polymerase chain reaction (PCR). In 2012, a multicenter validation study of a commercially available gene-expression assay for indeterminate thyroid FNA specimens reported results from 265 patients who underwent thyroidectomy. The assay measures expression of 142 genes and uses a proprietary algorithm to classify specimens as benign or malignant. In this study, 32% of patients were ultimately found to have malignancy, and the gene expression classifier correctly identified 78 of these 85 (91.7%) as suspicious for malignancy. The negative predictive value of the test was 85% to 95%, depending on the Bethesda classification assigned to the specimen. These results were reported as evidence that the test could help avoid unnecessary thyroidectomies. At least one study funded by the company reported that the rate of surgery in indeterminate nodules classified as benign by the gene-expression test decreased to 7% among patients of participating endocrinologists, compared with 74% overall for indeterminate nodules before adoption of the test. Despite the promise of these reports, the authors of the present review believe that it is premature to decide against surgery based on the results of Alexander and colleagues. All data collection and analysis in both studies was performed by the manufacturer, and the validation study employed a relatively small sample size of 265 patients. As such, these results could represent a best-case scenario of the test’s performance. Furthermore, in the utilization study, the proportion of total tests classified as benign was not reported, making it impossible to determination the total rate of surgery. An industry-sponsored study claiming cost-effectiveness of this $3200 test used a cost model that assumed very high 30% and 44% complication rates for hemithyroidectomy and total thyroidectomy, and did not account for the costs and impact on quality of life of missed cancer diagnoses. Finally, while this test clearly adds information over cytology results alone, the unanswered question is whether negative predictive values of as low as 85% in the highest risk category (implying a 15% rate of malignancy) would be sufficient for most surgeons to recommend against surgery. A larger, independent validation of the test should be done, and studies of reduced thyroidectomy rates after application of the test must include appropriate follow-up to determine how many patients not having surgery based on a negative test result ultimately develop cancer or undergo thyroidectomy at a later time.
Until completion of such studies, the authors of the present review agree with the management algorithm of Nikiforov and colleagues for solitary thyroid nodules with indeterminate cytology, which was based on analysis of 1056 FNA specimens. Indeterminate FNAs have a cancer risk of 14% to 54% and should undergo molecular testing with a limited and less expensive panel ( BRAF , RAS , RET , and PAX8/PPAR-γ ). Patients with positive results should undergo total thyroidectomy because of the high risk of malignancy (87%–95%). Patients with follicular lesions or atypia of undetermined significance and negative testing have a risk of malignancy of 6% and may consider observation, repeat FNA, or diagnostic lobectomy, whereas those with follicular neoplasm/suspicion for follicular neoplasm or suspicion for malignancy have a risk of malignancy of 14% to 28% and should undergo diagnostic lobectomy.
Parathyroid/MEN1
Parathyroid abnormalities encompass both benign and malignant disease, and hyperparathyroidism is a feature of MEN1 and MEN2A syndromes. Parathyroid carcinoma remains exceedingly rare, but is strongly associated with the tumor-suppressor HRPT2/CDC73. Germline HRPT2 mutations cause familial hyperparathyroidism/jaw-tumor syndrome, and somatic mutation of HRPT2 is found in more than 75% of sporadic parathyroid carcinomas. Some patients with seemingly sporadic parathyroid carcinoma will be found to have germline HRPT2 mutations, making genetic testing of patients with parathyroid carcinoma potentially helpful by identifying related gene carriers who will benefit from serum calcium screening. Parafibromin, the protein product of HRPT2 , acts as a cell-cycle regulator in the Wnt pathway through interaction with β-catenin, and is involved in histone modification during transcription. Loss of immunohistochemical staining for parafibromin is highly suggestive of parathyroid carcinoma, and in the future may aid in the diagnosis of malignant parathyroid tumors.
Hyperparathyroidism (HPT) occurs in a minority of MEN2A patients, with the risk strongly influenced by the specific RET mutation present (see Table 1 ). The incidence of HPT in MEN2A is known to be 20% to 35%, and is much more common with mutations of codon 634, although HPT also occurs in 1% to 5% of patients with codon 609, 611, 618, and 620 mutations. By contrast, HPT is the most common manifestation of MEN1, with nearly 100% of carriers affected by the age of 50 years ( Table 3 ). The MEN1 gene was first mapped to chromosome 11 by linkage in 1988, and cloned in 1997. The menin tumor-suppressor protein encoded by MEN1 interacts with many different proteins including transcription factors and cell-cycle regulatory proteins, can bind DNA directly, and although it seems to play a role in chromatin remodeling and genomic stability, its exact function remains unclear. Unlike MEN2 mutations, which cluster at particular codons, MEN1 mutations are highly variable, with more than 1100 distinct germline mutations described and the most common occurring in only 4.5% of families (as opposed to 85% of MEN2A families having RET codon-634 mutations). Also unlike MEN2, in MEN1, individuals show similar manifestations of the disease within affected families, but have considerable variation between families, even those sharing the same mutation. Thus while genetic testing for MEN1 mutations is available, identifying carriers does not suggest a specific prophylactic surgical therapy, as in MEN2, but rather identifies those who require screening for development of different manifestations of the disease. Lairmore and colleagues found that genetic testing for MEN1 helped identify biochemical changes 5 to 10 years before the development of clinically apparent tumors, allowing for early surgical intervention in some cases. Those at risk for MEN1 by family history or confirmed through genetic testing should begin serum calcium screening before the age of 10 years to detect development of HPT. In sporadic HPT, keen attention to family history suggestive of MEN1 (pituitary adenoma, pancreatic neuroendocrine tumor, hyperparathyroidism, thymic carcinoid, cutaneous angiofibroma, ependymoma, nodular adrenocortical hyperplasia, or multiple lipomas) helps identify patients who may benefit from genetic testing and 4-gland exploration.