Goiter
Graves disease
Hyperthyroidism
Hypothyroidism
Thyroid cancer
Thyroid nodules
TSH
The thyroid gland forms during the first trimester of fetal development from the medial and lateral anlagen and follows a complex migratory path.
Insufficient migration can lead to a lingual thyroid. Lingual thyroids may cause obstruction of the upper airway or develop thyroid cancer, but are not routinely removed if these complications do not develop.
Partial nonclosure of the migratory tract can lead to a thyroglossal duct cyst; thyroglossal duct cysts are usually benign and not of clinical significance unless infection of the cyst occurs, which may require surgical intervention.
Postnatally to age 8 years, thyroid growth is similar and steady in males and females.
During puberty, there is a more than four-fold increase in thyroid volume, which correlates not only with age and gender, but also with weight, height, body mass index, and pubertal stage.1
By the end of puberty, the average weight of the female thyroid is 14.4 g, and for the male, it is 16.4 g.2
Despite the significant increased growth of the thyroid during puberty, levels of free thyroxine (fT4) and TSH decrease from age 1 year to adulthood.
There is an increase in thyroid disorders of both structure and function during puberty.
Trisomy 21
Turner syndrome
Klinefelter syndrome
Autoimmune disorders (personal or family history)
Rheumatoid arthritis
Diabetes mellitus type 1
Celiac disease
Autoimmune polyglandular syndrome
Computerized axial tomogram (CT) scan with iodinated contrast
Kelp or seaweed supplements
Amiodarone which contains iodine
Lithium
Valproate
Amiodarone
Interferon
Thionamides
Interleukin-2
Tyrosine kinase inhibitors
Dopamine
Dobutamine
Glucocorticoids
Bexarotene
Cowden syndrome
Bannayan-Riley-Ruvalcaba syndrome
Gardner syndrome
Multiple endocrine neoplasia (MEN) type 2
Familial medullary thyroid cancer
TABLE 12.1 Clinical Effects of Thyroid Hormone
Clinical Effect
Hyperthyroidism
Hypothyroidism
Height velocity
Increased
Decreased
Weight
Decreased
Increased
Temperature
Increased in extreme cases
Decreased in extreme cases
Hair and skin
Oily and hair loss diffusely
Pretibial myxedemaa
Dry
Myxedema generalized
Fingernails
Ridges
Brittle
Bowels
Increased frequency
Constipation
Cardiac
Increased heart rate
Atrial fibrillation
Decreased heart rate
Menstruation
Lighter flow, irregular menses
Heavier flow, irregular menses
Skeleton
Bone loss
Advanced bone age
Normal bone density
Delayed bone age
Blood pressure
Systolic hypertension
Increased mean arterial pressure
Diastolic hypertension
Eyes
Stare, lid lag, dry eye exophthalmosa
Periorbital edema
Reflexes
Normal
Delayed relaxation
Cognition
Decreased school performance
Decreased school performance
a Associated specifically with Graves Hyperthyroidism.
Familial papillary thyroid cancer (PTC)
Carney complex type 1
Radiation treatment for childhood cancers
Fallout from nuclear reactor accidents
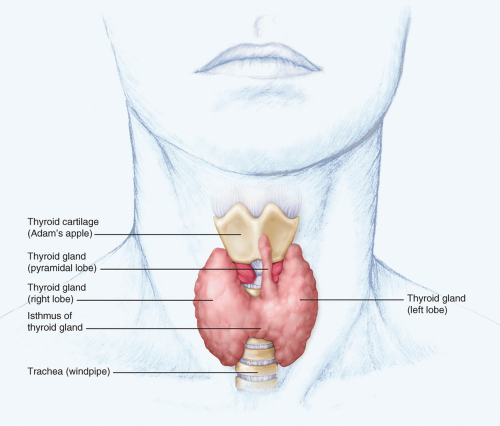
Inspection, palpation, and imaging by ultrasound, CT, or magnetic resonance imaging all provide information about the physical aspects of the thyroid gland.
Inspection (see Fig. 12.1) and palpation are best evaluated while the patient swallows, causing the thyroid to elevate. Ultrasound of the thyroid is the preferred imagine modality to assess thyroid gland structure. It allows for quantification of the size of the gland or a lesion, so it can be monitored and compared with a subsequent ultrasound. In addition, it can also identify features that aid in clarifying the diagnosis of thyroid enlargement:
Autoimmune thyroiditis
Diffuse heterogeneity is present.
Nodule(s)
Low risk for cancer:
Hyperechoic
Peripheral vascularity
Spongiform appearance
Resembles puff or Napoleon Pastry
Comet-tail shadowing
Increased risk for cancer:
Hypoechoic
Microcalcifications
Central vascularity
Irregular margins
Incomplete halo
Nodule is taller than wide
Significant growth of nodule
TSH is the most sensitive assay of thyroid function in steady-state situations.
When TSH is abnormal, or if a central (hypothalamic or pituitary) abnormality is suspected, fT4 is also measured.
Total T3 is helpful when TSH is suppressed to identify and monitor response to antithyroid treatment in Graves disease.
In inflammatory thyrotoxicosis due to release of preformed thyroid hormone, the ratio of T4:T3 is preserved (4:1).
When acute illness is a factor, rT3 levels can be measured, which if elevated suggests that the changes observed in TSH, early suppression followed by elevation, are associated with the acute illness and recovery phases. A “sick-euthyroid” pattern may also be reflected by a low total T3, a pattern common in AYAs with eating disorders.
The most specific thyroid antibody is thyroid-stimulating antibody (TSAb), which is typically measured in hyperthyroid patients to confirm Graves disease.
Thyroid peroxidase (TPO) antibody is the most sensitive antibody to detect autoimmune thyroid disease and can be elevated in patients with either hypo- or hyperthyroidism. It is most helpful in subclinical hypothyroidism where fT4 is normal and there is a mild TSH elevation <10 mU/L, where the presence of elevated TPO antibodies is associated with higher risk for overt hypothyroidism and can be an indication for thyroid hormone treatment.
Quantification of uptake in hyperthyroidism where increased uptake is consistent with Graves disease, while decreased uptake suggests either exogenous thyroid ingestion or release of preformed thyroid hormone associated with inflammatory thyroiditis
Assessment of pattern of uptake to determine if a nodule takes up tracer and suppresses the rest of the gland, uptake indicating a toxic nodule, or if a nodule takes up less tracer than the rest of the gland indicating that the nodule requires further evaluation by fine-needle aspiration
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree