Figure 6.1
The incision may be placed just below the cricoid cartilage, conforming to the skin crease. If the patient is likely to require neck dissection, a higher incision on the cricoid cartilage is preferred rather than making an apron-shaped incision
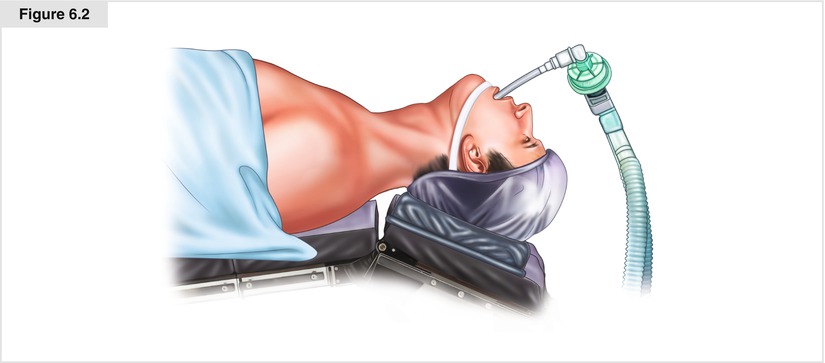
Figure 6.2
The patient’s neck is extended on the head plate of the operating table. A shoulder rest is preferred for best extension of the neck
6.6 Surgical Procedure
The skin should be incised with a knife. After the skin incision, most of the dissection is performed with electrocautery. Unipolar cautery is commonly used. Initially, the subcutaneous tissue should be incised with pointed electrocautery, and subsequently a flat electrocautery should be used. The skin and subcutaneous tissue are incised. The platysma is then incised. There is hardly any platysma in the midline, and the platysma can be seen as a well-developed muscle in its lateral potion. The upper flap should be raised under the platysma by elevation with skin hooks where an essentially avascular plane can be raised under the platysma (Fig. 6.3). The upper flap should be raised up to the thyroid notch, and the lower flap taken down to the sternal notch. At this time, the midline fasciae is exposed, and this should be incised with electrocautery. Occasionally, there are communicating veins between the two anterior jugular veins, which should be cauterized, ligated, or divided with a harmonic scalpel or LigaSure energy device. The strap muscles should be separated in the midline. Opening this area can be compared to opening a “gift box,” with the thyroid situated under the gift wrap, covered by strap muscles and the fascia [4]. The anterior strap muscles (sternohyoid) can be easily separated and pulled laterally. Rarely, this may require transection for better exposure if the tumor is adherent to the strap muscles. There is a debate about cutting of the inner strap muscle (sternothyroid). When necessary, we generally prefer to cut the inner strap muscle superiorly both from an oncologic point of view and for better exposure of the superior thyroid pole. The sternothyroid may be cut above and below for better exposure of a thyroid tumor. At this time, the dissection is performed on the lateral side of the thyroid. The middle thyroid vein is identified, and is clamped, ligated, and cut, or an energy device used. Gentle dissection may be performed in the inferior portion to expose the tracheoesophageal groove in this area.
