Clinical scenario
Recommendations
Level of evidenceb
Primary thromboprophylaxis
Not recommended (including LMWH, warfarin, FFP)
1B
Routine screening with coagulation studies or for thrombophilia not recommended
2C
Thrombophilia screening can be considered for patients with known TE risk factors
2C
Development of a non-CVC-related thrombosis
Thrombophilia screening
2C
Thromboembolism
Treatment with LMWH
2B
Thrombolysis with tPA or thrombectomy for life- or limb-threatening thrombosis
2C
Warfarin generally not recommended but can be considered with long-term anticoagulation
2B
Treatment for a minimum of 3 months and until the precipitating factor has resolved
2C
Consideration for holding asparaginase therapy during acute TE
2C
If nonfunctioning or no longer needed, the CVC should be removed after 3–5 days of anticoagulation
1B
If functioning and clinically necessary, the CVC can remain with continuing anticoagulation
2C
Cerebral sinovenous thrombosis
Total anticoagulation for at least 3 months
1B
Continued anticoagulation for 3 additional months if with persistent occlusion or symptoms
2C
If with hemorrhage, anticoagulation can be reserved for cases with thrombus extension
2C
Prophylactic anticoagulation should be given with subsequent asparaginase doses
2C
Thrombocytopenia with anticoagulation
Initially transfuse to keep platelets >20–50 × 109/L
2C
Subsequently, hold anticoagulation for platelets <20–50 × 109/L
2C
Lumbar puncture with concomitant anticoagulation
LMWH should be held 24 h prior and resumed 12 h after LP
1C
8.2 Acute Lymphoblastic Leukemia (ALL)
The incidence of thromboembolism in children with ALL is estimated to be between 1.1 and 36.7 % (Athale and Chan 2003a). This wide variation is likely due to differences in the definition of TE (symptomatic versus occult), diagnostic methods, study design, reporting period and treatment regimens. The true incidence is likely underestimated because patients are generally not screened for asymptomatic TE. The Prophylactic Antithrombin Replacement in Kids with ALL treated with Asparaginase (PARKAA) study reported a TE incidence of 36.7 % with prospective screening radiography after induction therapy; only 5 % were clinically symptomatic (Mitchell et al. 2003b). A meta-analysis estimated the rate of symptomatic thrombosis in 1,752 children with ALL from 17 prospective studies to be 5.2 % (Caruso et al. 2006). The risk is highest during induction, with an incidence rate more than double that in later phases of therapy. Although rare, thrombosis can also occur prior to the start of ALL treatment (Payne and Vora 2007).
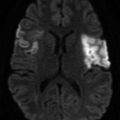
The CNS is by far the most common location of thrombosis in ALL, accounting for 54 % of events in the meta-analysis by Caruso et al. (2006). Twenty-nine percent of these were cerebral sinovenous thromboses (CSVT), while other types of CNS events were less clearly defined (Caruso et al. 2006). In their review, Athale and Chan (2003a) reported that 52 % of CNS events were CSVT, with 43.7 % parenchymal lesions and 4.3 % combined. The etiology of CNS thrombosis in children with cancer is likely multifactorial and related to direct tumor invasion, chemotherapy-induced hypercoagulability, and associated complications like dehydration and infection (Wiernikowski and Athale 2006). Non-CNS events in the meta-analysis by Caruso et al. (2006) included deep vein thrombosis (DVT, 43 %), pulmonary emboli (PE, 2 %) and right atrial thromboses (2 %). DVT was noted to be more common in upper than lower extremities, most in association with a CVC (Caruso et al. 2006). The majority of thromboses are venous, with only 3 % of events reported as arterial in the review by Athale and Chan (2003a). In 5 % of cases, thromboses were multifocal and 50 % of TE occurred in potentially life-threatening locations (Caruso et al. 2006). Thrombosis accounts for a relatively small fraction of treatment-related mortality, with reports ranging from 0 to 4.8 %, largely from PE and CNS events (Athale and Chan 2003a). Very little evidence exists about morbidity from TE in pediatric ALL; one study of pediatric ALL survivors reported a 50 % prevalence of post-thrombotic syndrome (PTS) following a symptomatic TE (Kuhle et al. 2008). PTS includes symptoms of pain, swelling and skin changes to the affected limb. For patients with CNS TE, reports suggest that up to 15–20 % will have residual neurologic deficits, while the effect on neurocognitive outcome is unknown (Athale and Chan 2003a). Others report that full neurologic recovery is the norm (Payne and Vora 2007). Qureshi et al. (2010) reported no permanent sequelae of TE among 59 children with ALL, including those with CSVT who presented with neurologic deficits.
8.3 ALL Risk Factors
Several studies have identified older age as a significant risk factor for TE among children treated for ALL (Athale and Chan 2003a). An analysis of 91 patients treated at McMaster Children’s Hospital following Dana Farber Cancer Institute (DFCI) protocols for ALL found that 7 of 16 patients ≥10 years (44 %) developed symptomatic TE versus 3 of 75 (4 %) in younger patients (Athale et al. 2005). Patients classified with high-risk ALL also appear more likely to develop TE, though this is confounded by the effect of age, as older children are considered high-risk by definition. In the same McMaster study, 26 % of the 35 high-risk patients developed TE (11 % of those <10 years) versus 2 % of 56 standard-risk patients. The effect of gender on the risk of TE has been less clear, with contradictory reports published; in the McMaster study, gender did not influence risk of TE (Athale and Chan 2003a; Athale et al. 2005). The presence of a CVC is a well-established risk factor for TE in the general pediatric population as well as in ALL; half of all symptomatic DVT in children with ALL are associated with a CVC (Athale and Chan 2003a).
Multiple studies have reported the association of genetic prothrombotic defects and ALL, including factor V Leiden, prothrombin gene G20210A mutation, MTHFR C677T and A1298 mutations, deficiencies of protein C, protein S, or antithrombin (AT), and high lipoprotein (a) levels. In the largest study, Nowak-Göttl et al. (1999) prospectively evaluated inherited thrombophilia traits in 301 children enrolled on ALL Berlin-Frankfurt-Muenster (BFM) 90/95 protocols. Eleven percent of patients with complete follow-up experienced a symptomatic TE, and the presence of an inherited thrombophilia significantly increased the risk: 46.5 % with an identified prothrombotic defect experienced a TE versus 2.2 % without such a defect. The greatest risk was associated with protein C, protein S and AT deficiency (Nowak-Göttl et al. 1999). In contrast, the North American PARKAA study prospectively evaluated the prothrombin 20210A mutation and factor V Leiden in 60 children with ALL and correlated with screening radiography but found no association with TE (occult or symptomatic), though four of eight patients with antiphospholipid antibodies did experience thrombosis (Mitchell et al. 2003b). Caruso et al. (2006) reviewed five prospective studies reporting prothrombotic genetic defects; the prevalence of mutations was similar to the general population and the pooled relative risk of TE with thrombophilia was 8.5. It remains unclear as to why studies of risk in children with thrombophilia have shown such variable conclusions (Raffini and Thornburg 2009).
Much of the literature regarding thrombosis in ALL patients centers on the use of L-asparaginase. Asparaginase catalyzes the hydrolysis of the amino acid asparagine to aspartic acid and ammonia. The rapid depletion of the circulating pool of asparagine reduces hepatic protein synthesis, which in turn causes a decrease in natural anticoagulants such as AT, fibrinogen, and plasminogen, as well as protein C and S. The coagulopathy associated with asparaginase may result in both thrombosis and hemorrhage, although the former is much more common (Athale and Chan 2003b). The pharmacology of asparaginase is affected by its source (Escherichia coli or Erwinia chrysanthemi), different commercial manufacturers (European, Japanese, American), and modifications (polyethylene glycosylated; PEG-asparaginase), with profound effects on half-life, asparagine depletion and protein synthesis inhibition. Comparison of published rates of TE associated with asparaginase is hampered by this variability as well as by variations in dosage, timing of administration, and concomitant chemotherapy. In the meta-analysis by Caruso et al. (2006), the rate of TE was significantly decreased with doses of ≥10,000 units/m2 vs. ≤6,000 units/m2 and with <9 days of asparaginase exposure; type of asparaginase or manufacturer did not show significant differences.
PEG-asparaginase, formed by covalently attaching polyethylene glycol to the native E. coli asparaginase enzyme, is now more commonly used in ALL therapy protocols and was associated with a 2 % risk of thrombosis in a study of 197 patients treated from 2005 to 2007 following a DFCI protocol including prednisone during induction (Silverman et al. 2010). Qureshi et al. (2010) reported venous thrombosis in 3.2 % of 1,824 patients treated on the British UK ALL 2003 protocol using PEG-asparaginase and dexamethasone during induction and delayed intensification. Ninety percent of events occurred during PEG-asparaginase exposure, 70 % of which were during induction. Although CVC placement was deferred to the end of induction on this protocol to reduce the risk of CVC-associated TE, 50 % of events were CVC related, while 36 % involved the CNS and the remainder were DVTs (Qureshi et al. 2010). All patients recovered completely without clinical sequelae, and 73 % received subsequent asparaginase (the majority with prophylactic LMWH) with no recurrent TE or excess bleeding. Intravenous PEG-asparaginase has been reported to have a similar rate of thrombotic complications as intramuscular administration (Silverman et al. 2010).
The effect of asparaginase may be further augmented by the concurrent use of corticosteroids during ALL induction, which can also increase the VTE risk eight to tenfold (Nowak-Göttl et al. 2009; Mitchell et al. 2010). In a prospective cohort study of 420 ALL patients enrolled on separate German cooperative protocols, symptomatic TE occurred in 11.6 % of those treated with concurrent prednisone and E. coli asparaginase in induction versus 2.5 % among those who received asparaginase in consolidation without prednisone (Nowak-Göttl et al. 2001). Steroids increase the level of prothrombin as well as factor VIII, von Willebrand factor, PAI-1 and AT (Harlev et al. 2010). Some evidence exists for a lower risk of TE with prednisone versus dexamethasone; 10.4 % of children receiving dexamethasone during induction on the BFM 2000 protocol developed TE compared with 1.8 % of those who received prednisone on the earlier BFM 90/95 protocols despite similar asparaginase dose and schedule (Nowak-Göttl et al. 2003). Caruso et al. (2006), however, showed no difference in rate of TE between prednisone and dexamethasone in induction although prednisone led to a significant increased risk in postinduction phases. Further data are required to make firm conclusions regarding the effect of steroids on thrombosis risk in pediatric ALL patients.
8.4 Other Malignancies
Data regarding TE in pediatric malignancies other than ALL are limited. Overall, more than 40 % of pediatric oncology patients with TE have a diagnosis other than ALL, and the prevalence among non-ALL cancers is about 16 % (Wiernikowski and Athale 2006). Lymphoma and sarcoma have an increased risk of TE, while brain tumors do not (Athale et al. 2008b). As in children with ALL, children with other malignancies are at significantly increased risk of TE if older and if with CVC dysfunction; mediastinal disease is a significant risk factor in children with lymphoma with a trend toward increased risk in patients with more extensive disease (Athale et al. 2007; Athale et al. 2008a).
