Thermal Stress
Robert W. Kenefick
Samuel N. Cheuvront
John W. Castellani
Catherine O’Brien
INTRODUCTION
In the past, aviators in open cockpit aircraft had to perform flight tasks with little or no protection from the environment or protective systems to mitigate environmental stresses. With the advent of modern aircraft, protective clothing, and survival equipment, it would seem that thermal stress (heat or cold) would no longer be a significant concern for the modern aviator. However, present day protective systems and equipment used in aviation create new situations where aviators remain challenged by thermal stress. For example, closed cockpits can create heat stress due to the greenhouse effect from solar radiation. Protective clothing [G-suits, nuclear-biological-chemical (NBC) gear] add to the difficulty of performing a task and increase heat stress and the risk of dehydration. The proximity of flight crews or ground crews to heat generated by engines and/or reflected from the tarmac or flight deck is also of great concern. This heat stress is further exacerbated by the ambient environment itself when working (ground crews) or waiting outdoors (flight crews) during preflight, taxiing, or standby for takeoff. The combined effects of heat stress and dehydration over many hours for both ground and flight crews can alter cognitive function, delay reaction time, increase error rate, deteriorate physical stamina, impair cockpit management, and increase the risk of heat illness or injury. Although heat mitigation systems exist (air-conditioning, built-in clothing cooling systems), their cooling capacity is limited.
Ground crews and support personnel may also be exposed to cold climates. As with heat, exposure to cold for longer periods can degrade cognitive function such as decision making and physical performance, including manual dexterity, and can increase risk of injury. This is especially true for ground crews who are not only exposed to cold air but also use their hands to perform tasks, where heat loss can occur when touching metal tools, and may lose heat through their feet by standing on a cold tarmac or flight deck for long periods. In these scenarios, risk for frostbite and freezing injuries can be of concern, especially in the extremities (fingers, toes). Heat loss and the risk of cold injury are further aggravated by environmental factors such as wind and/or rain that increase the rate of body heat loss. Flight crews must also be concerned with cold environments during in-flight operations on aircraft with high airflows such as helicopters operating with open doors (Figure 7-1).
 FIGURE 7-1 Aerospace personnel may be exposed to low ambient temperatures both during flight and upon planned or unplanned landings in cold climates. |
The protection from the environment (cold or heat) afforded by the aircraft is lost when pilots are forced to land or ditch. Once on the ground or in the water, flight crews are fully exposed and a large part of survival depends on meeting environmental challenges. Understanding the factors that contribute to heat gain or heat loss, dehydration, and injury due to environmental exposure can be important not only for ground and flight crews but also for aeromedical personnel who must not only recognize signs of heat or cold injury and dehydration but must also be able to provide appropriate medical treatment. This chapter will outline the specifics regarding mechanisms of heat exchange, the physiological and cognitive responses to environmental stress and dehydration, guidance for operations in hot and cold environments, and will present the signs and symptoms of injuries and illnesses related to heat and cold exposure and provide treatment recommendations.
Biophysics of Heat Exchange
Changes in body core temperature are the result of either a positive or negative change in heat storage. If the body gains more heat than it dissipates, body core temperature will rise. Conversely, if heat loss exceeds heat gain, then heat storage will be negative and core temperature will fall. We can present these relationships between gain and loss mathematically as follows:
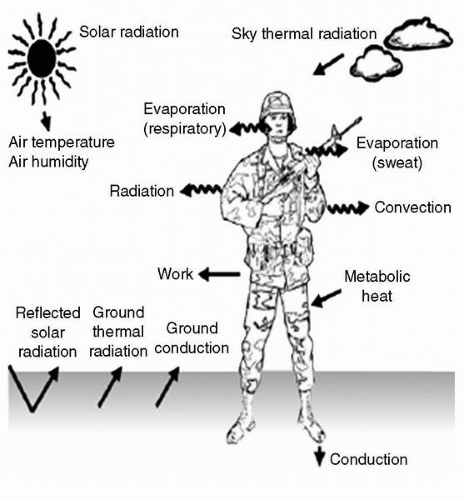
S = M − (± Work) − E ± (R + C) ± K
where S = heat storage, M = metabolic heat production, E = evaporation, R = radiation, C = convection, K = conduction, and W = external work (1). E, R, C, and K are the heat exchange pathways, explained in detail in the subsequent text. The mathematical equation contains positive and negative signs that indicate heat gain (positive sign) and heat loss (negative sign). It is important to understand that heat gain or loss by some of these exchange pathways are mathematical. Situations such as negative work (−W) may not occur in “real world” applications. Examples of heat gain and storage while on the ground and in the cockpit are depicted in Figures 7-2 and 7-3.
