Thyroid Disorders
M. Regina Castro
Hossein Gharib
EVALUATION OF THYROID FUNCTION
Thyrotropin
Thyroid-stimulating hormone (TSH), or thyrotropin, is the single most useful measurement in the evaluation of thyroid function. Produced by the anterior pituitary, TSH stimulates the thyroid gland to produce the thyroid hormones thyroxine (T4) and triiodothyronine (T3) and its secretion is, in turn, closely regulated by the serum concentrations of these hormones. This measurement has been recommended by the American College of Physicians as a screening test in women over the age of 50 years, in whom the prevalence of unsuspected hypothyroidism appears to be significant [1]. TSH determination every 5 years in women and men over the age of 35 is a cost-effective measure to detect early thyroid failure; its diagnostic yield increases with advancing age and is higher in women than men [2]. In hospitalized patients, however, screening with TSH leads to many false-positive results [3]. Although normal serum TSH reference range has long been considered to be 0.5 to 5.0 mIU/l, some authors have argued that a narrower reference range (0.5-2.5 mIU/l) more accurately reflects a true euthyroid state in the absence of other confounders, such as thyroid peroxidase antibodies (TPOAbs), medication effect, etc. [4, 5]. However, this has not been universally accepted [6]. TSH distribution progressively shifts toward higher concentrations with advancing age. Because of this, age-specific range for TSH should be used to avoid overestimating the prevalence of subclinical hypothyroidism (SCH) [7]. Limitations of TSH testing include the following:
Central hypothyroidism. Measurement of TSH alone may be misleading in these patients. Central hypothyroidism is suspected when free T4 (FT4) values are low and the TSH level is low, normal, or less elevated than would be expected in a patient with hypothyroidism [8]. In these patients, secreted TSH has reduced biologic activity but remains immunoactive in the assay [9].
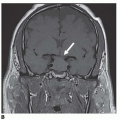
Thyrotoxicosis due to inappropriate TSH secretion. Measurement of TSH alone in patients with a TSH-secreting pituitary adenoma may be misleading. High levels of serum FT4 and T3, along with inappropriately normal or
elevated serum TSH levels, an elevated a-subunit, and finding of a pituitary adenoma on magnetic resonance imaging (MRI) will confirm the diagnosis.
Patients treated for hyperthyroidism, in whom serum TSH levels may remain suppressed for 3 months or longer after patient is clinically euthyroid. Because of this delay in recovery of the pituitary—thyroid axis, during the first several months of treatment, clinical decisions should be based on measurement of FT4 and T3, until steady-state conditions are met.
Drugs that affect serum TSH concentrations. Dopamine inhibits TSH and can reduce TSH levels in hypothyroid patients into the normal range. Glucocorticoids may slightly reduce TSH into the subnormal range. Acute amiodarone use can transiently increase TSH concentration.
Patients with nonthyroidal illness [10] (see Section on Euthyroid Sick Syndrome).
Free Thyroxine
Thyroxine is extensively bound to plasma proteins, and only a very small fraction circulates in the free state. The free hormone fraction, however, determines its biologic activity, making its measurement diagnostically more relevant than the total serum level because of the many binding protein abnormalities that can alter total thyroid hormone levels, independent of thyroid status. Although many methods of estimation of serum FT4 concentration are available, none—including equilibrium dialysis and ultrafiltration, regarded as the standard criterion or reference methods—gives a true indication of the effects of binding competitors that inhibit binding of T4 to thyroxine-binding globulin [11].
Total Thyroxine and Triiodothyronine
Serum total T4 and T3 values reflect not only thyroid hormone production but also serum levels of thyroid hormone—binding proteins. Discrepancy between normal serum free and high total thyroid hormone concentrations usually reflect elevated levels of binding proteins, a condition commonly referred to as “euthyroid hyperthyroxinemia.” T3 estimation is most useful when FT4 values are normal and TSH levels are suppressed (T3 toxicosis and subclinical hyperthyroidism) [12]. In euthyroid patients with acute medical illness, low T3 levels may reflect decreased peripheral conversion of T4 to T3. A high T3:T4 ratio (>20 ng/μg) suggests Graves disease as the underlying cause of hyperthyroidism.
Thyroid Autoantibodies
The test for TPOAbs is the most sensitive measurement for autoimmune thyroid disease. When it is measured by a sensitive assay, over 95% of patients with Hashimoto thyroiditis and 85% of patients with Graves disease have detectable levels of TPOAbs [12]. Also, the presence of TPOAbs is also predictive of future development of hypothyroidism, even in patients with normal serum TSH levels [13].
TSH receptor antibodies (TRAbs) can be found in most patients with Graves disease, although such determination is seldom necessary to confirm the diagnosis. TRAbs may be predictive of the risk of relapse of Graves hyperthyroidism after treatment with antithyroid drugs (ATDs) [14]. TRAbs are also useful in predicting fetal and neonatal thyroid dysfunction in pregnant women with a history of autoimmune thyroid disease [15].
Thyroglobulin antibody (TgAb) measurement is used primarily as an adjunct test to serum thyroglobulin (Tg) in the follow-up of patients with differentiated thyroid cancer because even very low levels of these antibodies can interfere with Tg determination causing falsely low or high values [16]. The sudden rise or appearance of TgAbs in a previously negative TgAb patient may be the first indication of recurrence [12].
Thyroglobulin
Thyroglobulin is the precursor of thyroid hormone synthesis and is present in the serum of all unaffected people. Serum thyroglobulin (Tg) concentrations reflect three factors: the mass of differentiated thyroid tissue; any physical damage or inflammation of the thyroid gland; and the level of TSH receptor (TSHR) stimulation, given that most steps in Tg biosynthesis and secretion are TSH dependent [17]. An elevated Tg level is a nonspecific indicator of thyroid dysfunction. Tg is helpful in distinguishing factitious hyperthyroidism, resulting from exogenous thyroid hormone administration and from endogenous hyperthyroidism, because in the former case, serum Tg levels are usually low, whereas in the latter, serum Tg concentrations are typically increased. Tg measurement is primarily used as a tumor marker in the follow-up of patients with differentiated thyroid cancer after thyroidectomy to detect recurrent or metastatic disease. Serum Tg, measured during TSH stimulation —endogenous TSH after thyroid hormone withdrawal or recombinant human TSH (rhTSH)—is more sensitive for detecting differentiated thyroid cancer than basal Tg measured during levothyroxine (LT4) suppressive therapy [18].
Tg measurement has also been used in recent years to confirm the presence of metastatic thyroid cancer in needle washouts after fine-needle aspiration (FNA) biopsy of suspicious cervical lymph nodes (CLNs) in patients with a history of thyroid cancer [19, 20]. It has been found to be more sensitive than FNA cytology of lymph nodes (LNs) and has the advantage of not being affected by the presence of anti-Tg antibodies in the serum [19].
THYROID IMAGING
Ultrasonography
Ultrasonography (US) is the test of choice for evaluation of thyroid size and morphology; it is the most sensitive test in the detection of thyroid nodules, capable of detecting lesions 2 to 3 mm in diameter. It is also useful in guiding FNA biopsy of palpable and nonpalpable thyroid nodules. US features predictive of malignancy in thyroid nodules include: hypoechogenicity; presence of microcalcifications; a thick, irregular, or absent halo; irregular margins; regional adenopathy; and intranodular vascular spots [21, 22]. US cannot, however, unequivocally distinguish benign from malignant nodules, and FNA is needed to confirm the diagnosis. US is also used for evaluation of regional LNs, both in the preoperative assessment and in the postoperative surveillance of thyroid cancer. It has been found in some studies to be more sensitive than other surveillance modalities such as Tg measurement and whole-body scanning (WBS) [23]. The major limitations of US are the high degree of observer dependency and its inability to visualize retrotracheal, retroclavicular, or intrathoracic lesions.
Scintigraphy
Scintigraphy is the standard method for functional imaging of the thyroid, and two isotopes most commonly used are iodine 123 (123I) and 99mTc-pertechnetate; the latter has the advantage of lower cost and greater availability. 99mTc scanning provides a measure of the iodine-trapping function in the thyroid or in a nodule within the gland. Thyroid scanning is commonly used to demonstrate that a palpable enlargement represents an entire lobe rather than a nodule; localize functional thyroid tissue; identify the cause of hyperthyroidism: homogeneously increased uptake in Graves disease, irregular uptake in multinodular goiter or thyroid nodules; identify functioning thyroid nodules: because “hot” or hyperfunctioning nodules are rarely malignant, such finding would obviate the need for FNA biopsy; and follow the evolution of characteristics of nodular goiter [24].
Computed Tomography
Computed tomography (CT) scans are useful in the evaluation of thyroid cancer recurrence, especially in delineating the extent of retrosternal involvement and defining the presence and extent of lymph node (LN) metastases, tracheal invasion, compression or displacement, and vascular invasion. CT is also helpful in assessing tumors not clearly arising from the thyroid and bulky tumors with possible invasion of local structures. CT is less sensitive than US in detecting intrathyroidal lesions.
Radioiodine Uptake
The main role of radioiodine (RAI) uptake is in the evaluation of hyperthyroidism, to distinguish subacute or silent thyroiditis from toxic goiter, to provide data to determine whether RAI therapy is feasible, and, if so, to aid in the dose calculation. Thyroid uptake reflects a combination of iodine transport into the thyroid follicular cells, its oxidation and organification, and its release from the thyroid. Increased uptake is usually seen in association with hyperthyroidism; Hashimoto thyroiditis; iodine deficiency; subacute, silent, or postpartum thyroiditis in the recovery phase; choriocarcinoma and hydatidiform mole; and during treatment with lithium carbonate. Decreased uptake occurs after treatment with iodinecontaining substances; in the thyrotoxic phase of subacute, silent, or postpartum thyroiditis; Hashimoto thyroiditis with widespread parenchymal destruction; thyroid agenesis, or after therapeutic ablation; and with the use of ATDs [24].
131I Whole-Body Scanning
131I WBS is used early in the diagnostic work-up of patients with suspected recurrent or metastatic thyroid cancer. Withdrawal of thyroid hormone therapy and a low iodine diet have been traditionally used to raise TSH concentration and increase uptake by thyroid tissue. Its sensitivity varies widely between studies, averaging 50% to 60%, depending on the dose of the isotope used, and site of tumor location, being highest for bone and lung, and lowest in LN metastases [25]; its overall specificity is high (90%—100%) [26]. When used in combination with Tg measurement after TSH stimulation, its sensitivity increases substantially, detecting up to 93% of cases with disease or tissue limited to the thyroid bed and 100% of cases with metastatic disease [18]. More recently, rhTSH has been used effectively to stimulate RAI uptake for WBS in patients with suspected recurrent thyroid cancer [27], and results have been comparable to those obtained after thyroid hormone withdrawal [28].
18F-Fluorodeoxyglucose Positron Emission Tomography
This imaging modality has been found to be most useful in patients with suspected recurrent or metastatic thyroid cancer, in whom other imaging modalities, such as131I WBS, have failed to localize the tumor [29]. Its sensitivity in such cases approaches 94% and its specificity 95% [30]. It is particularly helpful in patients with Hürthle cell carcinomas, in whom one study found it to be more sensitive than WBS [31].18F-Fluorodeoxyglucose positron emission tomography (FDG-PET) is especially useful in evaluating patients with elevated Tg levels and normal RAI WBS (scan negative, Tg positive). When combined with CT, it is a more sensitive method in the follow-up of thyroid cancer recurrence or metastases, particularly in those with negative WBS [32].
HYPERTHYROIDISM
Definition
Hyperthyroidism is a syndrome that results from the metabolic effects of sustained excessive circulating concentrations of thyroid hormones, T4, T3, or both. Subclinical hyperthyroidism refers to the combination of undetectable serum
TSH concentration and normal serum T3 and T4 concentrations, regardless of the presence or absence of clinical symptoms.
TSH concentration and normal serum T3 and T4 concentrations, regardless of the presence or absence of clinical symptoms.
Etiology
Hyperthyroidism may result from endogenous hormone overproduction alone or in combination with secretion of thyroid hormones or may be iatrogenic, as a result of administration of thyroid hormones or other drugs capable of inducing thyroiditis. The most common causes of endogenous hyperthyroidism include Graves disease, toxic multinodular goiter, toxic adenoma, and thyroiditis. Subacute thyroiditis can present in a painful (granulomatous) form, viral in origin, and a painless form, which may occur sporadically, or more commonly in the postpartum period. In this condition, a high prevalence (50%—80%) of TPOAbs in patients’ sera, evidence of lymphocytic infiltration of the gland, and frequently in association with other autoimmune diseases, suggests an autoimmune etiology. Exogenous thyroid hormone, given as suppressive therapy for thyroid cancer or benign thyroid nodules, or due to overreplacement in hypothyroid patients, or surreptitious use in others, may result in overt or subclinical hyperthyroidism.
Epidemiology
Graves disease accounts for between 60% and 80% of patients with hyperthyroidism. It is up to 10 times more common in women, with highest risk of onset between the ages of 40 and 60 years. Its prevalence is similar among whites and Asians and lower among blacks [33]. Autonomous adenomas and toxic multinodular goiter are more common in Europe and other areas of the world where residents are likely to experience iodine deficiency; their prevalence is also higher in women and in patients older than age 60 years.
Pathophysiology
Graves disease is an autoimmune disorder in which autoantibodies bind to and stimulate the thyroid stimulating hormone receptor (TSHR), resulting in increased intracellular cyclic adenosine monophosphate (cAMP) levels with subsequent thyroid growth, goiter formation, and increased thyroid hormone synthesis and secretion. With the use of more sensitive assays, these antibodies have been found in over 90% of patients with Graves disease. The pathogenesis of toxic nodular goiter is an area of active investigation. Thyroid autonomy has been postulated as the main pathogenic mechanism in toxic adenomas and is thought to be due to somatic mutations that constitutively activate the cAMP cascade. Such mutations have been clearly described [34], and in some cases of multinodular goiter, several mutations have been documented in the same patient. Other growth factors, iodine intake, and immune mechanisms may also contribute to the pathogenesis of toxic multinodular goiter.
Diagnosis
Classic manifestations of hyperthyroidism include nervousness, irritability, tremor, fatigue, tachycardia or palpitations, heat intolerance, and weight loss, often despite increased appetite. Atrial fibrillation, cardiac failure, and weakness are also common in older patients. In addition to these symptoms, Graves disease usually presents with a finding of a firm, diffuse goiter in up to 90% of patients, ophthalmopathy in about 50%, and in 1% to 2% a localized dermopathy over the anterolateral aspects of the shin [33]. In patients with toxic adenoma, a palpable nodule is often found on clinical examination, whereas in toxic multinodular goiter, a firm heterogeneous goiter of variable size is more common. Some patients with multinodular goiters may have retrosternal extension. Patients with toxic adenomas or multinodular goiters may have few or no clinical symptoms and may be diagnosed only on the basis of laboratory findings. Subacute (granulomatous)
thyroiditis may present with an exquisitely tender thyroid gland, often preceded by a viral upper respiratory infection, or in its more common, painless form, seen in the postpartum period, present with transient hyperthyroidism, followed by a variable period of hypothyroidism and subsequent spontaneous resolution.
thyroiditis may present with an exquisitely tender thyroid gland, often preceded by a viral upper respiratory infection, or in its more common, painless form, seen in the postpartum period, present with transient hyperthyroidism, followed by a variable period of hypothyroidism and subsequent spontaneous resolution.
Laboratory findings in hyperthyroidism are summarized in Table 2.1. Suppressed TSH and elevated FT4 and FT3 levels are seen in overt hyperthyroidism, but in subclinical hyperthyroidism, serum FT4 and FT3 concentrations are typically normal. When Graves disease is suspected but the diagnosis remains uncertain, measurement of TRAb may be helpful. Patients with symptoms of hyperthyroidism, elevated FT3 and FT4 levels, and normal or elevated TSH (inappropriate TSH secretion) may have a pituitary TSH-secreting tumor, or selective pituitary resistance to thyroid hormone. Similar findings, in the absence of signs or symptoms of hyperthyroidism, may be seen in syndromes of generalized resistance to thyroid hormone. RAI uptake and scan are useful in determining the etiology of hyperthyroidism. Increased uptake in a homogeneous pattern is seen in Graves disease, whereas in subacute thyroiditis and hyperthyroidism due to exogenous thyroid hormone administration, the uptake is usually low. Patients with toxic adenomas demonstrate a localized area of increased uptake, whereas in multinodular goiter, uptake may be normal but the pattern heterogeneous.
Treatment
Antithyroid Drugs
Antithyroid drugs (ATDs) are the treatment of choice for Graves disease in most countries in the world. The most commonly used in the United States are methimazole at doses from 10 to 40 mg once daily and propylthiouracil (PTU) in doses starting at 100 to 150 mg every 8 hours. PTU is no longer a first-choice drug because of recent reports of severe hepatotoxicity. When treating hyperthyroidism, the lowest dose needed to achieve and maintain clinical euthyroidism should be used because higher doses have not been shown to decrease relapse rates but may increase frequency of adverse effects [35]. Methimazole has the advantage of lower toxicity [36] (particularly when used in lower doses) and longer half-life, allowing single daily dosing, which usually results in increased adherence and more rapid decline in thyroid hormone levels, and is now recommended as the firstline ATD in most patients, whereas PTU is preferred during the first trimester of pregnancy since it is thought to be less likely to cross the placenta and because methimazole has been associated with certain rare congenital anomalies, such as choanal atresia and aplasia cutis [37]. Their major disadvantage is the high incidence of relapse of hyperthyroidism (up to 60%) after discontinuation of therapy. Optimal duration of therapy is between 12 and 18 months [38]. Prolonging treatment beyond 18 months does not seem to provide additional benefits [39, 40]. Longterm treatment appears to be safe [41] and a reasonable option for patients whose hyperthyroidism can be controlled with a low dose of these drugs [42].
Antithyroid Drugs plus LT4
A study from Japan reported a significant reduction in relapse (from 35% to 2%) with the addition of LT4 after 6 months of treatment with methimazole (block-replace regimen), and continuing this drug for 3 years after methimazole was stopped [43]. A subsequent study failed to confirm these findings [44]. The titration (low dose) regimen had fewer adverse effects than the block-replace (high dose) regimen and was equally effective. Continued thyroxine treatment following initial antithyroid therapy does not appear to provide any benefit in terms of recurrence of hyperthyroidism [39].
Table 2.1. Laboratory Tests for Hyperthyroidism | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Radioiodine
RAI has been used for treatment of hyperthyroidism for over six decades. It is the preferred treatment modality in the United States for patients with Graves hyperthyroidism, though used less commonly worldwide. RAI is appropriate treatment for Graves disease, toxic nodules, and toxic multinodular goiters [46]. It is effective and safe and significantly reduces thyroid volume, although patients with large goiters and severe hyperthyroidism may require several doses [47]. If RAI is used to treat Graves hyperthyroidism, sufficient radiation should be administered in a single dose (typically 10-15 mCi) to render the patient with Graves disease hypothyroid [37]. Most patients treated in this manner will require lifelong replacement with thyroid hormone. Some researchers believe that RAI therapy may transiently worsen Graves ophthalmopathy, a problem that can be prevented by administration of prednisone [48].
Surgery
Surgery is the treatment of choice for hyperthyroid patients with large goiters who have symptoms of compression, those with a coexistent suspicious thyroid nodule, for patients who have contraindications to or refuse medical therapy and RAI, and in pregnant women, whose symptoms cannot be controlled with, or who experience allergic reactions to, ATDs. It is safe and effective, with an overall success rate of 92% [49].
If surgery is chosen as the primary therapy for Graves disease, near-total or total thyroidectomy (TT) is the procedure of choice [37].
β-Blockers
β-Blockers are useful to control the adrenergic symptoms of hyperthyroidism and may be used as initial adjunctive therapy and discontinued after definitive therapy with ATDs, RAI, or surgery that have succeeded in controlling those symptoms. β-Blockers are safe and effective in the preoperative treatment of these patients and result in faster relief of hyperthyroid symptoms when compared with results of conventional preparation with ATDs [50]. They are strongly recommended in elderly patients with symptomatic hyperthyroidism and to other hyperthyroid patients with resting heart rates in excess of 90 beats per minute or coexistent cardiovascular disease.
HYPOTHYROIDISM
Definition
Hypothyroidism is a clinical syndrome that results from decreased thyroid hormone production and secretion, most commonly due to a disorder of the thyroid gland (primary hypothyroidism), and it is accompanied by elevated TSH levels. In less than 5% of patients, hypothyroidism results from hypothalamic or pituitary disease (secondary hypothyroidism), in which case, low serum thyroid hormone levels are accompanied by inappropriately normal, or even low, serum TSH levels. Subclinical hypothyroid (SCH) refers to a state in which increased serum TSH levels are accompanied by normal serum levels of FT3 and FT4, in a patient who is generally asymptomatic.
Etiology
Hashimoto thyroiditis is the leading cause of hypothyroidism. Treatment of thyrotoxicosis with131I or thyroidectomy, drugs such as lithium, and iodine-containing drugs or contrast agents can also lead to primary hypothyroidism. Central hypothyroidism results from hypothalamic or pituitary diseases.
Epidemiology and Pathophysiology
Hypothyroidism is one of the most common endocrine disorders. Its prevalence increases with age, and it is much more common in women than in men. Up to 2% of women between 70 and 80 years of age have overt hypothyroidism. The prevalence of SCH in women older than 50 years of age is higher, between 5% and 10% [1]. Hashimoto thyroiditis is an autoimmune disorder due to lymphocytic infiltration of the thyroid gland with subsequent atrophy of its follicular cells and fibrosis. Between 50% and 80% of patients with SCH test positive for TPOAbs. Conversely, the presence of positive TPOAbs, even in clinically euthyroid patients with no previous history of hypothyroidism, suggests an increased risk of future development of overt hypothyroidism [13].
Diagnosis
An elevated serum TSH level is the most sensitive test to diagnose primary hypothyroidism.
Patients with “SCH” have normal serum FT4 and T3 concentrations and are usually asymptomatic, whereas those with overt disease typically have low serum thyroid hormone levels and nonspecific symptoms, such as cold intolerance, weight gain, constipation, dryness of the skin, fatigue, and periorbital edema. Population screening for subclinical thyroid disease has not been universally accepted because the benefits of subsequent therapy have not been clearly established in prospective clinical trials. In central hypothyroidism, low serum thyroid hormone levels are seen along with inappropriately normal or low serum TSH levels. Pituitary MRI is recommended to exclude the presence of pituitary or hypothalamic disease or tumors.
Treatment
Levothyroxine
LT4 is the treatment of choice for hypothyroidism. The usual replacement dose is 1.6 to 4.2 μg/kg/d and should be titrated to maintain serum TSH levels within normal range [51]. Serum TSH levels between 0.5 and 2.0 mIU/l are generally considered the optimal target [12]. Whether SCH should be treated remains controversial. Some studies suggest that early treatment may improve cardiac function, reverse mild symptoms of hypothyroidism and lower serum lipids [52, 53], and improve memory [54], whereas others have shown no effect in total or low-density lipoprotein (LDL) cholesterol levels [55] or cognitive function [56].
LT4 plus Liothyronine (T3)
The use of combination LT4 and T3 in the treatment of hypothyroidism has been proposed as an alternative to LT4-only therapy, as a more physiologic form of thyroid hormone replacement [57]. Initial reports of improved mood and neuropsychological function with this combination [57] have not been confirmed by further controlled studies [58, 59, 60, 61], despite patients’ preference for this combination in some studies [62]. One study showed that combination therapy, when compared to LT4 alone, resulted in favorable changes in lipid profile but also in higher activation of bone resorption [61].
THYROID NODULES
Etiology
Autonomously functioning (toxic) adenomas may occur as the result of mutations in the TSHR or in the gene of the α-subunit of the G protein, leading to constitutive activation of the cAMP cascade and enhanced response to TSH. These mutations offer a growth and functional advantage to the cells affected, leading to development of an autonomously functioning nodule, inhibition of TSH secretion, and decreased
function of the rest of the gland. Toxic multinodular goiter results from gradual multiplication of autonomous follicles with varying degrees of function.
function of the rest of the gland. Toxic multinodular goiter results from gradual multiplication of autonomous follicles with varying degrees of function.
Epidemiology
Thyroid nodules are commonly seen in clinical practice. Their prevalence largely depends on the method of screening and the population evaluated. By palpation, the least sensitive method, their prevalence has been estimated around 4% [63]. Using high-resolution US, it has been reported to be as high as 68% [64, 65]. Autopsy data from patients with no history of thyroid disease have indicated a prevalence of 50% [66]. Increasing age, female gender, iodine deficiency, and a history of head and neck irradiation seem to consistently increase the risk of developing thyroid nodules. The Framingham study estimated the annual incidence rate, by palpation, at 0.09% [63]. This means that in 2012, approximately 310,000 new nodules will be discovered in the United States. Many patients with a single palpable nodule have additional nodules when examined with US [67]. The prevalence of thyroid cancer is similar in patients with single or multiple nodules [68].
Diagnosis
Thyroid nodules are usually discovered by palpation of the neck during routine physical examination. Most clinically palpable thyroid nodules are at least 1 cm in diameter. Nodules can also be incidentally diagnosed during US of the neck done for unrelated conditions (so-called incidentalomas). TSH is the best test to determine whether a palpable nodule is hyperfunctioning. If so, TSH will be suppressed and confirmation with scintigraphy is recommended, because the likelihood of malignancy in such nodules is very small.
Fine needle aspiration (FNA) biopsy of thyroid nodules is the most important, costeffective, and useful test in determining whether a nodule is benign or malignant. The mean sensitivity of FNA to detect thyroid cancer is 83% (65%—98%), its specificity 92% (72%—100%), and overall diagnostic accuracy 95% [69]. Its two major limitations are the inadequate or insufficient result and the suspicious or indeterminate cytologic findings, which occur in 15% and 20% of cases, respectively. Repeat US-guided biopsy may help overcome the first of these problems, but surgical excision is often needed to obtain a definitive diagnosis. Thyroid incidentalomas are very common. The incidence of cancer in such nodules ranges between 6% and 9% [21]. Prevalence of cancer was similar in nodules larger or smaller than 1 cm; irregular margins on US, microcalcifications, and intranodular vascular spots were independent predictors of malignancy, and 87% of cancers presented a solid hypoechoic appearance. FNA of nodules with at least one risk factor identified 87% of cancers [21, 22].
Treatment
Surgery
All thyroid nodules confirmed to be malignant and most found suspicious by FNA biopsy should be referred for surgical excision [70, 71]. The extent of the surgical procedure required is a matter of debate, with some authors advocating total or near-TT, and others favoring a more limited approach with lobectomy of the affected side. Benign thyroid nodules do not require surgery, unless they produce symptoms of compression or hyperthyroidism. Surgical excision is a reasonable option for patients with large or hyperfunctioning nodules, particularly if such nodules are associated with pressure symptoms [72].
Suppressive Therapy with Levothyroxine
Controversial evidence exists regarding the effectiveness of thyroid hormone suppressive therapy (THST) in reducing thyroid nodule size. One meta-analysis suggested an apparent therapeutic benefit of LT4 suppressive therapy in a subset
(20%—23%) of patients, with 1.9 to 2.5 times greater probability of achieving at least a 50% reduction in nodule size, when compared with placebo [73, 74]. Another meta-analysis found no statistically significant effect [75]. Predictors of response have not been identified. Suppressive therapy is not indicated for hyperfunctioning nodules. A controlled trial of suppressive therapy in nontoxic multinodular goiters showed a better than 13% decrease in thyroid volume in 58% of patients treated with LT4 compared with only 5% of those given placebo [76]. However, another randomized study comparing LT4 therapy with RAI in patients with nontoxic multinodular failed to show a benefit of LT4 suppressive therapy with regard to goiter size reduction but showed significantly increased bone loss [77]. Routine T4 suppressive therapy for benign nodule is no longer recommended, and potential adverse effects on the cardiovascular and skeletal systems should always be considered [77, 78].
(20%—23%) of patients, with 1.9 to 2.5 times greater probability of achieving at least a 50% reduction in nodule size, when compared with placebo [73, 74]. Another meta-analysis found no statistically significant effect [75]. Predictors of response have not been identified. Suppressive therapy is not indicated for hyperfunctioning nodules. A controlled trial of suppressive therapy in nontoxic multinodular goiters showed a better than 13% decrease in thyroid volume in 58% of patients treated with LT4 compared with only 5% of those given placebo [76]. However, another randomized study comparing LT4 therapy with RAI in patients with nontoxic multinodular failed to show a benefit of LT4 suppressive therapy with regard to goiter size reduction but showed significantly increased bone loss [77]. Routine T4 suppressive therapy for benign nodule is no longer recommended, and potential adverse effects on the cardiovascular and skeletal systems should always be considered [77, 78].
Radioiodine Therapy
RAI is effective in reducing thyroid volume by up to 60% in patients with nontoxic multinodular goiter and improving compressive symptoms in most [79]. It is successful in the treatment of nearly 90% of single toxic adenomas, although the relatively high doses usually required result in long-term hypothyroidism in 10% to 20% of cases [72]. It is also 80% to 100% effective in the treatment of toxic multinodular goiter, although often several treatments may be necessary [80]. RAI therapy is also effective in patients with sporadic nontoxic goiters, resulting in volume reductions of up to 45% in 1 year [81]. Pretreatment with a single dose of rhTSH has been successfully used in Europe as adjuvant to RAI, improving the efficacy of RAI by enhancing uptake in nontoxic thyroid tissue and allowing the use of lower doses of RAI, while still resulting in greater reduction of goiter size [82]. rhTSH also potentiates the effect of RAI allowing a major reduction of the RAI activity without compromising its efficacy, but it increases fivefold the risk of posttherapy hypothyroidism [83]. Moreover, because the side effects are dose dependent, they are rare following doses of rhTSH of 0.1 mg or less [84].
Percutaneous Ethanol Injection
Percutaneous ethanol injection (PEI) should be reserved for patients who cannot, or will not, undergo standard therapy. Local pain, risk of recurrent laryngeal nerve damage, and the need for repeat treatments make PEI unsuitable for routine treatment of solid thyroid nodules. However, this procedure appears to be safe and effective in the treatment of predominantly cystic nodules, resulting in substantial reduction of nodule volume and amelioration of cosmetic and compressive symptoms in up to 80% of patients [85, 86].
Laser Thermal Ablation (2B)
Ultrasound-guided laser thermal ablation (LTA) has emerged as an alternative therapeutic option in the management of patients with benign hypofunctioning thyroid nodules associated with compressive symptoms, who are poor surgical candidates or who refuse such intervention. This procedure has resulted in 45% to 60% reduction in nodule volume 6 months after treatment [87, 88]. The procedure requires considerable skill of the operator and is currently performed only in a few specialized centers.
THYROID CANCER
Definition and Classification
Thyroid carcinomas are malignant neoplasms of the thyroid epithelium. Papillary and follicular cancers, collectively termed differentiated thyroid cancer, arise from the follicular epithelial cells. Other follicular cell—derived thyroid cancers (FDTC)
include the oxyphilic, or Hürthle cell variant, and the undifferentiated, anaplastic carcinoma. Medullary thyroid cancer (MTC) originates from the parafollicular, calcitonin-secreting cells (C cells). Papillary thyroid cancer (PTC) is the most common histologic type in the United States, accounting for 80% of thyroid cancers, followed by follicular thyroid carcinoma (FTC) with 10% to 15%, and MTC with about 5%. Of MTC patients, 75% have sporadic disease and 25% present with the hereditary or familial forms (MEN 2A, MEN 2B, and familial MTC).
include the oxyphilic, or Hürthle cell variant, and the undifferentiated, anaplastic carcinoma. Medullary thyroid cancer (MTC) originates from the parafollicular, calcitonin-secreting cells (C cells). Papillary thyroid cancer (PTC) is the most common histologic type in the United States, accounting for 80% of thyroid cancers, followed by follicular thyroid carcinoma (FTC) with 10% to 15%, and MTC with about 5%. Of MTC patients, 75% have sporadic disease and 25% present with the hereditary or familial forms (MEN 2A, MEN 2B, and familial MTC).
Epidemiology
Thyroid cancer usually presents as a palpable nodule in the thyroid gland. Although thyroid nodules are very common, thyroid cancer is rare, constituting only 1% to 2% of all malignant neoplasms. It is three times more common in women than in men. Its annual incidence is approximately 0.5 to 10 per 100,000 in the world; some 40,000 new cases are diagnosed each year in the United States resulting in nearly 1,500 annual deaths [89]. Occult thyroid cancer, defined as any inapparent tumor found on a specimen by a pathologist, has been described in 0.5% to 13% of autopsy studies in the United States. Genetic (i.e., family history of thyroid cancer) or environmental factors (i.e., exposure to ionizing radiation) may be associated with the development of thyroid cancer in some populations. Nodule size larger than 4 cm, fixation to adjacent structures, enlarged regional LNs, vocal cord paralysis, rapid growth, and age younger than 15 years or older than 60 years predict a higher risk of malignancy.
Diagnosis
Fine-Needle Aspiration Biopsy
Most thyroid cancers present as a palpable thyroid nodule, often asymptomatic and are discovered during routine examination of the neck. FNA biopsy remains the single most accurate, reliable, and cost-effective test to diagnose thyroid cancer. Its sensitivity ranges between 65% and 98% (median 88%), specificity 72% to 100%, positive predictive value 46% to 100% (median 98%), negative predictive value 83% to 99% (median 97%), and its overall diagnostic accuracy is exceeds 95% [69, 90]. The two major limitations of FNA are the inadequate or insufficient result, in 15% of cases, and the suspicious or indeterminate cytologic findings, seen in about 20% of satisfactory specimens. In the first case, repeat FNA, under US guidance, may increase the biopsy yield and provide an accurate diagnosis. However, specimens in which repeat aspiration fails to provide an adequate sample should be referred for excision, particularly if nodules are large, solid, or have other features suggestive of malignancy [71]. Suspicious nodules should be excised, given that the rate of malignancy in these nodules may be as high as 30% [69].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree