Patricia W. Slattum, Kelechi C. Ogbonna, Emily P. Peron
The Pharmacology of Aging
Each day, worldwide, older adults consume millions of doses of medications. This remarkable amount of medication use benefits many older people by preventing and treating disease, preserving functional status, prolonging life, and improving or maintaining good quality of life. However, this level of medication exposure may harm older people via adverse drug reactions and is associated with other problems, such as drug interactions. The responses of older individuals to drugs, both beneficial and harmful, are partially dependent on age-related physiologic changes that influence how the body handles a given drug (pharmacokinetics) and what a drug does to the body (pharmacodynamics). To obtain the desired therapeutic response and prevent drug-related problems, it is also useful to have an understanding of drug use patterns in the geriatric population. Therefore, this chapter first examines the epidemiology of drug use in older adults around the world, followed by age-related alterations in drug pharmacokinetics and pharmacodynamics, and finally drug interactions.
Epidemiology of Drug Use
In general, the number of medications (prescription and nonprescription) used by older adults is greater than the number used by younger persons.1–3 In the United States, older adults account for 13% of the population but for 34% of all prescription drugs dispensed.4 The number and type of medications used by older adults are based in part on their living situation and access to medications.
Living Situation
Community-Living Adults
Of adults aged 57 to 85 years in the United States, 81% have reported taking at least one prescription medication.5 Although the prevalence of medication users has not changed over time, the prevalence of polypharmacy (the use of multiple medications) has increased in recent years.6 On average, community-dwelling older adults take from two to nine medications.7 In the United States, race has been associated with differences in medication use among older adults, with older African Americans and Hispanic Americans demonstrating less use than older whites and Native Americans.1 Older women also take more medication overall than older men.8–10
Rates of polypharmacy also vary by country. In one international survey of adults 55 years and older, 53% of older adults in the United States reported taking four or more prescription medications.11 Approximately 40% of older adults in eight other countries—Australia, Canada, Germany, the Netherlands, New Zealand, Norway, Sweden, and the United Kingdom—reported the same medication-taking behavior, and those least likely to report this rate of medication use were from France (29%) and Switzerland (29%).
Also, the use of dietary supplements has been on the rise in the United States, with estimates of use in older adults rising from 14% in 199810 to 49% in 2006.5 Although dietary supplement use appears to be more common among women than men, rates of nonprescription use overall are similar, with 42% of men and women aged 57 to 85 years in the United States using nonprescription medication.5 Cardiovascular drugs were found to be the most commonly used medications among all prescription and nonprescription medications in the population studied.
Hospitalized Older Adults
Medication use by hospitalized older adults tends to be slightly higher than that of community-dwelling older adults. However, there is a paucity of information with regard to the types of medications used by older adults in this setting. Reported rates of prescription medication use among hospitalized older adults have ranged from a mean of 5 per patient in Italy12 and Ireland13 to 7.5/patient in the United States14 and Austria.15 One study, using pharmacy records from the University of Pittsburgh Medical Center, a tertiary academic medical center in southwestern Pennsylvania, identified the top 50 oral drugs prescribed for older hospitalized patients.16 Warfarin, potassium, and pantoprazole were the most commonly prescribed oral drugs.
Older Adults in Long-Term Care Facilities
The level of medication use by older adults in long-term care facilities (LTCFs) is generally higher than that of older adults living at home in the community. There is a notable disparity worldwide in the percentages of LTCF residents taking large numbers of medications. In the United States and Iceland, 33% of LTCF residents take 7 to 10 medications, whereas only 5% of residents exhibit this degree of use in Denmark, Italy, Japan, and Sweden.17 In one survey of United States LTCFs, 40% of residents (and 45% of those ≥85 years) received nine or more medications.18 Gastrointestinal agents, central nervous system agents, and pain relievers were the most commonly used agents among patients receiving polypharmacy in that study.
Although the use of multiple medications may be necessary in some patients, the potential for inappropriate prescribing and drug-related problems are of concern. Overuse of certain centrally active medications—namely, antipsychotics—can be a particular problem in the LTCF setting.19 In 1987, federal legislation was enacted in the United States that defined clear indications for appropriate prescribing of these agents and mandated close monitoring of them (Omnibus Budget Reconciliation Act [OBRA], 1987).20 In 2005, the U.S. Food and Drug Administration (FDA) added a black box warning to the labeling of second-generation antipsychotics regarding the increased mortality risk associated with their use in older adults with dementia. This labeling change was then expanded to include all antipsychotics (first and second generation) in 2008. There have been decreases in antipsychotic prescribing in LTCFs since then,21,22 but additional efforts are needed to continue to reduce antipsychotic use, particularly among patients at risk of significant harm, such as older adults with dementia.
Access to Medications
Universal public health insurance programs for older adults in Australia, Sweden, Canada, France, Germany, Japan, New Zealand, and the United Kingdom provide some level of drug benefit coverage, with the drug benefits differing in the amount of cost sharing, maximum amount of coverage, and specific pharmaceuticals covered.23 The U.S. health insurance program for older adults, Medicare, began coverage of outpatient drugs in 2006 via Medicare Part D. Although characterized by substantial copayments and an absence of coverage over a small but fixed drug cost range (the so-called doughnut hole), older adults in the United States are now protected from catastrophic out of pocket costs for outpatient drugs. This, in turn, has improved adherence and reduced the need for older adults to forgo necessities to purchase medications.24–26 Notably, in many developing countries, medicines are the largest household health expenditure. Moreover, the supply of medications in developing countries may be inadequate or too expensive for older adults to purchase.27,28
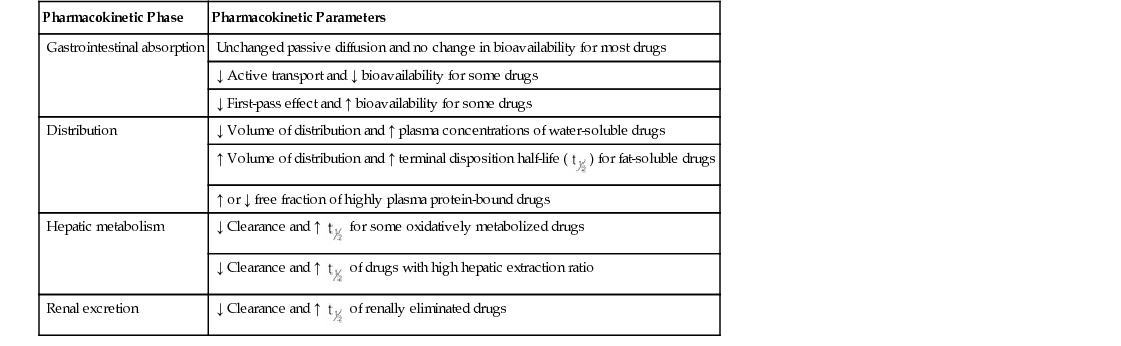
Altered Pharmacokinetics
Table 26-1 presents an overview of age-related changes in drug pharmacokinetics.29,30 This chapter details these changes in drug absorption, distribution, metabolism, and elimination. Frailty, a syndrome characterized by weight loss, fatigue, weakness, slowed walking speed, and low physical activity that is associated with advanced age and increased risk of adverse drug events, is probably more important than chronologic age as a risk factor for altered pharmacokinetics in older adults.31
Absorption
Numerous changes occur in the physiology of the gastrointestinal (GI) tract as a function of advancing age that might be expected to affect the absorption of drugs administered orally.29,32 Gastric pH rises because of the development of atrophic gastritis, as well as the use of acid-suppressive medications to treat age-related GI disorders, such as peptic ulcer and gastroesophageal reflux. Gastric emptying is somewhat delayed and decreases are seen in intestinal blood flow (30% to 40% from age 20 to 70 years), intestinal motility, and number of functional absorptive cells.
Most drugs administered orally are absorbed via the process of passive diffusion, a process minimally affected by aging. A few agents require active transport for GI absorption, and their bioavailability may be reduced as a function of aging (e.g., calcium in the setting of hypochlorhydria). Of more significance is the decrease in first-pass hepatic extraction that occurs with aging, resulting in an enhancement in systemic bioavailability for drugs such as propranolol and labetalol and reduced bioavailability of some prodrugs such as enalapril and codeine after oral administration.29,32 The bioavailability of drugs that are cytochrome P450 (CYP450), isoenzyme 3A4, and/or P-glycoprotein substrates (e.g., midazolam, verapamil) may be increased in older women, but no dosage adjustment recommendations have as yet been made.33 The effects of aging on modified-release dosage forms are not known, although absorption might be affected by changes in GI motility or pH for some dosage forms in some patients. The effects of aging on drug absorption from other sites of administration such as the rectum, muscle, and skin are poorly understood.
Distribution
A number of changes in physiology occur with aging that may affect drug distribution. Body fat as a proportion of body weight rises from 18% to 36% in men and from 33% to 45% in women from age 20 to 70 years, whereas lean body mass decreases by 19% in men and by 12% in women, and plasma volume decreases by 8% from age 20 to 80 years. Total body water decreases by 17% from age 20 to 80 years and extracellular fluid volume decreases by 40% from 20 to 65 years of age. In addition, cardiac output declines approximately 1%/year from age 30 years, and brain and cardiac vessel blood flow rates decline 0.35% to 0.5% and 0.5%/year, respectively, beyond age 25 years. Additionally, frailty and concurrent disease may result in substantial changes in the serum concentrations of the two major drug-binding plasma proteins—albumin, which binds acidic drugs, decreases, whereas α1-acid glycoprotein, which binds basic drugs, remains the same or rises.34
As a result of these factors, the volume of distribution of water-soluble (hydrophilic) drugs is generally decreased and that of fat-soluble (lipophilic) drugs is increased. Moreover, changes in volume of distribution can directly affect the loading doses of medications. For many drugs, loading doses will be lower in older versus younger patients and lowest in older white and Asian women (and thus use weight-based regimens routinely).33 Decreases in serum albumin concentration can lead to a reduction in the degree of plasma protein binding of acidic drugs, such as naproxen, phenytoin, tolbutamide, and warfarin, therefore increasing the unbound fraction of the drug. Increases in α1-acid glycoprotein because of inflammatory disease, burns, or cancer can lead to enhancement in the degree of plasma protein binding of basic drugs such as lidocaine, β-blockers, quinidine, and tricyclic antidepressants, thus reducing the unbound fraction of the drug. Provided there is no compromise in excretory pathways, these potential changes are unlikely to be clinically significant. However, plasma protein binding changes can alter the relationship of unbound (free) and total (unbound plus bound) plasma drug concentrations, making drug concentration interpretation more difficult. In these cases, the measurement of free plasma drug concentrations may be preferable to the usual use of total plasma drug concentrations.
Permeability across the blood-brain barrier may also be altered in older adults, affecting distribution of drugs into the central nervous system (CNS). Cerebrovascular P-glycoprotein is responsible in part for the transport of drugs across the blood-brain barrier. Studies using verapamil labeled with carbon-11 (a positron emitter) and positron emission tomography have demonstrated reduced P-glycoprotein activity in the blood-brain barrier with aging. As a result, the brain of older adults may be exposed to higher levels of drugs.35
Metabolism
Although drug metabolism can occur in numerous organs, most of the available data concern the effects of aging on the liver. Variations in drug metabolism and those resulting in altered drug clearance are a major source of variability in the response to medications in older adults.36,37 Hepatic metabolism of drugs depends on perfusion, liver size, activity of drug-metabolizing enzymes, transporter activity, and protein binding, all of which may be altered by aging. Drugs are metabolized by two types of reactions—phase I (oxidative reactions) and phase II (conjugative or synthetic reactions, wherein an acetyl group or sugar is conjugated to the drug to enhance its polarity, water solubility, and hence excretion via the kidneys). Generally, drugs that undergo phase I metabolism demonstrate reduced clearance, whereas drugs undergoing phase II metabolism are preserved with aging.36 For drugs with high intrinsic clearance (high hepatic extraction ratio), drug clearance is dependent on hepatic blood flow, is termed flow-limited metabolism. For drugs with low intrinsic clearance (low hepatic extraction ratio), clearance depends on hepatic enzyme activity, termed capacity-limited metabolism.
Age-associated reductions in hepatic blood flow can reduce the clearance of high hepatic extraction ratio drugs such as amitriptyline, lidocaine, morphine, diltiazem, and propranolol.29,36 Hepatic blood flow may decline by 20% to 50%, resulting in reduced clearance of drugs such as propranolol by 40% or more in older adults.31 Understanding the effect of age on the metabolism of drugs undergoing capacity-limited metabolism is more complex. For these drugs, total clearance depends on the fraction unbound in blood and intrinsic hepatic clearance. Many but not all studies report reduced size of the liver and reduced enzyme content in older adults.36 Total hepatic clearance for drugs with capacity-limited metabolism many be increased (e.g., ibuprofen, naproxen), reduced (e.g., lorazepam, warfarin), or unchanged (e.g., temazepam, valproic acid) with aging.36 Hepatic clearance of unbound drug rather than total hepatic clearance, which includes bound and unbound drugs, may be more relevant for understanding the effect of age on hepatic clearance.36 Numerous confounders such as race, gender, frailty, smoking, diet, and drug interactions can significantly enhance or inhibit hepatic drug metabolism in older adults.37 Frail older adults, for example, may experience reduced phase II metabolism. Although frailty remains challenging to define, it is characterized by reduced lean body mass, muscle loss, malnourishment, reduced functional status, and reduced endurance.36 Frailty is associated with inflammation, which may downregulate drug metabolism and transport.38 The interplay between drug transporters and drug-metabolizing enzymes may also play a role in the hepatic clearance of drugs with aging, but these relationships have remained largely unexplored.29
Elimination
Renal excretion is a primary route of elimination for many drugs and their metabolites. Aging is associated with a significant reduction in renal mass and number and size of nephrons. In addition, the glomerular filtration rate (GFR), tubular secretion, and renal blood flow decrease approximately 0.5%, 0.7%, and 1%/year, respectively, in those older than 20 years. At all ages, these three parameters are lower in women than in men.33 However, older adults are a heterogeneous group, with up to one third of healthy older adults having no decrement in renal function as measured by creatinine clearance, a surrogate for glomerular filtration. In addition, tubular secretion and glomerular filtration may not decline in parallel.39 Changes in kidney function with aging may be associated with hypertension or heart disease rather than with aging itself.29 The estimation of creatinine clearance (CrCl), using any of a number of equations, serves as a useful screen for renal impairment in lieu of the use of serum creatinine (SCr), which is an imperfect marker of renal function in older adults because of the reduction of muscle mass with advancing age (i.e., a normal serum creatinine level does not equate with normal renal function in older adults).40 One commonly used estimation equation for creatinine clearance used for dosage adjustment in older adults is the Cockcroft and Gault equation41:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 ) for fat-soluble drugs
) for fat-soluble drugs for some oxidatively metabolized drugs
for some oxidatively metabolized drugs of drugs with high hepatic extraction ratio
of drugs with high hepatic extraction ratio of renally eliminated drugs
of renally eliminated drugs