Introduction
Osteosarcopenia is the combined diagnosis of both osteoporosis and sarcopenia, both of which are conditions associated with aging . Sarcopenia is currently defined by the European Working Group on Sarcopenia in Older People (EWGSOP) (2019) as low muscle strength, quantity, and performance; as defined by performance on specified functional tests . Sarcopenia is known to lead to increased risk of falls, mortality, frailty, and poor function . It is also associated with type 2 diabetes , cardiac cachexia , and metabolic syndrome . Osteoporosis is a condition of low bone mineral density (BMD), Specifically, it is diagnosed by a dual-X-ray absorptiometry (DXA) T score of less than − 2.5. This means that the BMD is 2.5 standard deviations or more below what would be expected at peak bone mineral density (BMD) in young adulthood. Osteoporosis is a condition of reduced bone strength, so it increases the risk of low trauma bone fractures. Hip and vertebral fractures are associated with increased morbidity and mortality .
With an aging global population, the incidence of osteosarcopenia is increasing, with subsequent large costs to the affected individual and to society . Recent estimates of osteosarcopenia prevalence include 5%–37% of community-dwelling Australian adults over the age of 65 years , one-third of older adults in Iran over the age of 60 years , and 10%–15% of 75 year old men and women in China .
There has been the suggestion that a diagnosis of osteosarcopenia may carry a higher health burden than having either osteoporosis or sarcopenia alone. Persons with both osteoporosis and sarcopenia are likely to be the frailest individuals who are at most risk of fractures, falls, and are most likely to live in a nursing home . For instance, one study found that mortality risk was 1.5 times higher in those with osteosarcopenia, compared with those without either osteoporosis or sarcopenia . However, another study found that those with osteosarcopenia had similar falls and fracture risk with those having osteoporosis or sarcopenia alone .
Adequate vitamin D concentration is known to be important for ensuring both bone and muscle health . Therefore, it is important to establish whether vitamin D deficiency, with concurrent high PTH concentration, is a candidate for influencing the development of osteosarcopenia. Of concern, there is a global epidemic of vitamin D deficiency, with one study finding that less than 50% of the global population in winter are sufficient in 25(OH)D (defined as > 50 nmol/L) . Therefore, if vitamin D status does influence the development of osteosarcopenia, it could be an important modifiable factor to address as part of osteosarcopenia treatment and prevention.
Vitamin D
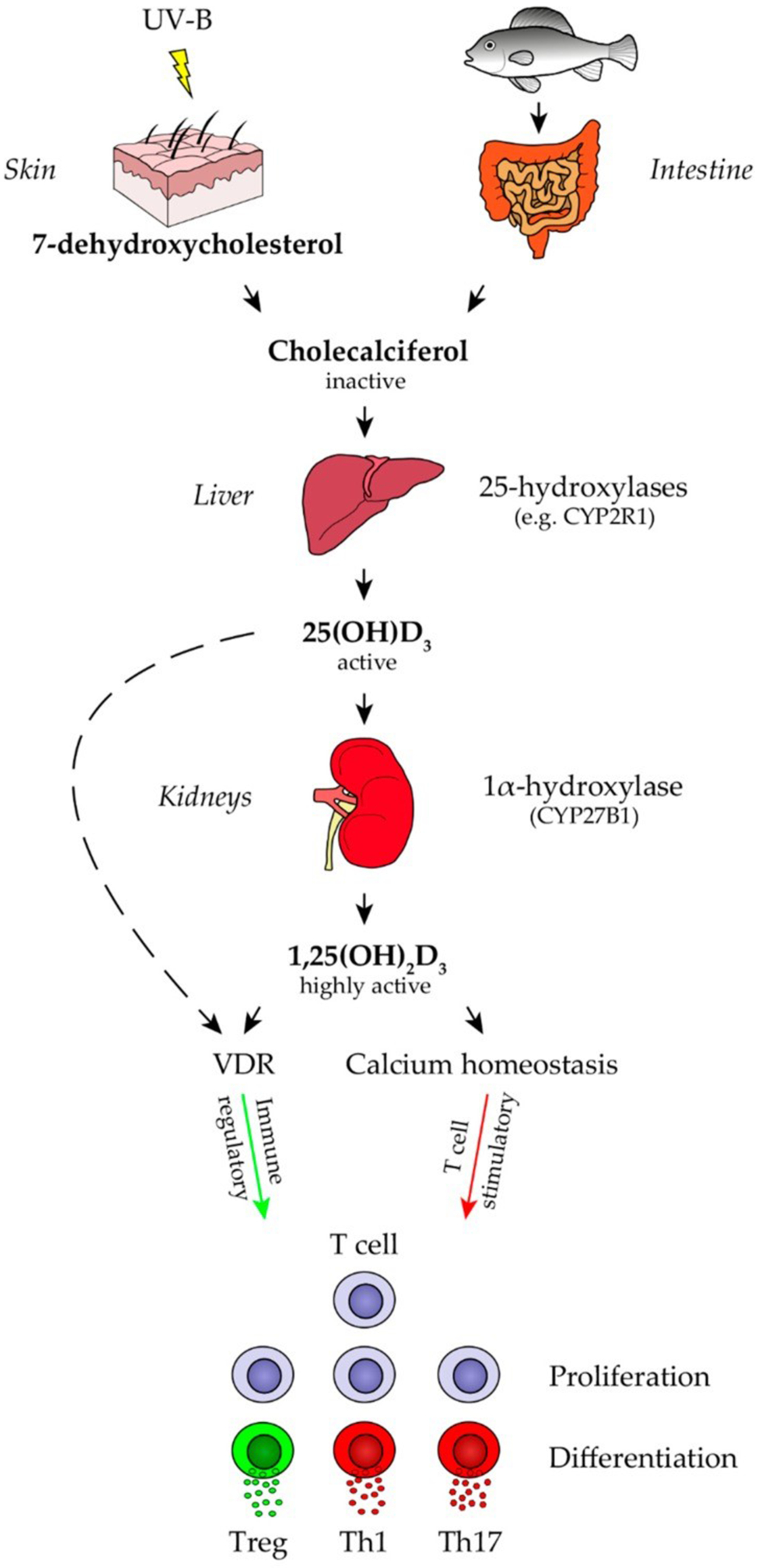
Vitamin D is a prohormone, rather than a vitamin, with clear endocrinological functions in the body. It is ingested from the diet in relatively small amounts, but the main source for most people is dermal production under the action of ultraviolet-B (UVB) radiation on the skin. The active hormone, 1,25-dihydroxy vitamin D (1,25(OH) 2 D), is produced from the hydroxylation of 25-hydroxyvitamn D (25(OH)D) in the kidney ( Fig. 1 ). There are multiple vitamin D metabolites in the body, but the most measured are 25(OH)D and 1,25(OH) 2 D.
The gold standard marker of vitamin D deficiency is 25(OH)D concentration . This is because the concentration of 1,25(OH) 2 D is highly regulated in the blood. Conversely, 25(OH)D is not tightly regulated and in serum or plasma it is a proxy estimate of the body’s store of vitamin D. However, the level to which it accurately reflects tissue saturation with vitamin D is unclear.
Vitamin D deficiency has been associated with increased risk of a wide range of health conditions, including cancer, heart disease, and osteoporosis; as well as autoimmune conditions and infectious diseases . Vitamin D comes in two forms, vitamin D 2 (from plant and fungal sources) and vitamin D 3 (usually from animal dietary sources, as well as being the form produced dermally). There are few natural rich sources of vitamin D in the diet, the most concentrated ones being oily fish, and to a lesser extent eggs and meat. Vitamin D intake from diet varies by gender, age, and the supplementation and fortification policies of individual countries . Higher intakes are generally seen in countries with high fish or vitamin D supplement consumption, or with mandatory vitamin D food fortification policies . Of concern, vitamin D deficiency is very common in older people in some parts of the world. For example, a systematic review and meta analysis reported the following average 25(OH)D concentrations in people aged over 65 years old: Asia/Pacific (66 nmol/L); Europe (52 nmol/L); Middle East (38 nmol/L), and North America (71.7 nmol/L) .
These estimates may contain few frail individuals in nursing homes, so maybe an overestimate. However, they do illustrate that in Europe and the Middle East, a significant number of older individuals have 25(OH)D less than 50 nmol/L (so are deficient using the European Food Safety Agency (EFSA) recommended serum or plasma concentration of > 50 nmol/L ). Vitamin D deficiency is particularly common in older people in nursing homes or receiving home personal care. For example, a study in Japan found that 15%–20% of older individuals receiving home personal care had vitamin D deficiency in winter (defined as < 30 nmol/L) . With aging, there is some evidence of a reduced ability to produce vitamin D in the skin, with production falling by up to 50% between young childhood and age 60 years . Sunlight exposure may also be low for those living in nursing homes, suggested by the fact that a study in the Netherlands (latitude 52.2°N) found low 25(OH)D was low (median of around 15 nmol/L) all year round and did not show the expected seasonal variation .
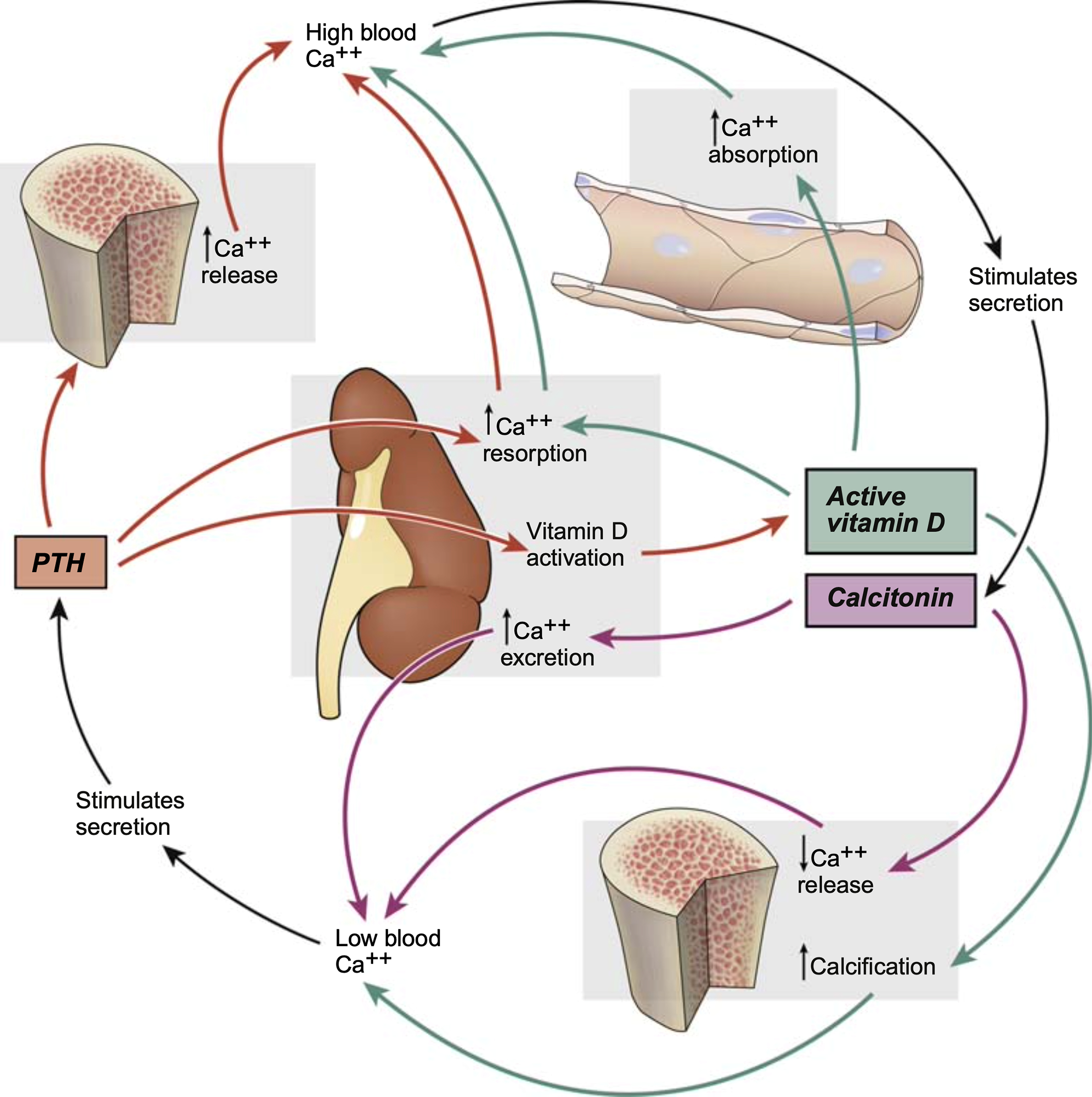
Vitamin D and PTH—Overview of the regulation of calcium metabolism
The physiological regulation of calcium concentration is crucial for life. Serum ionized calcium must be strictly maintained between 2.2 and 2.6 mmol/L. When serum ionized calcium is too low, PTH is released, leading to increased renal reabsorption of calcium. Increased 1,25(OH) 2 D concentration leads to increased calcium absorption from the gut. Increased PTH leads to loss of calcium from bone by increased osteoclast activity ( Fig. 2 ). These actions lead to a normalization of serum ionized calcium. Conversely, when serum ionized calcium is too high, the hormone calcitonin is released from the thyroid, which stimulates the uptake of calcium into bone tissue by inhibition of osteoclast activity. There is also reduced renal reabsorption of calcium and increased calciuria.
Vitamin D and osteoporosis/osteopenia
Vitamin D has a clear role in bone health . Low 25(OH)D concentration is a known cause of secondary hyperparathyroidism and consequent high bone turnover . For 25(OH)D concentrations, 50 nmol/L has been suggested as the recommended minimum for patients with osteoporosis by the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) . They also suggest a minimum of 75 nmol/L for fracture prevention .
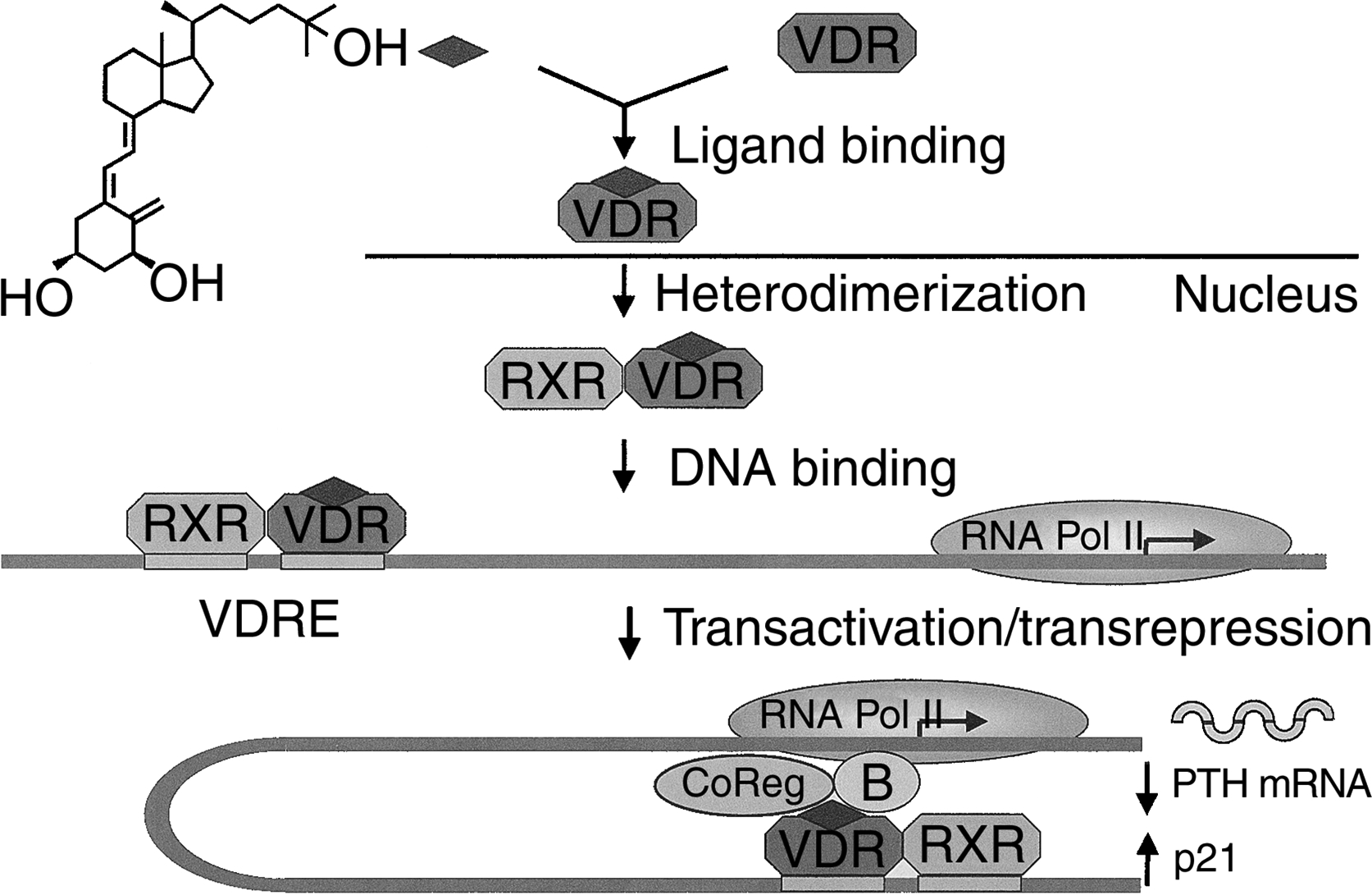
In addition to its role in regulating calcium metabolism and ensuring adequately mineralized bone, 1,25(OH) 2 D promotes other aspects of bone health via the vitamin D receptor (VDR). This is a nuclear hormone receptor that is present throughout the body, including in bone tissue , and acts as a transcription factor, affecting the expression of multiple genes ( Fig. 3 ). The 1,25(OH) 2 D ligand binds to the VDR, which heterodimerizes with the retinoid X receptor (RXR) . It then binds to vitamin D response elements (VDRE), which instigate gene transcription . There are also direct effects of 1,25(OH) 2 D on the activity of bone cells, which affects calcium transport and signaling of other molecules with knock-on effects on bone tissue function.
There is some evidence that vitamin D supplementation improves bone strength. For example, one peripheral Quantitative Computer Tomography (pQCT) study found that vitamin D supplementation slowed decline in tibial cortical thickness in postmenopausal women . In another pQCT study, there was a benefit of supplementation for bone microarchitectural strength (e.g., trabeculae) but not for overall areal BMD . In terms of DXA studies, one study found that a 1000 IU/d vitamin D supplement attenuated hip bone loss , with a secondary analysis of this data showing that vitamin D supplementation only benefited BMD when the participants had a 25(OH)D concentration of ≤ 30 nmol/L . However, another DXA study found a detrimental effect of high dose vitamin D supplementation (4000–10,000 IU/d) on BMD . Moreover, some studies have found no beneficial effect of vitamin D supplementation on BMD , including two mendelian randomization studies which have found no causal relationship between 25(OH)D concentration and neither femoral neck nor lumbar spine BMD nor total body BMD .
For osteoporotic fracture, there has been a relatively large amount of research showing an inverse association between 25(OH)D concentration and fracture prevalence. In observational studies, lower serum 25(OH)D has been associated with higher fracture risk, for hip fracture , all fractures combined and for faster BMD loss . However, if individuals are calcium deficient then calcium may also need to be supplemented for vitamin D supplements to be able to benefit bone health. A systematic review and meta analysis of randomized controlled trials found that 800 IU of vitamin D and 1200 mg of calcium per day were effective in reducing fracture risk (RR = 0.87 (95% CI 0.77–0.97)) and slowing hip BMD loss in adults aged 50 years or older . Similar results were found in a meta analysis by Avenell et al. (2014) who found a benefit of vitamin D supplementation on fracture prevention in older men and women, but only when calcium was also supplemented . However, some fracture risk systematic reviews and metaanalyses still show no effect of vitamin D supplementation (with or without calcium) on fracture risk in community-dwelling older adults or suggest that only those with specific risk factors should be supplemented . Overall, the situation is complicated in that vitamin D supplements may only reduce fracture risk when calcium is also supplemented and may only benefit certain high-risk groups, such as older people living in institutions .
Vitamin D and sarcopenia
Vitamin D, via the VDR, is critical for normal myocyte function . In animals, myocyte-specific vitamin D receptor (mVDR) null mice have been shown to have poor muscle function and sarcopenia .
Human studies have assessed whether 25(OH)D concentration is associated with either muscle strength or diagnosed sarcopenia. In observational studies, one study found that in older men, and in both sexes at a very advanced age, low baseline of 25(OH)D may be associated with an increased decline in muscle strength . In sarcopenic older adults, lower overall muscle mass and increased loss of lean mass have been associated with lower 25(OH)D concentration. Two studies found an association between 25(OH)D and sarcopenia or skeletal mass in women only . In older adults (60 years or over) 25(OH)D concentrations < 40 nmol/L were associated with worse musculoskeletal function than those with 40–94 nmol/L . Another study found increased odds of sarcopenia in middle-aged and older men and women with lower 25(OH)D concentrations .
Alternatively, some studies have found that 25(OH)D concentration is only associated with one type of muscle strength. For example, Meng et al. (2017) found no association between 25(OH)D and appendicular muscle mass, but there was a positive association with grip strength . However, one study found an association between low 25(OH)D and reduced muscle mass and poorer physical performance but not frank sarcopenia itself . Finally, a systematic review and meta analysis of observational studies found lower 25(OH)D concentrations in sarcopenic adults than nonsarcopenic controls . Of note, some studies have found no association between 25(OH)D concentration and muscle strength or function. For example, one study found no association between grip strength in men and women over 50 years old . Similarly, in men aged 40–79 years, another study found that 25(OH)D was not associated with the annual change in grip strength, gait speed, or appendicular lean mass or incident sarcopenia .
There have been few vitamin D supplementation trials assessing sarcopenia as an outcome , but one trial found that vitamin D supplementation led to improved appendicular muscle mass but there was no increase in grip strength in presarcopenic older men and women . Another trial found improved muscle strength and reduced loss of muscle mass in postmenopausal women . However, one trial in 45–60-year old early postmenopausal women found no effect of vitamin D supplementation on muscle mass or muscle strength . Similarly, another trial in 50–79-year-olds found no effect of vitamin D supplementation of 50,000 IU monthly for 1 year on trunk muscle function .
Vitamin D and osteosarcopenia
There are no human observational studies or randomized controlled trials to date assessing the association between vitamin D and osteosarcopenia as a syndrome in itself . There are only separate studies on vitamin D and osteoporosis, or vitamin D and sarcopenia (as discussed above). However, recent research in vitamin D deficient, senescence-accelerated mouse prone 6 (SAMP6)rodents (who have both senile osteoporosis and muscle aging, so are a potential model for osteosarcopenia) has found a higher grip strength and muscle mass in those exposed to UVB radiation than in those not exposed to UVB radiation . This suggests that dermal vitamin D production leads to improved muscle strength in vitamin D deficient aged rodents. However, may have been other biological effects from the radiation itself that are not linked with vitamin D production which may explain the enhanced muscle strength. The authors of the above paper suggest that UVB irradiation may help improve function in those with osteosarcopenia . However, it is unclear as to whether similar observations would be seen in humans, and whether oral dosing of vitamin D would have the same effects.
A recent human study found beneficial effects of resistance training on function in older men with osteosarcopenia, when supplemented with vitamin D and protein . However, as all participants were supplemented with vitamin D it is not possible to show whether the exercise effect was dependent on vitamin D or not. Finally, in kidney transplant patients, vitamin D concentration has not been found to be predictive of having osteosarcopenia or not, once confounders such as age and physical activity levels were controlled for . Therefore, there is only limited literature on the subject and the results are conflicting.
PTH, osteoporosis, sarcopenia and osteosarcopenia
Human parathyroid hormone is an approved treatment for osteoporosis, with a systematic review and meta analysis demonstrating increased BMD at all skeletal sites after administration of PTH treatment, except for the radius . Although long-term high PTH concentrations are detrimental to the bone, intermittent administered PTH actually increases osteoblast activity and number . In terms of endogenous, long-term exposures to high PTH, in older people, increased PTH concentration and lower 25(OH)D have been associated with being sarcopenic and longitudinal data shows that lower baseline 25(OH)D in older men is associated with higher sarcopenia incidence over 5 years . Sarcopenic obesity and frailty are associated with higher PTH and lower 25(OH)D. One study found an association between PTH and sarcopenia in men only . However, another study assessing both men and women found no association between PTH and odds of sarcopenia after BMI adjustment .
As discussed above, high PTH is associated with osteoporosis and sarcopenia as separate entities. However, it is unclear as to whether PTH is associated with the development of osteosarcopenia . Few research publications have specifically assessed PTH and osteosarcopenia, rather than just osteoporosis and sarcopenia separately. One cross-sectional study found that persons with osteosarcopenia had a higher PTH than those with just sarcopenia, just osteoporosis or neither osteoporosis nor sarcopenia . Similarly, the osteosarcopenia group had higher falls susceptibility than the other groups when PTH was high (> 6.8 pmol/L) .
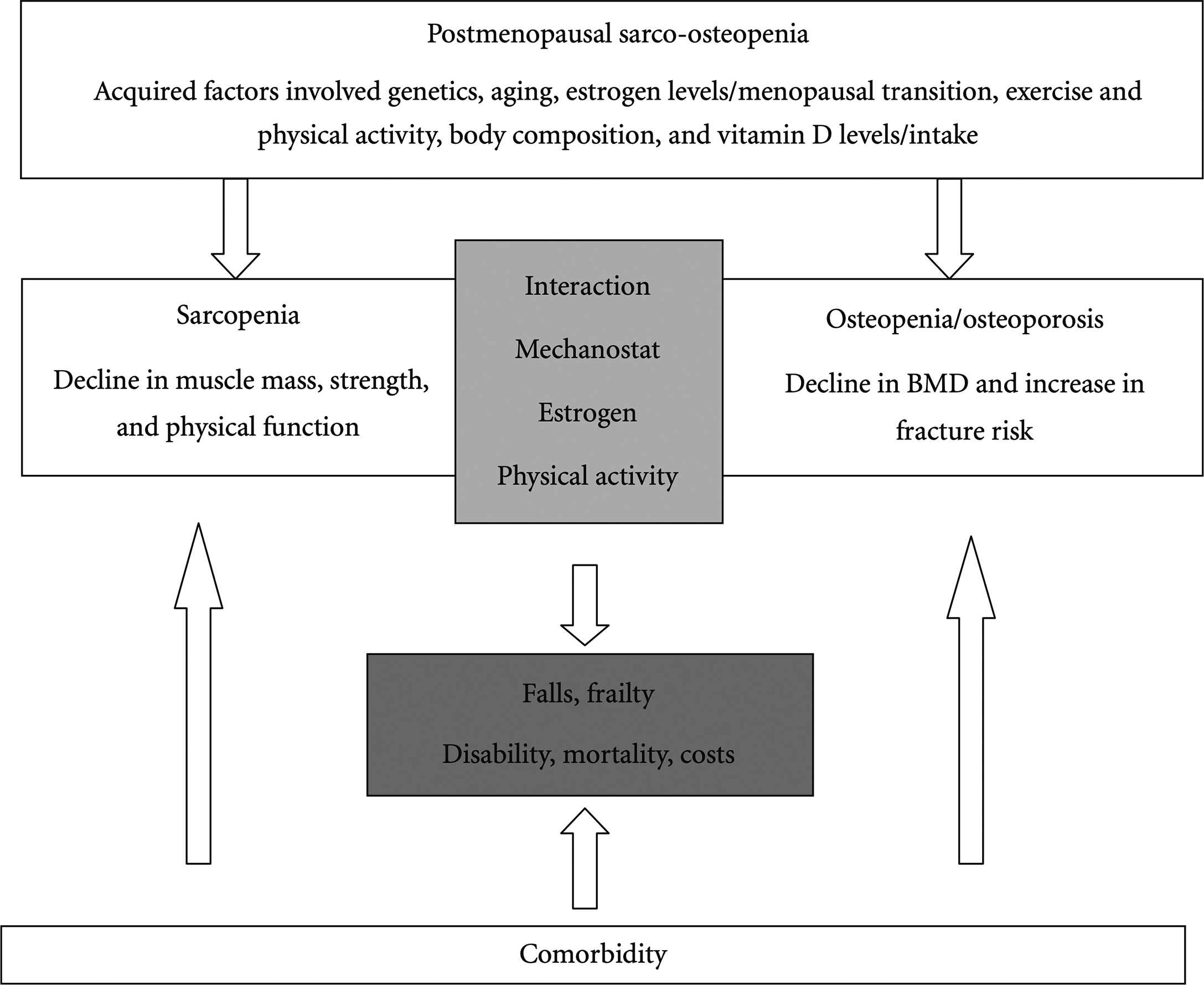
Vitamin D, PTH, bone, and muscle interactions
There is much cross-talk between muscle and bone. The muscle provides the mechanical stimulus that regulates bone modeling . There is also non mechanical communication between muscle and bone. For instance, muscle releases a series of mediators such as IGF-1, myostatin, osteoglycin, FAM5C, irisin, osteonectin, FGF2, IL-6, IL-7, IL-15, and MMP-2, which have an effect on bone metabolism . Equally, bone releases mediators such as IGF-1, sclerostin, osteocalcin, MGF, VEGF, and HGF . Both sarcopenia and osteopenia/osteoporosis share common antecedent factors, such as aging, genetics, estrogen, physical activity, 25(OH)D, and anthropometry ( Fig. 4 ) . Moreover, as discussed above, long-term vitamin D deficiency and high PTH concentration negatively affect both muscle and bone health. More research is required into the associations between sarcopenia, osteopenia/osteoporosis, and osteosarcopenia, in order to develop and tailor the correct treatments for the right individuals, and to instigate effective prevention strategies in populations.