A 2008 retrospective study of 75 children diagnosed between 1999 and 2004 with Hodgkin lymphoma (HL) or non-Hodgkin lymphoma (NHL) reported 9 patients (12 %) with 16 thrombotic events (Athale et al. 2008a). Twelve of these events were venous and there was a 2.6 % rate of PE (Athale et al. 2008a). Sixty-nine percent were associated with a CVC and none were CNS events, in contrast with the distribution in ALL patients. However, it has been reported separately that 1–3 % of patients with advanced NHL develop CSVT (Wiernikowski and Athale 2006). In multivariate analysis, mediastinal involvement increased the risk of thrombosis; 9 of 51 patients with mediastinal lymphadenopathy developed TE versus none of 21 patients without mediastinal involvement (Athale et al. 2008a). Lymphoma type, gender, presence of B-symptoms, age and stage were not risk factors for TE in lymphoma patients. Notably, despite the use of asparaginase, children with NHL did not appear to be at higher risk for TE than children with HL, contrasting results in adults (Wiernikowski and Athale 2006; Athale et al. 2008a). The meta-analysis additionally noted a 40 % recurrence rate (four patients); of these patients, only two had received secondary thromboprophylaxis with coumadin or LMWH and both had TE recurrence while on coumadin.
A retrospective cohort study investigated thromboses in 122 children and adolescents with soft tissue sarcoma treated at the National Cancer Institute from 1980 to 2002 (Paz-Priel et al. 2007). The authors reported 23 thromboembolic events in 19 patients and an overall TE incidence of 16 %. Over 50 % of the TE were detected at the time of initial cancer evaluation and 57 % were symptomatic. Thirty-five percent of thromboses were related to tumor compression and 13 % CVC associated. Involved sites included extremity DVT (43 %), PE (22 %) and inferior vena cava (17 %). Patients with distant metastasis were 2.5 times more likely to have a clot, 23 % vs. 10 %, with a trend towards significance (Paz-Priel et al. 2007). The rate of TE was similar for all types of sarcoma and between children and young adults. Though thrombophilia was infrequently investigated, four patients had lupus anticoagulant detected. In another single-institution retrospective analysis of pediatric sarcoma patients treated between 1990 and 2005, 10 of 70 patients (14.3 %) developed symptomatic TE (all DVTs), six of which were CVC associated (Athale et al. 2007). CVC dysfunction significantly increased the risk of TE: 55 % of those with CVC problems developed TE versus 8.2 % in those without. Prevalence of TE was increased in patients with pulmonary disease, metastases, older age and Ewing sarcoma, but these factors failed to reach statistical significance. Relapse and death were more common in patients with symptomatic TE but again without reaching statistical significance.
In adults with malignant brain tumors, the risk of TE is 20 % in the perioperative period without prophylaxis and risk remains high throughout treatment, reaching 28 %, particularly in adult patients with malignant gliomas (Wiernikowski and Athale 2006). TE is comparatively much less common in children with CNS tumors (Athale et al. 2008b). Tabori et al. (2004) reviewed 462 pediatric patients with malignant brain tumors over 14 years in Israel and only three (0.6 %) had symptomatic VTE. All were severely debilitated at the time of TE diagnosis, likely stemming from complications of their underlying malignancy (Tabori et al. 2004). In a report of 253 patients treated at St. Jude Children’s Research Hospital, the frequency of symptomatic TE was 2.8 %, with increased risk associated with CVC dysfunction (Deitcher et al. 2004). Athale et al. (2008b) reported a significantly lower prevalence of TE in patients with CNS tumors than other groups, with one event among 201 children with CNS tumors. A summary of known and presumed risk factors for TE is presented in Table 8.2.
Table 8.2
Summary of known and presumed risk factors for thromboembolism in pediatric oncology patientsa
Known risk factorsb | Type of malignancy |
ALL | |
AML | |
Lymphoma | |
Sarcoma | |
Older age | |
Presence of central venous cathether | |
Dysfunction of central venous catheter | |
Asparaginase therapy in ALL | |
Steroid therapy in ALL | |
Blood vessel compression by bulky solid tumor | |
Presumed risk factorsc | Type of malignancy
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|