Highlights
- •
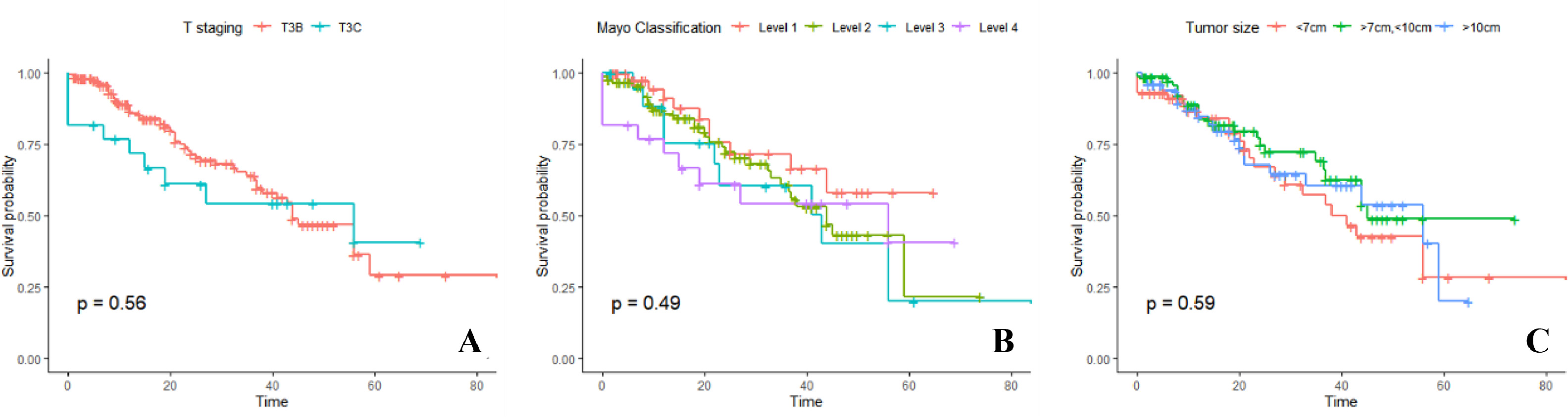
Regarding the controversy over the prognostic value of the primary tumor, our study supports that the level of IVCTT and tumor size have no significant prognostic value.
- •
For patients with RCC and IVCTT, the primary tumor score demonstrates promise in reflecting the prognostic value of local lesions.
- •
the model we proposed can accurately predicted OS with C-index of 0.77 and the AUC of time-dependent ROC for 1, 2, and 3year OS were 0.80, 0.81, and 0.78.
- •
For patients in high-risk group classified by our model, postoperative adjuvant therapy significantly improved the survival( P = 0.02) compared to low-risk group( P = 0.42).
Abstract
Background
Radical surgery can achieve remarkable improvements in the survival of patients with renal cell carcinoma (RCC) and inferior vena cava tumor thrombus (IVCTT); however, not all patients can obtain the desired results. Therefore, identifying patients with poor survival after surgery is crucial for guiding follow-up adjuvant therapies and patient counseling.
Objective
To evaluate the impact of primary tumor score based on tumor necrosis and tumor thrombus morphology on overall survival (OS), and create a postoperative prognostic model for patients with RCC and IVCTT.
Methods
This retrospective study included 182 patients with RCC and IVCTT who underwent radical nephrectomy and thrombectomy (RNTE). Preoperative contrast-enhanced computed tomography (CT), magnetic resonance imaging (MRI), ultrasound imaging, and clinical records were collected. Kaplan-Meier analysis was used to evaluate the overall survival (OS). Prognostic factors for OS were identified by univariate and multivariate analyses using the Cox proportional hazards regression model. A nomogram was developed and internally calibrated using the bootstrap resampling method.
Results
The mean follow-up time was 24.1 months (1–84.5 months), and 34.1% (62 of 182) of the patients died of all causes. The primary tumor score possesses a superior prognostic value for the primary tumor compared with the level of IVCTT and tumor size. Multivariate Cox regression analysis showed that primary tumor score, distant metastasis, nonclear cell subtype, sarcomatoid degeneration, preoperative anemia grade, and ASA level were independent prognostic factors. Based on these factors, a nomogram was built; the concordance index was 0.77, and the AUC for predicting 1–3 years OS were 0.80, 0.81, and 0.78, respectively.
Conclusions
Primary tumor score is a independent prognostic factors for patients with RCC and IVCTT. Combined with 5 easily acquired prognostic factors, a postoperative nomogram was developed and internally validated, and can be used to select patients who may benefit from adjuvant therapy or aggressive surveillance regimens.
1
Introduction
The prevalence of inferior vena cava tumor thrombus (IVCTT) in renal cell carcinoma (RCC) patients ranges from 4% to 10%. [ ] Radical nephrectomy with thrombectomy (RNTE) is the only curative treatment for these patients, even for metastatic patients, radical surgery can significantly improve overall survival (OS) [ ]. However, aggressive resection does not always guarantee satisfactory survival benefits, which vary significantly, with 5-year overall survival rates ranging from 25% to 71% [ ]. Therefore, selecting patients who may benefit from postoperative adjuvant therapy or aggressive surveillance regimens is critical for the accurate improvement of the survival rate.
Many studies have laid the foundation for exploring the prognostic predictors of patients with RCC and IVCTT; among these, how to represent the prognostic value of tumor thrombus remains controversial. From the perspective of tumor thrombus extent, the current 8th edition of the AJCC TNM staging system categorizes patients with RCC and IVCTT into T3b and T3c classifications based on whether the tumor thrombus extends beyond the diaphragmatic level. However, many studies have highlighted the inadequacy of the T3b/T3c method for survival prediction [ ]. Furthermore, follow-up research found that further subdividing the extent of the IVCTT into 3 levels based on the Mayo Clinic classification also has no prognostic value [ ]. Besides tumor thrombus, another factor of primary tumor that may help define its prognostic value is tumor necrosis(TN). A systematic review and meta-analysis [ ] reported that TN is strongly associated with poor survival and should serve as an independent prognostic factor for patients with RCC and IVCTT.
In this study, we aimed to explore the prognostic value of IVCTT from the perspective of thickness and combine it with the state of tumor necrosis to aid the selection of patients who may benefit from postoperative adjuvant therapy or aggressive surveillance regimens.
2
Patients and methods
Patients with RCC and IVCTT who underwent RNTE between June 2014 and July 2021 at Peking University Third Hospital were selected after obtaining approval from the Medical Ethics Committee of our hospital. Twenty-three patients were excluded because of missing follow-up and indeterminate tumor thrombus on preoperative imaging. Finally, 182 patients were included in this retrospective study.
2.1
Data collection
The clinical, pathological, and laboratory variables were collected through the electronic medical record system. Preoperative contrast-enhanced CT, MR, and ultrasound were reviewed to determine the features of the primary tumor.
2.2
Statistical analysis
Non-normally distributed continuous variables were described as the median and interquartile range (IQR). Normally distributed continuous variables are described as mean ± standard deviation. Categorical variables were calculated using frequency counts and percentages. The analysis of variance (ANOVA) test or Kruskal-Wallis test was used to compare the continuous variables. The Chi-square test or Fisher’s exact test was used to compare the categorical variables.
The Kaplan-Meier method was performed to analyze the survival rate, and the survival difference between groups was compared using the log-rank test. The max stat method (max stat package, R software) was used to determine the optimal cutoff value of continuous variables according to survival outcomes.
A multivariate Cox proportional hazards model was fitted for OS by including all the statistically significant covariates from the univariate Cox models. Using the regression coefficients of the independent prognostic factors from the multivariate Cox regression model, a nomogram for predicting the probability of survival was established. Harrell’s concordance index (C-index) and time-dependent receiver operating characteristic curves was used to evaluate predictive accuracy. Bootstrap validation (300 resamples) was conducted and calibration was assessed graphically using plots of the predicted probability of OS versus the actual proportion of surviving patients.
Two experienced radiologists independently assessed the presence of extensive necrosis and thickened tumor thrombus. Inter-observer agreement was evaluated using Cohen’s kappa coefficient. R software (version 3.5.0; http://www.r-project.org ) was used to establish and calibrate the nomogram and conduct other statistical analyses; P< 0.05 was considered statistically significant.
3
Results
A total of 182 patients were enrolled in this study, with a mean age of 60.01 years (SD: 10.19 years), and 74.2% of them were male. The median follow-up time after surgery was 24.01 months (IQR, 9.10–38.75 months), and 34.1% of patients(62 of 182) died of all causes. The median survival time was 45.0 months, the 1, 2, and 3 years survival rates were 84.8%, 70.4%, and 63.0%, respectively. The clinicopathological features of the included patients are shown in Table 1 .