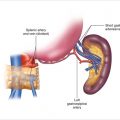
The upper pole is now exposed. A clamp is placed on the upper portion of the thyroid lobe, and the thyroid lobe is pulled inferiorly and laterally; this opens up the medial aspect of the superior thyroid vessels known as Joll’s triangle. There are always tiny veins in this area from the superior thyroid vein, which should be cauterized. At this juncture, the superior thyroid vessels are pulled inferiorly and laterally, which may expose the superior laryngeal nerve (Fig. 6.4). If the nerve can be identified, it is pushed up and medially and preserved carefully by ligating the superior thyroid vessels inferior to the superior laryngeal nerve. Quite often the superior laryngeal nerve may be difficult to identify, and the superior thyroid vessels should be clamped, ligated, and cut or an energy device to divide it very close to the upper pole of the thyroid. There are always minor veins with multiple branches from the superior thyroid vessels, which should be carefully ligated or cauterized. At this time, the dissection continues from the superior pole on the lateral side. On the right side, due consideration should be given at this time to evaluate if the patient has a nonrecurrent laryngeal nerve. The dissection is performed on the lateral side of the thyroid gland, exposing the entire thyroid lobe and pulling it medially. We generally prefer finger retraction of the thyroid lobe and dissection into the paratracheal area; however, some surgeons prefer using an Allis or Lahey clamp on the thyroid, although this may cause capsular trauma and bleeding from the thyroid gland. The surgeon’s hand-retraction probably gives the best nontraumatic exposure of this area. The dissection may be continued in the medial aspect of the superior thyroid pole, where the pyramidal lobe may be identified. There is always a tiny vein in front of the cricoid cartilage, which should be ligated. This vein is important because if it is not identified it may cause postoperative bleeding when the patient coughs or bucks at the end of the surgical procedure. As the superior pole and the lateral aspect of the thyroid are exposed, the tracheoesophageal groove area should also be exposed. The parathyroid glands can be identified in the superoinferior portion of the thyroid gland in front of and behind the recurrent laryngeal nerve (Figs. 6.5 and 6.6). Occasionally, the parathyroid glands may be in the thyroid capsule, which requires careful dissection and separation of the thyroid from the parathyroid gland. Every effort should be made to carefully preserve the vasculature of the parathyroid gland, and separating them intact is important (Fig. 6.6) [5]. If a parathyroid gland appears to be devascularized, it should be auto-transplanted into the sternocleidomastoid muscle after confirming that it is parathyroid tissue on frozen section from a small biopsy. It is important to avoid implantation of lymph nodes or metastatic thyroid carcinoma. As the dissection continues on the lateral aspect of the thyroid, the area of the tuberculum Zuckerkandl is identified.
The recurrent laryngeal nerve is generally posterior to the tuberculum Zuckerkandl, which can be easily identified by the retraction of the tuberculum. The recurrent laryngeal nerve may be identified in three distinct areas. First, in the tracheoesophageal groove and traced in its entirety up to the cricoid cartilage. This is where it is more commonly found when evaluating suspicious lymph nodes. The second region where the nerve can be found is its crossing on the inferior thyroid artery. However, it must be remembered that in approximately a quarter of the patients, the nerve may be in front of the inferior thyroid artery and not behind it (Fig. 6.7). Our current practice is to find a short segment of the nerve near the ligament of Berry, behind the tuberculum Zuckerkandl (Fig. 6.8).
The dissection in the region of ligament of Berry and tuberculum Zuckerkandl is quite critical, and meticulous dissection and mobilization of the thyroid should be performed. The thyroid gland is generally mobilized medially, although excessive medial retraction may cause traction injury to the nerve. This should be kept in mind at the time of transecting the ligament of Berry. Invariably, there are tiny vessels in the ligament of Berry that may cause bleeding. The bleeding should be controlled very carefully, either with electrocautery or with bipolar cautery with a fine tip forceps. If a tie is to be placed on this bleeding vessel, it should be with Vicryl or chromic catgut, which are dissolving suture materials. The inferior thyroid veins, which are generally multiple and some of which may be parallel to the recurrent laryngeal nerve or the trachea, should be carefully ligated. One may find an arteria thyroidea ima vessel in this region, which generally runs from the brachiocephalic trunk along the trachea to the inferior aspect of the thyroid. The hemostasis of inferior thyroid veins is critical, as these veins may retract into the mediastinum, causing bleeding that is difficult to control. After mobilization of the entire lobe, the dissection continues on the surface of the trachea in the pretracheal plane. The extent of thyroidectomy will depend upon the disease process and the personal philosophy of the operating surgeon. Occasionally, a small remnant of thyroid tissue is left behind in an effort to protect the parathyroids and the recurrent laryngeal nerve. However, generally we perform extracapsular true total thyroidectomy in patients with suspected malignancy. In spite of this, a small portion of thyroid tissue may be left behind near the ligament of Berry, the superior pole, and the pyramidal lobe area.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree