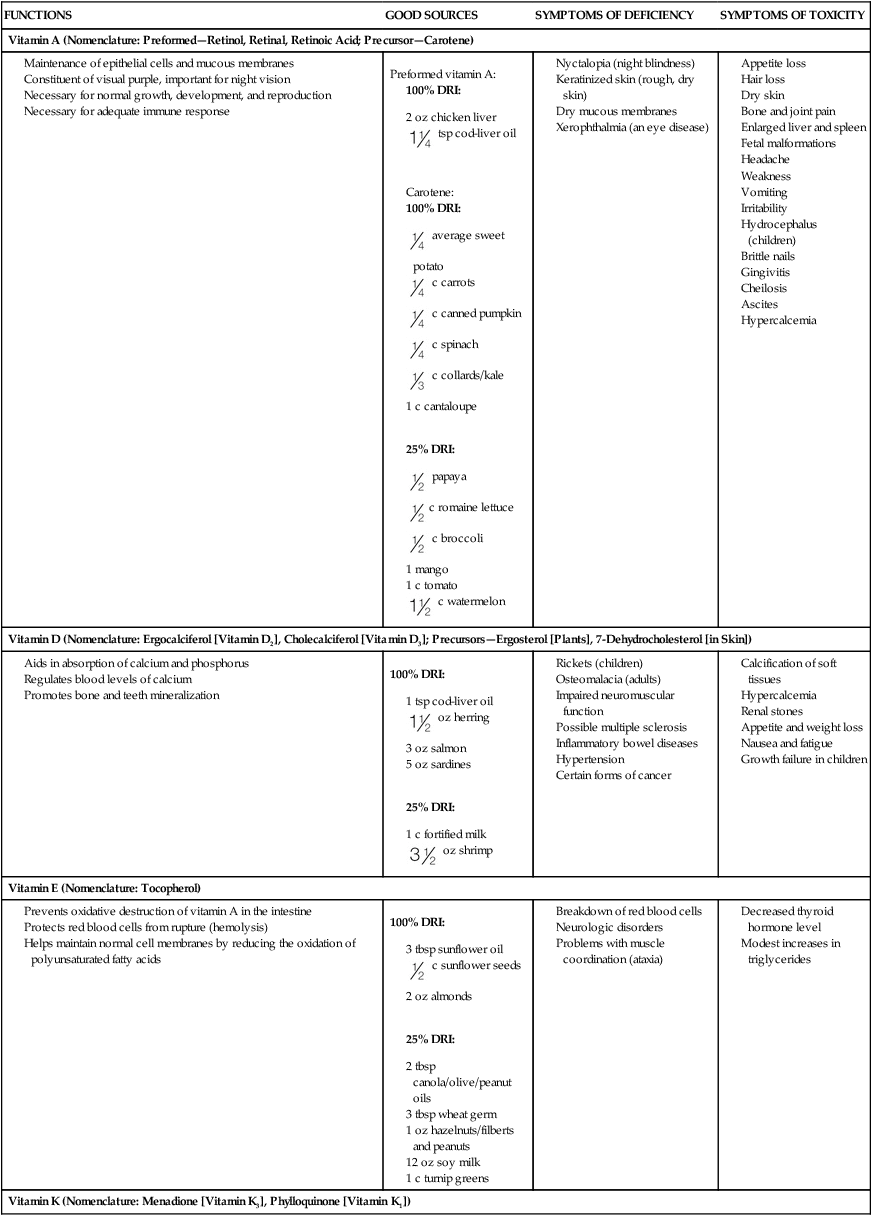
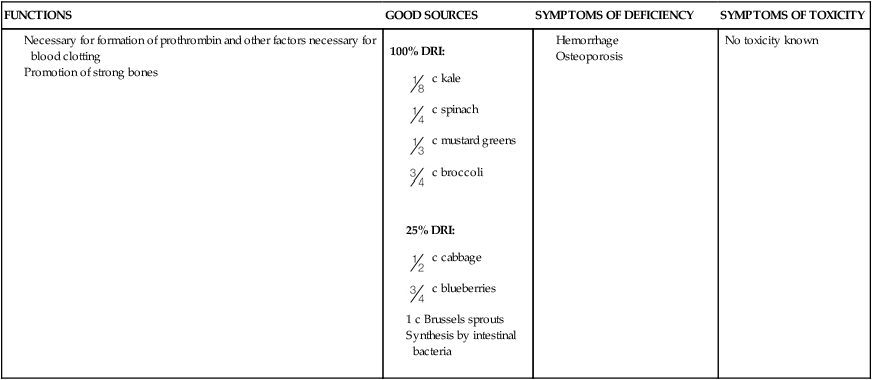
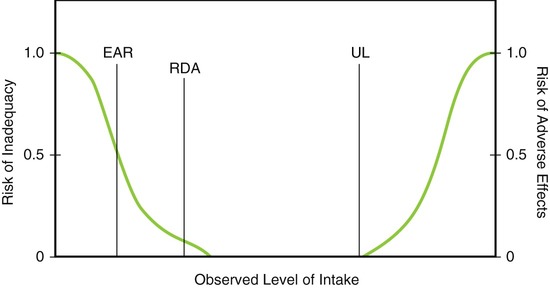
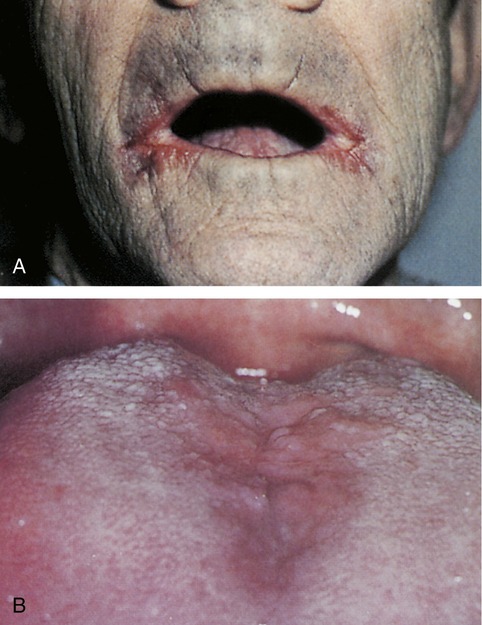
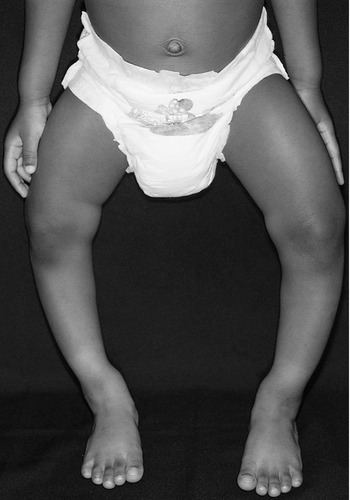
After completing this chapter, you should be able to: • Describe the main difference between the fat-soluble and water-soluble vitamins. • Recognize at least one known function of each of the vitamins and minerals. • List foods high in the various vitamins and minerals. • Recognize phytochemicals and their potential role in health. • Describe the potential concerns regarding supplements of vitamins and minerals and herbal products. • Describe how the nurse or other health care professional can most appropriately promote the intake of vitamins, minerals, phytochemicals, and supplements. Vitamins and minerals become available to body cells from foods we eat after the processes of digestion and absorption. Vitamins and minerals are integral to the function of metabolic enzymes at the cellular level for basic life processes (see Chapter 4). Food is the ideal medium for intake of vitamins and minerals. For example, it has been found that individuals consuming salads and other raw vegetables tend to have improved serum levels of vitamin E and the water-soluble vitamins C and folic acid along with a form of vitamin A called carotenoid (Su and Arab, 2006). Nuts are another source of many nutrients needed by the body and have been noted to improve health status. They contain a variety of compounds that can lower risk of heart disease: phytosterols that interfere with intestinal cholesterol absorption, healthy fats and fiber that lower the body’s production of cholesterol, folate that lowers homocysteine levels (see Chapter 7), and magnesium and potassium with naturally low levels of sodium related to lowered blood pressure (see Dietary Approaches to Stop Hypertension [DASH] diet, Chapter 7). These nutrients and other trace minerals found in nuts contribute to healthy bones and lower insulin resistance and the risk of diabetes (see Chapter 5). Nuts are also a good source of protein, and are vital to a healthy vegetarian diet. No vitamin and mineral supplement can include all of the healthy nutrients found in nuts and other unprocessed foods. The U.S. Recommended Dietary Allowances (RDAs) and Canadian Recommended Nutrient Intake (RNIs) have been replaced with the Dietary Reference Intakes (DRIs), the term used collectively to describe four primary measures of recommended dietary intake. The updated DRIs are now used by both the United States and Canada. Nutrient intake amounting to less than the lower end of the range of the DRIs may lead to nutrient deficiency. Intake amounting to more than the upper limit may give rise to toxic effects, especially with trace minerals (Figure 3-1). The DRIs should not be confused with requirements for a specific individual because requirements vary considerably. Problems such as premature birth, inherited metabolic disorders, infections, chronic diseases, and the use of medications may require special dietary modifications. The specific reference values that constitute the DRIs are as follows: Estimated Average Requirement (EAR): the amount of a nutrient estimated to meet half of healthy individuals’ needs based on life stage and gender. Recommended Dietary Allowance (RDA): the average daily dietary intake level that meets the nutrient requirement of more than 97% of the healthy population in a particular life stage and gender group. Adequate Intake (AI): a recommended intake of vitamins and minerals based on observations of nutrient intake by a group of healthy persons that is assumed to be adequate (when an RDA cannot be determined). The AI level is generally between the RDA level and the maximum safe amount. Tolerable Upper Intake Level (UL): the highest level of daily nutrient intake that is likely to pose no risk of adverse health effects in almost all individuals in the general population. Intakes above the UL are associated with increased risk of adverse reactions. Derived from UL are two newer methods described as the Observed Safe Level (OSL) and Highest Observed Intake (HOI). Reliance on nonfortified (see section below) food sources for vitamins and minerals offers little risk of ingesting toxic amounts and provides a good balance of vitamins and minerals. The MyPyramid Food Guidance System (see Chapter 1) is a strategy to plan healthy meals. Although there is debate about how best to portray recommended intake for the majority of the population through MyPyramid, the general goals are still sound. The 2005 Dietary Guidelines were updated to specifically recommend three whole-grain servings or half of the daily grain intake, along with increased quantities of fruits and vegetables to the equivalent of The body requires vitamins only in minute amounts, but proper growth and development and optimal health are impossible without them. Some vitamins may be synthesized by the body, but for the most part they must be supplied in the daily diet of normal healthy persons. Early attention was paid to the clear-cut manifestations of diseases caused by vitamin deficiencies (Figure 3-2). Vitamins are classified as body regulators because of the following functions: • Regulating the synthesis of many body tissues (bones, skin, glands, nerves, brain, and blood) • Participating in the cellular metabolism of macronutrients through their function with metabolic enzymes (chemicals the body produces to allow for basic life processes) as coenzymes and cofactors • Preventing nutritional deficiency diseases and allowing for optimal health at all ages • Serving as antioxidants to reduce damage at the cellular level from the process of oxidation (see Chapter 4) The absorption of fat-soluble vitamins is enhanced by dietary fat. Individuals who are afflicted with malabsorption of fat or who consume an extremely small amount of fat are at higher risk for development of fat-soluble vitamin deficiencies. The same applies to use of a weight loss medication, orlistat, that is now available for over-the-counter sale. This medication interferes with the digestion of fat (see Chapter 4) and has the potential to contribute to deficiency of fat-soluble vitamins (Filippatos and colleagues, 2008). The other form of vitamin A is the preformed version (retinol and retinyl palmitate as used in food fortification). Preformed vitamin A is found in animal products such as liver; milk fat as in whole milk, cream, and butter; and egg yolks. See Table 3-1 and Figure 3-3 for other specific food sources. Vitamin A is often added to foods in a process called fortification (see section below) and is found in supplements. Vitamin A in the preformed version is able to produce toxicity if ingested in large amounts, especially because it is readily stored in the body for up to 2 years. Some acne creams contain preformed vitamin A, which has been linked with birth defects; caution is advised for use of these creams among women of childbearing years. Table 3-1 Preformed vitamin A: 100% DRI: 100% DRI: 100% DRI: DRI, Dietary Reference Intake. *Amounts of foods listed meet the Dietary Reference Intake for adults ages 31 to 50 (largest amount used as reference) as rounded off to the nearest portion size to meet the DRI. Data from USDA Composition of Foods, Handbook No. 8 Series, Washington, DC, 1976-1986, Agricultural Research Service, USDA; U.S. Department of Agriculture, Agricultural Research Service: USDA National Nutrient Database for Standard Reference, release 17; Davis J, Sherer K: Applied nutrition and diet therapy for nurses, ed 2, Philadelphia, 1994, Saunders; and Mahan KL, Escott-Stump S: Krause’s food, nutrition, and diet therapy, ed 12, Philadelphia, 2008, Saunders. Retinol can be found in oil-based or water-based forms (water-miscible), emulsified, and in solid preparations. The non–oil-based forms of retinol are approximately 10 times as toxic as are oil-based preparations. This is due to increased absorption. The safe upper single dose of retinol in oil or liver seems to be approximately 4 to 6 mg/kg body weight. Chronic intake of 2 mg retinol per kilogram in oil-based preparations results in hypervitaminosis A, regardless of age (Myhre and colleagues, 2003). Food fortification with retinyl palmitate can lead to toxic levels of vitamin A in the body, called hypervitaminosis A. Retinoids (vitamin A and its derivatives) circulate in the body predominantly attached to retinol-binding protein (RBP). This allows transport of retinol from liver stores to body tissues. There are wide variations in carotenoid usage from one person to another due to a variety of factors such as absorption differences from specific foods consumed, certain medicines used, genetic and physiologic factors, and nutritional status. Conversion of provitamin A carotenoids into vitamin A is not 100% efficient, and good protein status is needed (Borel and colleagues, 2005). Vitamin A is important for healthy epithelial tissue (external skin and internal lining of the respiratory and gastrointestinal [GI] tract). Deficiency of vitamin A has long been known to increase the risk of infection and is associated with night blindness, as well as total blindness in many countries (see Chapter 14). It is now known that a good intake of vitamin A helps with bone growth, a healthy immune system, improved vision, and reproduction. Marginal vitamin A deficiency is common and can result in a form of iron deficiency. Marginal vitamin A intake by a breastfeeding mother can put the nursing offspring at risk for iron deficiency (Kelleher and Lonnerdal, 2005). It is beneficial for individuals with marginal vitamin A status to consume carotene-rich orange and green leafy vegetables with a low-fat diet. It has been shown this can normalize the body pool of vitamin A through increased absorption (Ribaya-Mercado and colleagues, 2007). Toxicity of vitamin A has been linked with cheilosis (see Figure 3-4), altered lipids, and hypercalcemia (excess calcium in the blood). Although vitamin A deficiency impairs bone growth, hypervitaminosis A causes bones to lose their calcium and can lead to osteoporosis (see Chapter 13). It can also cause severe liver damage (Castaño, Etchart, and Sookoian, 2006). In one situation after ingestion of large doses of vitamin A, the symptoms included muscle soreness, hair loss, nail disorder, and ascites (fluid accumulation in the peritoneal cavity of the abdomen), and with deteriorating health, the person further developed renal insufficiency, encephalopathy (brain degeneration), failure to thrive, and ultimately required liver transplantation (Cheruvattath and colleagues, 2006). Hypervitaminosis A caused hypercalcemia to develop in a toddler who had been treated for autism with massive doses of vitamin A, 100,000 IU daily for 3 months followed by a daily dose of 150,000 IU the 3 following months. His symptoms included vomiting, headache, fever, and skin abnormalities (Kimmoun and colleagues, 2008). Cases of children overdosing on vitamin A via excess intake of chewable vitamins has been reported and found to take months to normalize serum levels (Lam and colleagues, 2006). Treatment of hypervitaminosis A may be helped by use of vitamin E supplementation. This was found in a study of rabbits, with 2 weeks of supplementation effectively lowering the serum vitamin A levels (St Claire, Kennett, and Besch-Williford, 2004). Persons with cystic fibrosis and impaired pancreatic function are at risk of vitamin A deficiency because of fat malabsorption. However, avoidance of excess vitamin A intake is still important. One study of individuals with cystic fibrosis found that total preformed vitamin A intake exceeded the UL in the majority studied. Despite the fat malabsorption, the serum levels of vitamin A were found to be at levels for potential toxicity (Graham-Maar and colleagues, 2006). With the advent of industrialization in the late nineteenth century and the resulting long hours of working in factories endured by many children, rickets (bowing of the legs caused by body weight on soft leg bones) (Figure 3-5) became common enough that public health measures for its prevention began. The preventive measure used was the practice of giving children cod-liver oil. After vitamin D was chemically isolated in 1935, it was eventually added to milk, which ultimately replaced cod-liver oil as a means of preventing rickets (1 teaspoon of cod-liver oil provides about 100% of the DRI for vitamin D and vitamin A). Milk is an appropriate food to fortify with vitamin D because this vitamin greatly enhances the absorption of calcium, of which milk is one of the best sources. Rickets is again on the upsurge because of reduced intakes of fortified milk, decreased exposure to ultraviolet B sunlight in urban settings, and children increasingly spending their time indoors. Factors that influence vitamin D production in the skin include sunscreen use, skin pigmentation, time of day, season of the year, latitude, and aging. A total of 100 IU of vitamin D raises the blood level of 25-hydroxyvitamin D (25[OH]D) by 1 to 2 nmol/L (Cranney and colleagues, 2007). Thus children and adults who do not receive adequate vitamin D from sun exposure need at least 1000 IU/day vitamin D. There are different forms of vitamin D, including 1,25-dihydroxyvitamin D3 (1,25[OH][2]D], simply known as vitamin D2, which is generally the form of vitamin D in vitamin supplements. The biomarker for vitamin D stores is the serum level of 25(OH)D, with the minimum goal of 80 nmol/L or 32 ng/mL for optimal health. The evidence now appears strong enough to advise a higher vitamin D intake than the current DRI guidelines (see back of book). Based on a study in Nebraska, it was found that to achieve optimal vitamin D status an expected intake would be almost 2000 IU/day (Lappe and colleagues, 2006). Evidence is growing that a minimum of 800 IU of vitamin D is required to meet goals of optimal vitamin D status. Vitamin D has many physiologic roles beyond those related to bones, including regulating blood pressure and acting as a tumor suppressant. A study using data from the National Health and Nutrition Examination Survey (NHANES) found that although the mean levels of 25(OH)D were above the minimum goal, vitamin D levels were lower in women, persons 60 years of age and older, minorities, and persons with obesity, hypertension, diabetes mellitus, and elevated triglycerides. This was particularly true at the lowest levels of 25(OH)D (Martins and colleagues, 2007). There is evidence from a variety of studies that shows a 50% lower incidence of colon cancer with an intake of 1000 IU/day vitamin D or serum 25(OH)D levels greater than 33 ng/mL (82 nmol/L) and that this level of serum vitamin D is associated with reduced risk for a number of other cancers, including breast, lung, ovarian, prostate, and non-Hodgkin’s lymphoma. There is further evidence that vitamin D reduces the risk of autoimmune diseases, including multiple sclerosis (MS), a disease of the central nervous that is more prevalent in regions farther from the equator, and type 1 diabetes mellitus (see Chapter 8). Olympic skiers have noted a high rate of MS in their sport. Exposure to sunlight during early life or vitamin D supplementation has been related to reduced incidence of this condition. There also appears to be benefit for the primary forms of arthritis, type 2 diabetes mellitus, hypertension, and stroke (Grant, 2006). Vitamin D deficiency leads to secondary hyperparathyroidism, increased bone turnover, bone loss, and when severe, osteomalacia (softening of the bones). Hypovitaminosis D (a condition of low vitamin D status) is associated with impaired neuromuscular function. All persons with persistent, nonspecific musculoskeletal pain are at high risk for severe hypovitaminosis D (the condition of vitamin D deficiency). Hypovitaminosis D is prevalent even in southern latitudes and should be taken into account in the evaluation of postmenopausal and male osteoporosis (Levis and colleagues, 2005). Persons with renal (kidney) disease usually require supplementation because of impairment of the final steps of vitamin D synthesis (see Chapter 9). There is an increased risk of vitamin D deficiency in conditions of malabsorption of fat, such as with cystic fibrosis. In one study of this condition, despite a mean intake of 800 IU daily, optimal goals of 25(OH)D were not met (Rovner and colleagues, 2007). Prevalence of vitamin D deficiency in persons treated with medication for epilepsy has been found, especially with use of multiple medications, with indicators of adverse impact on bone health. Routine monitoring of serum 25(OH)D and vitamin D supplementation should be considered for individuals with epilepsy treated with medication (Nettekoven and colleagues, 2008). Vitamin E, also known as tocopherol, was initially recognized as essential for reproduction in rats. Vitamin E is transported in triglyceride (TG)-rich lipoproteins (see Chapter 7). One case of type 2 diabetes was found with both high levels of triglycerides and vitamin E (Girona and colleagues, 2008). Vitamin E acts as an antioxidant (preventing cell damage from oxidation). In relatively recent years, vitamin E was routinely advised at the 400 IU level in medical practices for the goal of reduced cardiovascular disease related to the oxidative damage. However, no evidence was found for this expected protection, and instead there was evidence of increased incidence of disease and mortality. Consequently, vitamin E supplementation is no longer routinely advised. However, a genetic subgroup of persons with diabetes were found to benefit with 400 IU vitamin E supplementation significantly reducing cardiovascular events (Milman and colleagues, 2008). Vitamin E is still important for overall health, when it comes from food sources in particular. Nuts and vegetable oils are rich in vitamin E and are protective against heart disease (see Chapter 7). A mere Maternal intake of vitamin E during pregnancy is beneficial for growth and development of the fetus. One study found that infants whose mothers had low plasma alpha-tocopherol concentrations weighed less and had smaller head circumference. Higher levels of both maternal alpha-tocopherol and cord retinol concentrations were associated with improved growth (Masters and colleagues, 2007). There is some evidence that asthma among children may be also related to maternal diet during pregnancy due to inadequate vitamin E intake (Seaton, 2008). One form of vitamin E, gamma-tocopherol, has been shown to be more effective than alpha-tocopherol in reducing systemic inflammation. In a rat study large doses of the gamma form was found to inhibit inflammatory pathways that are related to allergic rhinitis and asthma (Wagner and colleagues, 2008). However, in another rat study large doses of vitamin E were associated with changes in the small intestine and inflammation (Gianello and colleagues, 2007). Thus too little or excess intake of vitamin E appears to be related to inflammation. Vitamin K is also known as phylloquinone. Recommendations for dietary vitamin K intake have been made on the basis of blood coagulation factors. Vitamin K was first recognized as an antihemorrhagic factor. Because vitamin K is essential for the formation of prothrombin (a clotting factor), defective blood coagulation is the main symptom of vitamin K deficiency. Vitamin K is also involved in other physiologic processes, including vascular function and bone metabolism. There are three forms of dietary vitamin K, known as K1, K2, and K3. Vitamin K is found in dietary sources such as dark green, leafy vegetables (see Table 3-1), and it is also synthesized by bacteria in the jejunum and ileum of the small intestine (see Chapter 4). Vitamin K has a key function in the synthesis of at least two proteins involved in calcium and bone metabolism. Good vitamin K status has been found to increase bone mass in healthy peripubertal children (van Summeren and colleagues, 2008). The B vitamins are water-soluble vitamins required as coenzymes for enzymes essential for cell function. They have an essential role in maintaining function of the mitochondria (the furnaces of the cell); mitochondria are compromised by a deficiency of any B vitamin (Depeint and colleagues, 2006). Water-soluble vitamins are required in the diet because they cannot be synthesized by humans. The vitamin B complex refers to all water-soluble vitamins except ascorbic acid, also known as vitamin C (Table 3-2). Thiamin, or vitamin B1, is a water-soluble B complex vitamin that was first discovered in 1910 in the process of exploring how rice bran cured patients of beriberi (a condition involving inflammation of the nerves). Beriberi is classified as “dry” (neurologic) or “wet” (cardiovascular) and may include both forms in the same person. Table 3-2 100% DRI: 100% DRI: Angular stomatitis and cheilosis
The Micronutrients of Balanced Meals
Vitamins, Minerals, and Phytochemicals
INTRODUCTION
WHAT ARE THE DIETARY REFERENCE INTAKES?
HOW ARE VITAMINS AND MINERALS BEST INCLUDED IN THE DIET?
 cups, and a minimum of 3 cups of milk daily; MyPyramid has been altered to better portray these guidelines for food choices.
cups, and a minimum of 3 cups of milk daily; MyPyramid has been altered to better portray these guidelines for food choices.
WHAT IS THE ROLE OF VITAMINS IN NUTRITION?
WHAT IS THE DIFFERENCE BETWEEN FAT-SOLUBLE AND WATER-SOLUBLE VITAMINS?
FAT-SOLUBLE VITAMINS
Vitamin A
FUNCTIONS
GOOD SOURCES
SYMPTOMS OF DEFICIENCY
SYMPTOMS OF TOXICITY
Vitamin A (Nomenclature: Preformed—Retinol, Retinal, Retinoic Acid; Precursor—Carotene)
100% DRI:
Carotene:
100% DRI:
25% DRI:
Vitamin D (Nomenclature: Ergocalciferol [Vitamin D2], Cholecalciferol [Vitamin D3]; Precursors—Ergosterol [Plants], 7-Dehydrocholesterol [in Skin])
25% DRI:
Vitamin E (Nomenclature: Tocopherol)
25% DRI:
Vitamin K (Nomenclature: Menadione [Vitamin K3], Phylloquinone [Vitamin K1])
25% DRI:
No toxicity known
Vitamin D
Vitamin E
 cup of almonds provides 100% of the RDA for vitamin E.
cup of almonds provides 100% of the RDA for vitamin E.
Vitamin K
WATER-SOLUBLE VITAMINS
FUNCTIONS
GOOD SOURCES
SYMPTOMS OF DEFICIENCY
SYMPTOMS OF TOXICITY
Vitamin B1 (Nomenclature: Thiamin)
25% DRI
Rare with IV thiamin
Vitamin B2 (Nomenclature: Riboflavin)
25% DRI:
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 tsp cod-liver oil
tsp cod-liver oil average sweet potato
average sweet potato c carrots
c carrots c canned pumpkin
c canned pumpkin c spinach
c spinach c collards/kale
c collards/kale papaya
papaya c romaine lettuce
c romaine lettuce c broccoli
c broccoli c watermelon
c watermelon oz herring
oz herring oz shrimp
oz shrimp c sunflower seeds
c sunflower seeds c kale
c kale c spinach
c spinach c mustard greens
c mustard greens c broccoli
c broccoli c cabbage
c cabbage c blueberries
c blueberries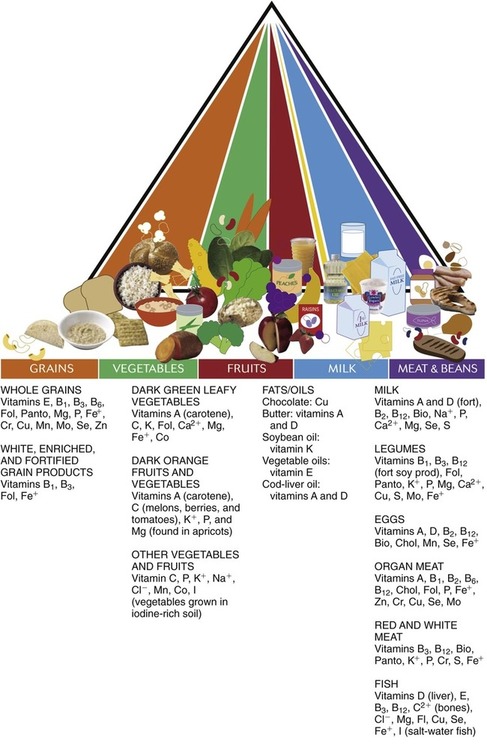


 c rice (enriched)
c rice (enriched) c wheat germ
c wheat germ c black-eyed peas/black beans
c black-eyed peas/black beans slices whole-grain bread
slices whole-grain bread c soybeans
c soybeans