| All patients (182) | ||
|---|---|---|
| Sex (%) | male | 135 (74.18) |
| female | 47 (25.82) | |
| Age (mean (SD)) | 60.01 (10.19) | |
| BMI (median [IQR]) | 23.54 [21.29,26.20] | |
| degree of anemia(%) | 0 | 102 (56.04) |
| 1 | 54 (29.67) | |
| 2 | 14 (7.69) | |
| 3 | 9 (4.95) | |
| 4 | 3 (1.65) | |
| The side (%) | left | 49 (26.92) |
| right | 133 (73.08) | |
| Tumor diameter (median [IQR]) | 8.6 [6.6,10.3] | |
| necrosis (%) | Present | 104 (57.14) |
| Absent | 78 (42.86) | |
| IVCTT level-Mayo (%) | 1 | 47 (25.82) |
| 2 | 94 (51.65) | |
| 3 | 19 (10.44) | |
| 4 | 22 (12.09) | |
| IVCTT level-T stage (%) | T3B | 160 (87.9) |
| T3C | 22 (12.1) | |
| regional lymph node (%) | absent | 73 (40.11) |
| present | 109 (59.89) | |
| metastasis at surgery (%) | absent | 129 (70.88) |
| present | 53 (29.12) | |
| Pathological Subtypes (%) | cc-RCC | 157 (86.26) |
| ncc-RCC | 25 (13.74) | |
| Sarcomatoid degeneration (%) | absent | 139 (83.23) |
| present | 28 (16.77) | |
| Nuclear grading (%) | 1 | 4 (2.23) |
| 2 | 59 (32.96) | |
| 3 | 72 (40.22) | |
| 4 | 44 (24.58) | |
| thickening degree (median [IQR]) | 1.51 [1.19,1.82] |
3.1
The prognosis controversial of the level of IVCTT and tumor size
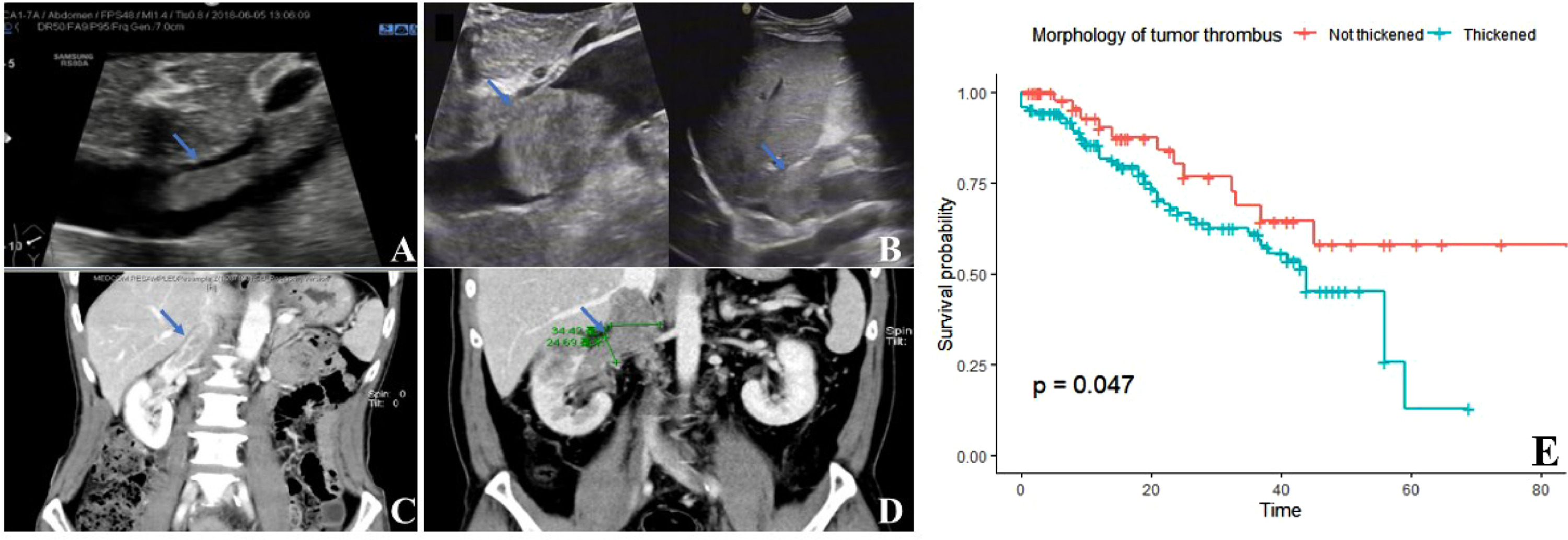
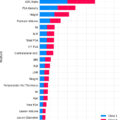
The current 8th edition of the AJCC TNM staging system categorizes patients with IVCTT into T3b and T3c based on whether the tumor thrombus exceeds the diaphragmatic level. However, this classification has been found to be insufficient for the prognosis of patients who undergo RNTE [ ]. Follow research also found that the Mayo Clinic classification, which further subdivided the height of the IVCTT by 3 levels, is also inadequate for prognosis [ ]. Consistently, our study demonstrated that the extent of the tumor thrombus remains without prognostic value for postoperative stratification. ( Fig. 1 A, Fig. 1 B). In our cohort, we found that tumor size had no significant prognostic value ( Fig. 1 C), which is consistent with the findings of previous studies [ , , ].
3.2
The establishment of the primary tumor score
3.2.1
Thickness of IVCTT
In clinical practice, the morphology of tumor thrombus varies from person to person and can be described as a cylindrical shape with significantly different thicknesses ( Fig. 2 A–D). The thickness degree(TD) indicates the extent to which the tumor thrombus grows along the short axis after entering the inferior vena cava; in other words, it indicates whether the IVCTT is skinny or chubby. The measurement of TD is shown in Fig. S1 . Range from 0,25 to 5.90, TD demonstrated varied morphological features. The best cut-off value of TD for indicating survival in our cohort was 1.23 ( Fig. S2 ), and accordingly, 129 of our patients were classified as having a chubby thrombus, and 53 were classified as having a skinny thrombus. The difference in survival between the 2 groups was significant ( Fig. 2 E).