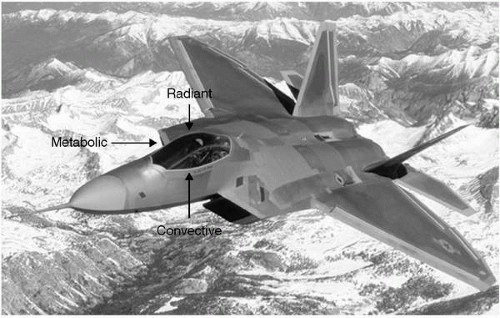 FIGURE 7-3 Examples of cockpit heat sources. Radiative heat from sun and electrical equipment; convective heat from air within cockpit and greenhouse effect; metabolic heat from pilot(s). |
During physical work, approximately 25% of energy expended goes toward performing the actual work and approximately 75% of energy expended is released in the form of heat. This heat is released from active skeletal muscles and transferred from the body core to skin, which then must dissipate the heat to the environment. Physical exercise can increase whole body metabolism by as much as 15 to 20 times above the resting metabolic rate in healthy young males. If heat production is not balanced by loss, body temperature will increase early in the work bout. In the cold climate, the opposite scenario occurs, where resting individuals must increase overall resting metabolic
heat production (M) through mechanisms such as shivering, which can increase M by 3 to 5 times, in order to maintain normal body core temperature (37°C).
heat production (M) through mechanisms such as shivering, which can increase M by 3 to 5 times, in order to maintain normal body core temperature (37°C).
Convection is heat transfer by movement of air or fluid over the body, whether induced by thermal currents, body motion, or natural movement of air (wind) or water. Heat loss by convection occurs when the temperature of the air or water that is in contact with skin is below body temperature; conversely, heat gain by convection from air or water occurs when these temperatures approach or exceed that of the body. The primary means of moving heat from the core to the skin is by convection through blood flow (1).
Heat gain by radiation (solar, sky, large objects, and ground) occurs when radiative temperatures are higher than the body surface temperature. Heat loss occurs when surrounding objects or environments have temperatures lower than the body and the body will radiate heat to these objects and environments. Accordingly, temperature combinations of the sky, ground, and surrounding objects may exist which results in body heat gain due to radiation, although the air temperature is below that of the body. Radiative heat exchange is independent of air motion (1).
Conduction is heat transfer to or from solid objects through direct contact. In hot environments, conduction is usually minimal because little contact surface is involved. However, in the case of individuals such as aircrew, conduction can be more significant due to such factors as standing on hot tarmac, or contact with metal aircraft. Conversely, in the cold standing on cold tarmac, or a steel flight deck can result in conductive heat loss and contributes to extremity cooling.
When the ambient temperature is greater than or equal to skin temperature, evaporative heat loss accounts for all body cooling. Eccrine sweat glands secrete fluid onto the skin surface permitting evaporative cooling when liquid is converted to water vapor. Sweat glands respond to thermal stress primarily through sympathetic cholinergic stimulation, with catecholamines having a smaller role in the sweat response (2). The rate of sweat evaporation depends on air movement and the water vapor pressure gradient between the skin and the environment, so in still or moist air the sweat does not evaporate readily and collects on the skin. Sweat that drips from the body or clothing provides no cooling benefit.
The mechanism of heat loss depends on the ambient temperature. At low ambient temperatures (5°C—10°C), dry heat loss (i.e., heat loss from radiation and convection) is greater than heat loss through evaporation. At high ambient temperatures, evaporative heat loss predominates. Ambient water vapor pressure (relative humidity) also affects heat loss. When water vapor pressure is high, less sweat is able to evaporate from the skin to the environment, compared to a dry environment. Heat exchange between skin (or man) and the environment is influenced by air temperature; air humidity; wind speed; solar, sky, and ground radiation; and clothing.
Physiological Regulation in Hot Environments
Humans regulate their body core temperature within a narrow range (35°C-41°C). This is accomplished through behavioral and physiological regulation. Behavioral thermoregulation includes conscious actions such as altering physical activity, selecting appropriate clothing, adjusting indoor thermostats, and seeking shade, sun, or shelter. Physiological temperature regulation is typically independent of conscious behavior, but can be modified by it, and includes control of skin blood flow (Figure 7-4), sweating, and metabolic heat production (2).
Figure 7-4 schematically depicts the sensory and effector aspects of the human thermoregulatory system. Core temperature is the controlled variable under most conditions and must be maintained within defined limits. Signals regarding core temperature are integrated with skin temperature signals at the hypothalamus. If the core temperature signal deviates from the defined set point, appropriate effector responses (e.g., vasoconstriction or dilation, sweating or shivering) are elicited to either reduce or increase peripheral heat loss and metabolic heat production. For example, during exercise in the heat, core temperature is increased. This change in core
temperature causes heat loss effector responses (sweating, vasodilation, and increased skin blood flow) to attenuate the rise in core temperature. These responses exhibit two control characteristics: (i) they turn on when reaching a particular core temperature threshold, and (ii) they exhibit a graded response as the controlled variable is further disturbed. This type of control system is called a proportional control system.
temperature causes heat loss effector responses (sweating, vasodilation, and increased skin blood flow) to attenuate the rise in core temperature. These responses exhibit two control characteristics: (i) they turn on when reaching a particular core temperature threshold, and (ii) they exhibit a graded response as the controlled variable is further disturbed. This type of control system is called a proportional control system.
Figure 7-5 demonstrates the proportional control system for two heat-dissipating responses (sweating and skin blood flow). Note that there is a particular threshold when these physiological responses increase and then as the core temperature continues to rise, these responses increase linearly. Changes in the threshold of an effector response are generally thought of as a change in the set-point temperature (2). Any change in the slope of the relationship between core temperature and the effector response is considered as a change in the sensitivity of the system at a peripheral level (e.g., sweat gland). For example, dehydration will increase the body core temperature threshold for sweating, thereby delaying the onset of sweating.
TABLE 7-1 | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||
Proportional control systems are modified by both thermal and nonthermal factors (3). Skin temperature, a thermal factor, changes the sensitivity of the relationship between sweating and core temperature. Therefore, at any given core temperature, sweat rates are greater when the skin is warm and lower when the skin is cool. Nonthermal factors that change the relationship between core temperature and heat loss responses include dehydration, acclimatization, circadian rhythms, and endocrine status (3,4). Table 7-1 presents the effects of these factors on thermoregulatory control of the heat.
Heat acclimatization is a classic example of how changes in thermoregulatory control impact overall health and performance. Sweating begins at a lower core temperature threshold, allowing earlier heat dissipation and a cooler skin temperature. Similarly, skin blood flow is higher at any given core temperature due to change in the threshold temperature at which cutaneous vasodilation begins to rise (5). Therefore, lower skin temperatures following heat acclimation reduce the volume of skin blood flow for heat exchange; however, acclimation initiates skin blood flow sooner so that dry heat loss (R + C) improves to an even greater extent. Higher sweating rates and skin blood flow, in concert, help explain why core temperature is lower after acclimatization; it is due to better evaporative, radiative, and convective heat loss.
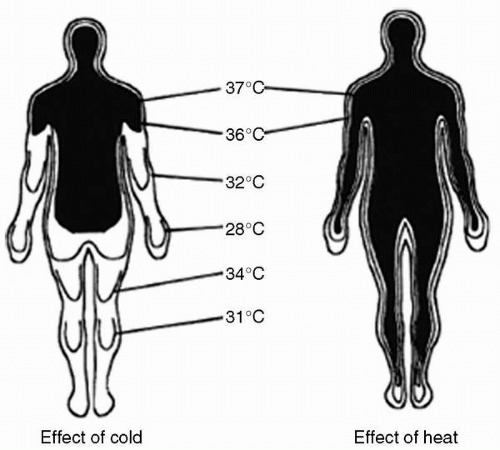
Physiological Regulation in Cold Environments
One of the initial responses to cold exposure is peripheral vasoconstriction. Decreased blood flow to the shell (skin, subcutaneous fat, and skeletal muscle) in effect increases insulation, and reduces convective heat transfer between the body’s core and shell (Figure 7-6), and skin temperature declines. Skin vasoconstriction begins when skin temperature falls below 33°C(95°F). As exposure to cold continues, vessels in underlying tissues vasoconstrict and thereby increase the insulating layer. Cooling of underlying inactive muscles can cause them to become stiff. Therefore, the vasoconstrictor
response to cold exposure helps retard heat loss and defend core temperature, but at the expense of a decline in peripheral tissue temperatures (6).
response to cold exposure helps retard heat loss and defend core temperature, but at the expense of a decline in peripheral tissue temperatures (6).
Another primary response to cold exposure is involuntary shivering, which increases metabolic heat production and voluntary behavior, that is, increasing physical activity (exercise, increased “fidgeting,” etc.) which increases heat production. Shivering consists of involuntary, repeated, rhythmic muscle contractions (7), and may start immediately, or after several minutes of cold exposure, usually beginning in torso muscles and then spreading to the limbs (8). The intensity and extent of shivering varies according to the severity of cold stress. As shivering intensity increases and more muscles are involved metabolic rate increases, typically reaching approximately 600 to 700 mL/min during resting cold air exposure, and often exceeding 1,000 mL/min during resting cold water immersion (6). The highest oxygen intake reported is 2.2 L/min, recorded during cold water immersion, which was approximately six times the resting metabolic rate (50% VO2max) for that subject (9).
A common response to cold exposure is cold-induced diuresis (CID), an increase in urine production associated with the central fluid shift induced by vasoconstriction (10). The fluid loss due to CID does not have the same effects on health and performance during cold exposure as a similar loss of fluid would during heat exposure. In fact, individuals who are dehydrated before cold exposure typically experience less CID than euhydrated individuals (11), that is, the diuresis is self-limiting. Furthermore, individuals who have free access to food and fluid will rehydrate upon returning to a warm environment. The fluid loss due to CID may be more important during heavy exercise in the cold environment when core temperature is elevated and blood flow to the skin increases to dissipate heat. If individuals in the cold environment are heavily clothed, they may overheat more readily and increase fluid losses due to thermoregulatory sweating. For these reasons, maintaining hydration is important during work in cold environments. Dehydration does not appear to increase risk of peripheral cold injury (11).
The vasoconstriction-induced reduction in blood flow and fall in skin temperature contribute to the etiology of peripheral cold injuries, particularly in the digits, ears, cheek, and nose. Cold-induced vasoconstriction has pronounced effects on the hands, fingers, and feet making them particularly susceptible to cold injury, pain, and a loss of manual dexterity (12) (Figure 7-6). Another vasomotor response, cold-induced vasodilatation (CIVD), can under some circumstances interrupt vasoconstriction in the fingers, toes, nose, cheeks and ears. Following the initial decline in skin temperature during cold exposure, an increase in blood flow may occur. The CIVD may be transient, resulting in periodic oscillations of skin temperature. The increased blood flow increases local tissue temperature and may protect against cold injury. Although initiated by local cooling, the CIVD response is also modulated by the central nervous system (13).
Wet Bulb Globe Temperature
Numerous environmental indices have been proposed for predicting thermal heat strain. The most widely used of these is the Wet Bulb Globe Temperature (WBGT) index, which was developed 50 years ago to provide guidance for controlling heat casualties among military troops in hot environments (14). Since this time, the index has also been adopted and popularized by occupational and sports governing authorities to promote safe environmental limits for work and exercise. The WBGT index is computed from measures of the natural wet-bulb temperature (Twb), black globe temperature (Tbg), and dry bulb air temperature (Tdb) using the following weighted formula:
WBGT = 0.7 (Twb) + 0.2 (Tbg) + 0.1 (Tdb)
When indoors the formula simplifies to 0.7 (Twb) + 0.3 (Tbg). The equation emphasizes the strong influence of air water vapor content on human thermoregulation (sweat evaporation) in the heat, which is an extension of the same fundamental observation made more than a century ago (15). Because NBC protective clothing and body armor create situations where sweat evaporation is impaired, WBGT adjustments for clothing have also been established for the military (16).
In an effort to develop a thermal strain index specifically applicable to aviation, Harrison et al. (17) examined the relationship between ground weather and cockpit conditions across a broad range of WBGT at altitudes less than 3,000 ft. The following equation was developed from the relationship between ground WBGT (WBGTgr) and cockpit WBGT (WBGTcp):
WBGTgr = (WBGTcp − 0.333)/1.183
On the basis of WBGTgr and WBGTcp relationship, a practical thermal strain index for aviation was developed known as the Fighter Index of Thermal Stress (FITS) (18). The FITS assumes that Tbg is greater than Ta by 10°C (clear skies) and
requires only two ground measurements to estimate cockpit thermal stress:
requires only two ground measurements to estimate cockpit thermal stress:
FITS = 0.83 (Twb) + 0.35 (Ta) + 5.08
FITS temperatures between 32°C and 38°C represent a “caution zone” where operations are permissible for pilots when adhering to proper precautions (18). FITS temperatures greater than 38°C represent a “danger zone” for flight operations that recommend cancellation of low-altitude missions and strict limits on high-altitude flights (18). It is important to remember that FITS provides only general guidance, but it does specifically address the unique occupational circumstances of aviators.
The following FITS procedures are designed to minimize heat stress impact (18):
FITS caution zone (between 32°C and 38°C)
Encourage crews to drink water before cockpit entry, during standby, and in flight
Be alert to symptoms of heat stress
Avoid exercise 4 hours before takeoff
Precool cockpits by means of air-conditioning the ground carts
Assign alternate crewmembers to perform preflight aircraft inspection
Keep the sun out of transparencies by using rolling roofs or fabric covers
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree