Fig. 23.1
The process recommended for evaluation of a new thyroid nodule. Surgical treatments are presented based on fine-needle aspiration (FNA) diagnosis and not by histological cell type. TFTs thyroid function tests, CLND central lymph node dissection
Diagnostic Imaging
Ultrasound
The American Thyroid Association (ATA) recommends ultrasound evaluation of all palpable thyroid nodules and all those discovered by incidental imaging [1]. This allows for the confirmation of the presence of a nodule, the identification of additional nodules, and the measurement and characterizations of any lesions. As above, only nodules that are ≥1 cm in greatest diameter should prompt continued evaluation, as these are more likely to harbor clinically significant cancers. Patients with normal or high TSH levels should be evaluated with particular attention to sonographic features that suggest malignancy. These suspicious features include poorly defined margins, predominantly solid composition, microcalcifications, hypoechogenicity, taller-than-wide shape, cervical lymphadenopathy, and hypervascularity by Doppler. While none of these findings are definitive, the combination of hypoechogenicity, microcalcifications, and irregular borders in a solitary nodule was associated with a 30-fold increased risk of malignancy in a retrospective study [7].
Computed Tomography/Magnetic Resonance Imaging
There are very few indications for CT or MRI imaging in the initial workup of a thyroid nodule. If a patient has had a previous thyroid operation, these imaging techniques can help better delineate the thyroid bed. In addition, if there are signs of tracheal deviation or superior vena cava obstruction, three-dimensional imaging can evaluate the extent of deviation or substernal/mediastinal component of the tumor. Any CT imaging must be done without intravenous iodinated contrast, as this blocks iodine uptake by the thyroid and thereby would delay any adjuvant therapy with radioactive iodine should it be necessary [8].
Fine-Needle Aspiration
Fine-needle aspiration (FNA) has become the gold standard for thyroid nodule evaluation. It is the most accurate and cost-effective method for evaluating thyroid nodules and should be performed on all nonfunctional nodules ≥1 cm in size, unless they are simple cysts with no solid components (refer to Fig. 23.1) [1]. In a patient with multiple nodules ≥1 cm (e.g., multinodular goiter), those nodules with suspicious sonographic findings should be preferentially biopsied with FNA. If none of the nodules have a suspicious appearance, the largest nodules should be evaluated with FNA. FNA of smaller nodules is also indicated in patients with a family history of thyroid cancer, a personal history of radiation exposure, or concerning ultrasound characteristics (see above). Additionally, if a thyroid nodule is detected incidentally on a positron emission tomography (PET) scan and is fluoro-deoxy-glucose (FDG) avid, it should be biopsied as these nodules have up to a 50 % risk of being malignant [9]. Ultrasound guidance is routinely used, but is especially essential in non-palpable nodules or those with >25–50 % cystic component to allow for more accurate targeting. Results from an FNA are reported in six general categories: benign, follicular lesion of undetermined significance, follicular neoplasm, suspicious for malignancy, malignant, and nondiagnostic. Each of these carries with it a certain risk of malignancy, as detailed in Table 23.1 [9]. See also Fig. 23.1 for guidance in management based on FNA results.
Table 23.1
Bethesda system for reporting thyroid cytopathology: implied risk and recommended management
Cytology classification | Risk of malignancy | Usual management |
|---|---|---|
Nondiagnostic | N/A | Repeat FNA with US guidance |
Benign | 0–3 % | Clinical follow-up |
Atypia or follicular lesion of undetermined significance | 5–15 % | Repeat FNA |
Follicular neoplasm | 15–30 % | Thyroid lobectomy |
Suspicious for malignancy | 60–75 % | Total thyroidectomy or lobectomy |
Malignant | 97–100 % | Total thyroidectomy |
Nondiagnostic
Nondiagnostic or unsatisfactory samples are unable to be reliably interpreted due to limited cellularity or absence of follicular cells. This category also encompasses samples that suffer from poor fixation or preservation. Though this is not generally the final FNA diagnosis received, nondiagnostic results accounted for more than 9 % of all FNA results in a large series of patients that eventually went on to surgical removal at the Mayo Clinic [10]. This result in an FNA report should prompt a repeat US-guided FNA.
Benign
Generally, this category includes multinodular goiter, lymphocytic thyroiditis, and hyperplastic nonfunctional thyroid nodules. While benign aspiration cytology does not completely rule out malignancy, these nodules have a very low rate of pathological cancer diagnosis, with a risk of malignancy of 0–3 %. However, because the risk still exists, patients with a benign FNA result must continue active monitoring, with serial clinical and ultrasound examinations for 6–18 months after the first FNA. If the nodule is stable, then the periodic examinations can be extended to every 3–5 years [1]. Any changes in size or suspicious sonographic features should prompt a repeat FNA biopsy [9].
Any nodule ≥4 cm should undergo the same workup as smaller nodules, with serum laboratory tests, ultrasound evaluation, and FNA. However, surgical removal is recommended even if all of these tests indicate that the nodule is benign, for large nodules have a much higher rate of false-negative FNAs than smaller nodules do [11]. This holds true even if the nodule is functioning (or “hot”) on thyroid scintigraphy.
Atypia of Undetermined Significance/Follicular Lesion of Undetermined Significance (AUS/FLUS)
Cytopathology with atypia represents the most subjective category of results, with an associated malignancy risk of 5–15 %. These results include cells that do not represent benign lesions but do not have a degree of atypia sufficient to define them as follicular neoplasms. Recommendations vary as to how to manage patients with these FNA results. Since this category can include some biopsy results that have minimally sufficient cellularity for evaluation, a repeat FNA can be the most appropriate next step in these cases. The National Cancer Institute recommends obtaining an iodine123 scan, especially if the patient’s TSH level is low. If the nodule is “hot,” the nodule can be followed clinically with a repeat FNA in 3–6 months [9]. If the nodule is “cold,” the patient should undergo a thyroid lobectomy for further diagnostic evaluation and treatment [1, 9]. At our institution, the diagnosis of FLUS carries a malignancy rate that exceeds 15 %, and therefore virtually all patients with FLUS undergo surgery. Since FLUS can be a variable diagnosis, we recommend that each institution evaluates its own malignancy rate.
Follicular Neoplasm/Suspicious for Follicular Neoplasm
Biopsies categorized as follicular/Hurthle cell neoplasms include all non-papillary follicular patterned and Hürthle cell lesions and have a malignancy risk of 15–30 %. Since follicular neoplasms can only be truly differentiated from follicular carcinomas by evidence of capsular or vascular invasion on permanent histology, this distinction cannot be made with FNA alone. These patients must undergo a thyroid lobectomy for further diagnosis. We and others have previously demonstrated that the frozen section is not useful and extremely inaccurate in the evaluation of follicular neoplasms. It does not provide any diagnostic information 90 % of the time [12]. An initial thyroid lobectomy should be performed, and, if the surgical pathology indicates a diagnosis of follicular carcinoma, the patient can return for a completion thyroidectomy when clinically stable [1, 9]. If the patient has had a history of head/neck radiation, a family history of thyroid cancer, a bilateral nodular disease, and/or a preference for bilateral surgery, an initial total thyroidectomy can be considered.
Suspicious for Malignancy
Cytopathology in this category carries an intermediate to high risk of malignancy of 60–75 %. It is used to describe results that appear likely to be malignant but are lacking in sufficient evidence to confirm the diagnosis. These include results that are suspicious for papillary carcinoma (many in this group are eventually diagnosed with follicular variant of papillary carcinoma), suspicious for medullary carcinoma (with insufficient specimen available for confirmatory calcitonin immunostains), suspicious for lymphoma, suspicious for metastatic tumor, or suspicious for malignant neoplasm due to total necrosis of cells (e.g., anaplastic carcinoma). In cases where the FNA is suspicious for papillary thyroid cancer, thyroid lobectomy with intraoperative frozen section or total thyroidectomy is our preferred operation [13]. In the remaining suspicious cytologies, the patient may require diagnostic thyroid lobectomy. The appropriate operative approach depends on the histological diagnosis and is addressed in more detail below. Additionally, if a nodule is suspicious for medullary carcinoma, the patient should be evaluated for elevated serum calcitonin and CEA levels. Nodules suspicious for lymphoma may provide definitive diagnostic results if FNA is repeated with the resulting cells evaluated with flow cytometry for T- and B-lymphocyte markers.
Malignant
Nodules with FNA biopsies reported as malignant have a high risk of malignancy at 97–100 %. As described above, most but not all thyroid malignancies can be diagnosed by cytopathology, including papillary thyroid carcinoma, poorly differentiated thyroid carcinoma, anaplastic carcinoma, medullary carcinoma (with calcitonin immunostains and confirmatory serum tests), lymphoma (with the addition of flow cytometry), and metastatic tumors. While many prognostic scoring systems exist, they have predominantly been replaced by the TNM scoring system from the American Joint Committee on Cancer (AJCC) (Table 23.2) [14]. The ATA strongly recommends that any patient fit to undergo an operation receives at least a near-total or total thyroidectomy for a malignant FNA diagnosis in a carcinoma ≥1 cm, in contralateral disease, or if the patient has a personal history of head or neck radiation therapy or a family history of thyroid cancer [1]. Any additionally recommended procedures will be discussed in the detailed explanation of each histological diagnosis below.
Table 23.2
American Joint Committee on Cancer (AJCC) TNM staging for thyroid carcinomas (7th edition)
Primary tumor (T)* | |
|---|---|
All categories may be subdivided: (s) solitary tumor and (m) multifocal tumor (the largest determines the classification) | |
TX | Primary tumor cannot be assessed |
T0 | No evidence of primary tumor |
T1 | Tumor ≤2 cm in greatest diameter limited to the thyroid |
T1a | Tumor ≤1 cm limited to the thyroid |
T1b | Tumor >1 cm ≤2 cm in greatest dimension, limited to the thyroid |
T2 | Tumor >2 cm ≤4 cm in greatest dimension, limited to the thyroid |
T3 | Tumor >4 cm in greatest dimension, limited to the thyroid or any tumor with minimal extrathyroid extension (e.g., extension to sternothyroid muscle or perithyroid soft tissues) |
T4 | Moderately advanced disease |
Tumor of any size extending beyond the thyroid capsule to invade the subcutaneous soft tissues, larynx, trachea, esophagus, or recurrent laryngeal nerve | |
T4b | Very advanced disease |
Tumor invades prevertebral fascia or encases the carotid artery or mediastinal vessels | |
All anaplastic carcinomas are considered T4 tumors | |
T4a | Intrathyroidal anaplastic carcinoma |
T4b | Anaplastic carcinoma with gross extrathyroid extension |
Regional lymph nodes (N) (comprises of central compartment, lateral cervical, and upper mediastinal lymph nodes) | |
|---|---|
NX | Regional lymph nodes cannot be assessed |
N0 | No regional lymph node metastasis |
N1 | Regional lymph node metastasis |
N1a | Metastasis to Level VI (pretracheal, paratracheal and prelaryngeal/Delphian lymph nodes) |
N1b | Metastasis to unilateral, bilateral, or contralateral cervical (Levels I–V) or retropharyngeal or superior mediastinal lymph nodes (Level VII) |
Distant metastasis (M) | |
|---|---|
M0 | No distant metastasis |
M1 | Distant metastasis |
Anatomic stage/prognostic groups | |||
|---|---|---|---|
T | N | M | |
<45 years | |||
Papillary or follicular (differentiated) | |||
Stage I | Any T | Any N | M0 |
Stage II | Any T | Any N | M1 |
≥45 years | |||
Stage I | T1 | N0 | M0 |
Stage II | T2 | N0 | M0 |
Stage III | T3 | N0 | M0 |
T1–T3 | N1a | M0 | |
Stage IVA | T4a | N0 | M0 |
T4a | N1a | M0 | |
T1–T3 | N1b | M0 | |
T4a | N1b | M0 | |
Stage IVB | T4b | Any N | M0 |
Stage IVC | Any T | Any N | M1 |
Medullary carcinoma (all age groups) | |||
Stage I | T1 | N0 | M0 |
Stage II | T2–T3 | N0 | M0 |
Stage III | T1–T3 | N1a | M0 |
Stage IVA | T4a | N0 | M0 |
T4a | N1a | M0 | |
T1–T4a | N1b | M0 | |
Stage IVB | T4b | Any N | M0 |
Stage IVC | Any T | Any N | M1 |
Anaplastic carcinoma (all are considered Stage IV) | |||
Stage IVA | T4a | Any N | M0 |
Stage IVB | T4b | Any N | M0 |
Stage IVC | Any T | Any N | M1 |
Papillary Thyroid Cancer
Initial Evaluation and Treatment
Papillary thyroid carcinoma (PTC) is the most common thyroid cancer, accounting for 84 % of all thyroid cancers reported in the NCI’s surveillance, epidemiology, and end results (SEER) database from 1992 to 2006 [2]. Fortunately, the prognosis is excellent, with an overall 20–25-year cancer-specific mortality rate of 5 % [15]. Interestingly, in the case of differentiated thyroid cancer, the staging system is additionally based on patient’s age, with patients younger than 45 years old being classified only as Stage I or II (Table 23.2). Multiple subtypes of papillary cancer have been described, including the classical form, with areas that have mostly a papillary growth pattern as well as follicles; a follicular variant that has a predominantly follicular pattern; and the tall cell, columnar cell, diffuse sclerosing, and insular variants, which are all more aggressive than the other more common types [15]. The majority of patients are women, with female patients representing 60 % of new cases in the SEER program [2]. Specific risk factors for PTC include exposure to ionizing radiation and hereditary associations such as familial adenomatous polyposis, Cowden syndrome, and Carney complex. The goals of management for PTC include surgical removal of the primary tumor and any extrathyroidal disease including involved lymph nodes, radioablation of any remaining thyroid tissue, suppression of endogenous TSH, and continued long-term surveillance [16]. Since PTC spreads lymphatogenously, the preoperative workup should include a cervical ultrasound to evaluate the patient for lymphadenopathy. The rate of lymph node metastasis present at the time of diagnosis is 20–90 %, so any suspicious lymph nodes should be biopsied with FNA, as positive findings would increase the extent of the operation [17, 18]. If there is no evidence of lymphadenopathy, the initial operation in nodules ≥1 cm that are positive for papillary thyroid carcinoma should be a total thyroidectomy. The appropriate management of cervical lymph nodes in PTC is slightly more controversial. Some experts advocate a prophylactic dissection of the central neck (level VI, including the lower jugular node from the cricoid cartilage to the clavicle), citing the high percentage of nodal metastases at diagnosis and the inability to detect nodal micrometastases preoperatively with standard imaging. However, in the absence of any overt nodal disease, others recommend limiting the operation to a total thyroidectomy because extending the dissection can also increase complications, because prophylactic dissection has not been convincingly proven to reduce mortality or local recurrence and because, regardless of the significance of micrometastases, they can be treated with radioactive iodine ablation. The ATA recommends a central compartment (level VI) neck dissection for any patients with clinically significant FNA-positive central or lateral neck lymph nodes. For patients with no evidence of nodal disease, the recommendations are based only on consensus expert opinion and suggest that a prophylactic central compartment dissection can be performed in patients with more advanced primary tumors (T3 or T4, Table 23.2), but that total thyroidectomy is also a sufficient treatment, especially in T1 or T2 primary carcinomas [1]. We generally do not perform a prophylactic central neck dissection.
Postoperative Management
The second goal of PTC management is radioablation of any remnant tissue or unrecognized/unremoved micrometastases in selected patients. PTC cells are sensitive to iodine-131 (I131), which is generally administered 4–12 weeks postoperatively. It should not be employed in patients who underwent less than a near-total thyroidectomy, as the remaining intact thyroid gland will absorb all or nearly all of the iodine, preventing it from treating the intended targets, micrometastases, and remnant tissue. Based on many previous studies of effective doses to achieve ablation while minimizing excess radiation, the ATA recommends 30–100 mCi doses in low-risk patients and allows for use of higher doses (100–200 mCi) in patients with known or suspected residual disease or with an aggressive variant cell type on tumor histology [1]. While the goal of radioactive iodine (RAI) ablation is specifically to ablate any small amount of remaining normal thyroid tissue, it can also be considered as adjuvant therapy to potentially treat any remaining thyroid cancer cells [19]. A scan approximately 2–10 days after administration of postoperative RAI ablation can also be useful in surveying patients for remaining disease, especially unrecognized disease in the neck that would have been masked by thyroid uptake in preoperative imaging. Two clear recommendations for RAI use exist: low-risk (stage I) patients under 45 years old should not undergo postoperative RAI ablation, and high-risk (stage III-IV) patients older than 45 years old or any with tumors >4 cm should receive postoperative RAI ablation [1, 20]. In the former group, use of RAI therapy does not show any overall or disease-free survival benefit [20, 21], while in the latter group, single-dose RAI adjuvant therapy has been shown to decrease disease recurrence and, in some cases, prolong survival [20, 22, 23]. Use of postoperative radioiodine therapy in all other groups is selective. The ATA recommends that patients older than 45 years with a T1–T2 carcinoma who also have N1 disease or other high risk factors should receive RAI adjuvant therapy. On the other hand, patients with multifocal cancer where none of the foci are >1 cm and no other high risk factors are present should not have RAI therapy [1].
Patients undergoing RAI ablation need to have high serum levels of circulating TSH (>30 mU/L) to stimulate uptake of iodine into cells. This can be achieved by withdrawal of levothyroxine over 4–6 weeks or by TSH stimulation with administration of recombinant human TSH (rhTSH). Baseline postoperative thyroglobulin (Tg) tests should also be performed at this time, when TSH will be at the highest level, around 72 h after administration of rhTSH [16] Thyroglobulin can only be synthesized by thyroid follicular cells, and it is thus used as a postoperative tumor marker for papillary or follicular thyroid cancer recurrence. While preoperative levels have no demonstrative predictive or prognostic utility, and thus should not be routinely measured, post-thyroidectomy levels should be consistently <2 ng/mL. Thyroid hormone suppression and rhTSH stimulation are provocative tests, and any Tg level >2 ng/mL under either of these conditions is indicative of recurrent (or persistent if in the first postoperative evaluation) disease [24].
The third goal for management of patients with PTC is suppression of endogenous TSH levels. TSH has a trophic effect on thyrocytes, and therefore suppressing circulating levels with supraphysiologic doses of levothyroxine has been demonstrated to reduce the risk of major clinical adverse events [25, 26]. The ATA consensus recommendations for degree of suppression are <0.1 mU/L for high- or intermediate-risk patients and 0.1–0.5 mU/L for low-risk patients.
Long-Term Surveillance
Surveillance in PTC consists of serial laboratory tests and imaging studies. The frequency of these tests is dictated in part by the TNM staging of the primary tumor and histological considerations such as resection margins and aggressive histological subtypes. The first evaluation should occur 6 months after RAI ablation. This consists of a physical exam, cervical ultrasound of the central and lateral compartments, and measurement of serum Tg, TSH, and antithyroglobulin (anti-Tg) antibodies. The anti-Tg antibodies should always be measured with Tg in surveillance as high levels of antibodies can falsely lower Tg levels. Rising serial anti-Tg antibody levels can be a surrogate marker for residual normal thyroid tissue or tumor. Tg levels can be measured with or without TSH stimulation, as long as the manner is consistent throughout. In low-risk patients, an undetectable Tg with undetectable anti-Tg antibody during TSH suppression and then confirmed with rhTSH stimulation is one of the criteria for disease-free status. Patients must also have undergone a total or near-total thyroidectomy and thyroid remnant ablation and have no clinical or imaging evidence of tumor on whole-body scans at follow-up examination.
Cervical ultrasounds evaluating the central and lateral compartment should be performed at 6 and 12 months post-RAI ablation and then annually for at least 3–5 years. If nodes are suspicious for disease involvement and are 5–8 mm in the smallest diameter, they should be biopsied by FNA with Tg measurement in the needle washout fluid. Lymph nodes suspicious for involvement smaller than 5–8 mm in largest diameter can be monitored without biopsy, but should be followed for growth and biopsied if changes occur.
Whole-body RAI scans (WBS) are used in surveillance of intermediate- or high-risk patients to detect any persistent or recurrence of iodine-avid disease. Any patient who had minimal to no uptake on the first WBS after RAI ablation treatment will have low sensitivity on any subsequent scans, so low-risk patients with undetectable Tg levels and negative cervical ultrasounds should not undergo a WBS as part of surveillance [1]. Intermediate- or high-risk patients should have a WBS with levothyroxine withdrawal or rhTSH stimulation 6–12 months after RAI ablation. However, since this test is for detection and not ablation, it should be done with lower radiation exposure levels, either by using 123I or low-activity 131I.
Management of Recurrent Disease
Recurrences in PTC are either locoregional or distant metastases. Locoregional disease detected by one of the above surveillance methods should be confirmed with FNA. The treatment of choice for locoregional recurrences is surgical resection. In general, the recommended approach to resection is either by formal compartmental resection of the involved side of the neck (level VI) or selective ipsilateral dissection of previously unexplored compartments with clinically significant involved nodes (>8 mm in diameter) (levels II–IV). With extensive disease, a modified neck dissection may be appropriate (levels II–V), with sparing of the spinal accessory nerve, internal jugular vein, and sternocleidomastoid muscle. These approaches are all preferred compared to selectively removing only nodes that appear positive, as micrometastases are generally more extensive than can be appreciated from imaging studies [1]. However, if the recurrent disease is in a previously dissected compartment, it may be appropriate to selectively remove only the involved nodes, as complete resection of the compartment may jeopardize surrounding vital structures [15].
Distant metastases most commonly occur in the lungs, bones, and central nervous system (CNS). Any iodine-avid disease should be treated with RAI ablation and therapy, with treatments completed every 6–12 months as long as the disease continues to take up the RAI. Macronodular disease in any location can be considered for surgical removal, especially for tumors that are not iodine avid. 18FDG-PET scans should be considered if Tg levels are high (≥10 ng/mL), but a WBS does not show any uptake. This usually indicates that there is a present focus of recurrent disease that is not iodine avid but may be detectable with 18FDG-PET. External beam radiation therapy (EBRT) or stereotactic radiosurgery may be considered for bone or CNS metastases, respectively, in the absence of iodine avidity when surgical resection would be unacceptably morbid [16]. This should be done in conjunction with corticosteroid administration to limit the risk of complications from acute tumor expansion.
Unfortunately, PTC is relatively insensitive to standard forms of cytotoxic chemotherapy, and it is thus not a recommended treatment option. In patients with recurrent disease that is resistant to all other forms of treatment, doxorubicin monotherapy is the only chemotherapy treatment that has been approved by the US Food and Drug Administration [1]. While this can show some cytotoxic tumor effect, it may also sensitize recurrent disease to EBRT, thus improving the efficacy of radiation treatment.
Follicular Thyroid Cancer
Initial Evaluation and Treatment
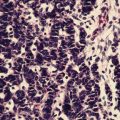
Follicular thyroid carcinoma (FTC) is the second most common type of thyroid cancer, accounting for 10 % of all new cases in the SEER program from 1992 to 2006 [2]. Hürthle cell carcinoma (HCC), while classified by the World Health Organization as a subtype of FTC, is actually a distinct clinical entity. It accounts for 4 % of all thyroid cancer cases, and, while it shares some similarities with FTC, they have different risk factors and considerations for treatment. The risk factors for developing FTC are similar to those for PTC, including radiation exposure and similar hereditary syndromes such as Cowden syndrome and Carney complex type 1. HCC has no associated genetic syndromes, but a connection between HCC and lymphoma has been proposed, though this requires more research to confirm. The imaging workup for FTC and HCC is as described above for PTC, though the common findings differ from those in PTC. On ultrasonography, follicular cancers tend to be iso- or hyperechoic (compared to the hypoechoic PTCs) and have a thick, irregular halo but lack microcalcifications [27].
FTC presents a diagnostic dilemma by FNA due to the inability to distinguish follicular adenomas from carcinomas by cytology alone because the distinction is based on invasion not apparent in an FNA. Additionally, efforts should be made to distinguish Hürthle cell neoplasms (HCN) from follicular neoplasms (FN). HCC has a higher risk of locally invasive (T4) disease at diagnosis (27 % vs. 9 %) and higher rate of recurrence (24 % vs. 8 %) than FTC [28]. HCC is also not generally iodine avid, so it cannot generally be treated by RAI ablation. Based on this information, patients with a diagnosis of FN/HCN on FNA should undergo a thyroid lobectomy and isthmusectomy at minimum, though high-risk patients, HCN patients with a nodule >4 cm or ≥70 years old, or patients with bilateral thyroid nodule(s) ≥1 cm should be considered for a total thyroidectomy as the initial operation [29–32]. Since follicular cancers spread hematogenously, the rate of synchronous lymph node metastases is very low (<10 %), though this risk may be slightly higher in HCC; routine prophylactic lymph node dissection is not recommended [1, 30]. If suspicious lymph nodes are detected in preoperative ultrasonography, these nodes should be biopsied with FNA to confirm involvement and removed during the initial operation, along with any nodes that appear grossly involved at the time of operation.
By pathology from the initial lobectomy, FTCs can be classified as minimally invasive or invasive variants. Minimally invasive FTC is encapsulated with a single focus of capsular invasion (differentiating it from a FN). Invasive FTC has sites of angioinvasion or extensive invasion beyond the capsule along with diffuse infiltration of the affected thyroid lobe [29]. Thyroid lobectomy is thus sufficient to treat a minimally invasive FTC, while a total thyroidectomy is necessary to treat invasive FTC. The management differs slightly in regard to lymph node dissection with a diagnosis of HCC from the initial lobectomy. Since HCC has higher rates of lymph node involvement and is often radioresistant, the ATA recommends considering central neck dissection (level VI) at the time of completion thyroidectomy.
Postoperative Management
Postoperative management follows the same principles for FTC and HCC as for PTC. Patients with minimally invasive FTC treated with a thyroid lobectomy need only have long-term surveillance, as described below. Patients treated with a total or completion thyroidectomy should undergo an evaluation for residual disease along with RAI ablation with 131I, which should be done approximately 4–12 weeks postoperatively under conditions of either levothyroxine withdrawal or rhTSH stimulation, as described earlier. A WBS done 2–10 days after RAI administration can identify areas of residual iodine-avid thyroid tissue. Baseline postoperative Tg and anti-Tg antibody should be drawn at this time also, to obtain it under levothyroxine withdrawal or rhTSH stimulation. Although the majority of HCCs will not be iodine avid, this should not preclude undergoing a RAI ablation. Even if this does not treat any residual microcarcinomatous disease, it will ablate any remaining thyroid tissue, making Tg surveillance testing and future WBS more sensitive. Additionally, both FTC and HCC have TSH receptors, and so chronic TSH suppression should be initiated postoperatively in both, following the same process and to the same suppression levels as described for PTC.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree