The Lymphomas
Joachim Yahalom
Introduction
Lymphomas are malignant neoplasms arising in the lymphatic system, most commonly in lymph nodes. Yet, lymphomas may appear in any organ of the body where lymphocytes are present or may travel into. Lymphomas that arise outside the lymph nodes are called extranodal lymphomas. We recognize two main groups of lymphomas: The Hodgkin’s lymphomas (HL) and the non-Hodgkin’s lymphomas (NHL). The HL includes two categories: lymphocyte-predominant Hodgkin’s lymphomas (LPHL) and classical HL. The NHL is a more heterogeneous group that includes many entities with different characteristics and prognosis. This chapter will address general principles of radiation treatment of NHL, rather than each individual lymphoma or organ-specific involvement. The standard approaches for management of HL and NHL are outlined in the annually updated guidelines of the U.S. National Comprehensive Cancer Network (NCCN) (1,2).
In general, the lymphomas are among the most radiosensitive malignancies, and indeed, ionizing radiation is a highly effective modality for the treatment of both HL and NHL. The dramatic effects of radiation alone in reducing large lesions and even eliminating HL lesions were reported more than 100 years ago, soon after the discovery of x-rays by Wilhelm Conard Roentgen. Yet, during the first half of the twentieth century, due to technical constraints and/or poor methods of delivering radiation, all lymphomas remained incurable; radiation was used mostly for palliation and responses were brief. As x-ray technology improved in the 1940s and the concept of irradiating beyond the involved area was adopted, patients with early stage HL and NHL could be cured with radiation alone—the only effective curative modality that was available for lymphomas until the late 1960s.
Before the advent of effective chemotherapy, attempts were made to cure even advanced HL and NHL by maximizing the use of radiation alone. Optimizing the selection of patients and tailoring the radiation fields were associated with aggressive staging efforts that included using staging laparotomy and splenectomy for HL and even NHL. Moreover, the dependency on radiotherapy (RT) as the primary modality required wide extension of the radiation field as well as raising the dose to normal tissue tolerance levels. Although this mega-RT led to the cure of many patients, it was also associated with late development of complications and increased the mortality of cured patients beyond what was expected of the normal population. This was the price of successfully pioneering radiation therapy as a curative modality before the availability of effective chemotherapy.
The emergence of more effective and less toxic chemotherapy over the last three decades led to considerable changes in the use of RT in the management of lymphomas. First, in several types of NHL and in classical HL, chemotherapy has become the primary modality with RT used for consolidation and reduction of the risk of relapse. Yet, in some lymphomas, mostly in early stage low-grade lymphomas where chemotherapy is less effective, radiation alone remained the primary standard of care.
Radiation alone is currently the treatment of choice for early stage follicular lymphoma, mucosa-associated lymphoid tissue (MALT) lymphoma, and LPHL. The role of RT in consolidation following chemotherapy is well established in early stage “classic” HL, whereas in advanced-stage HL following programs of brief chemotherapy or following incomplete response. RT also plays an important role in high-dose therapy programs for salvage of HL and NHL. In early stage “aggressive” NHL, consolidation with RT is also the standard of care.
RT is also an excellent palliative modality that provides long-term local control and clinical benefit even for lymphomas in advanced stage such as mantle cell lymphoma (MCL), small lymphocytic lymphoma, advanced-stage MALT lymphoma, and follicular lymphoma. These specific types of lymphoma are highly sensitive to radiation and very low doses may be adequate for local control. The indications for using RT for treating lymphomas are summarized in Table 27.1.
Basics of Staging and Prognostic Groups
The staging system (3) for both HL and NHL is detailed in Table 27.2. The assignment of stage is based on the following:
The number of involved sites
Whether lymph nodes are involved on both sides of the diaphragm and whether this involvement is bulky (particularly in the mediastinum)
Table 27.1 Indications for Radiotherapy in the Treatment of Lymphomas
Radiation alone—potentially curative
- Hodgkin’s lymphoma—lymphocyte predominance
Stage I–II
- Hodgkin’s lymphoma—classicala
Stage IA–IIA (nonbulky)
- Follicular lymphoma
Stage I–II
Stage III (rarely used)
- Extranodal marginal zone (MALT) lymphoma
Stage IE–IIE
- Nodal marginal zone lymphoma
Stage I–II
- Mycosis fungoides
Stage IA, IB, IIA
- Anaplastic large cell lymphoma of skin
Stage IE
- Hodgkin’s lymphoma—classical
Stage I–II (favorable and unfavorable)
- Hodgkin’s lymphoma
Advanced stageb
- Diffuse large B cell lymphoma
Stage I–II
- Primary mediastinal lymphoma
Stage I–II
- Peripheral T cell lymphoma
Stage I–II
- Extranodal natural killer/ T cell lymphoma–nasal type
- Primary central nervous system lymphoma
- In high-dose therapy programs for Hodgkin’s lymphoma, diffuse large B cell lymphoma, follicular lymphoma, and mantle cell lymphoma
- Follicular lymphoma
- Mantle cell lymphoma
- Small lymphocytic lymphoma/chronic lymphocytic leukemia
- Marginal zone lymphoma
- Mycosis fungoides
- Diffuse large cell lymphoma
aCombined modality is treatment of choice.
bFor bulky sites, incomplete response, and as part of brief chemotherapy program (e.g., Stanford V).
MALT, mucosa associated lymphoid tissue.
- Hodgkin’s lymphoma—lymphocyte predominance
Whether there is contiguous extranodal involvement (E sites) or disseminated extranodal disease
Whether typical systemic symptoms (B symptoms) are present
In defining the stage of the disease, it is important to note how the information was obtained, because this fact reflects on the remaining uncertainties in the evaluation of the extent of disease. Clinical staging refers to information that has been obtained by initial biopsy, history, physical examination, and laboratory and radiographic studies only. A pathologic stage is determined by more extensive surgical assessment of potentially involved sites, for example, by surgical staging laparotomy and splenectomy.
Table 27.2 The Cotswald’s Modification of the Ann Arbor Staging for Hodgkin’s Lymphomas and Non-Hodgkin’s Lymphomas | |
|---|---|
|
Prognostic Factors for Early Stage Hodgkin’s Lymphomas
In practice, most experts categorize HL as either early stage (stages I–II) or advanced stage (stages III–IV). In the early stage category, it is important to distinguish between favorable early stage and unfavorable early stage. To be considered as unfavorable early stage, one or more of the following should be present: B symptoms, bulky disease, or involvement of more than three sites.
Indications for Radiotherapy
Hodgkin’s Lymphoma
It is important to distinguish between the two well-defined entities of HL, classical HL, and the less common nodular LPHL. The radiation approach to each entity is different. Most patients with LPHL are potentially curable with radiation alone, whereas combined-modality therapy is the standard approach for most patients with classical HL.
Lymphocyte-Predominant Hodgkin’s Lymphoma
Most (>75%) patients with LPHL present at an early stage; the disease is commonly limited to one peripheral site (neck, axilla, or groin) and involvement of the mediastinum is extremely rare. The treatment recommendations for LPHL differ markedly from those for classic HL. Involved or regional field radiation alone is the standard treatment for all early stage LPHL. It should be emphasized that even if regional radiation fields are selected, the uninvolved mediastinum should not be irradiated, thereby avoiding the site most prone for radiation-related short- and long-term side effects. Although there has not been a study that compared extended-field RT (commonly used in the past) with involved-field radiotherapy (IFRT), retrospective data suggest that IFRT is adequate (4). The radiation dose recommended is between 30 and 36 Gy with an optional additional boost of 4 Gy to a (rare) bulky site. In most cases, chemotherapy is not indicated.
Classical Hodgkin’s Lymphoma
Early Stage (Favorable and Unfavorable). Over the last two decades, the treatment of early stage classical HL has drastically changed. Combined-modality therapy consisting of short-course chemotherapy (most often doxorubicin [Adriamycin], bleomycin, vinblastine, dacarbazine [ABVD]) consolidated by reduced-dose radiation carefully directed only to the involved lymph node(s) site successfully replaced radiation alone as the treatment of choice (1,5). Although no longer the primary treatment, RT limited to smaller volumes, administered to a reduced dose with improved targeting, which is achieved with new imaging technology and supported by modern delivery systems, remains an important component of effective treatment programs for HL.
In the early 1960s, the implementation of a new concept—irradiating all involved and uninvolved lymph nodes—was termed radical RT (6). Radical RT soon cured an increasing number of patients with HL, a disease that
was then considered incurable. Radiotherapists used the newly available linear accelerators to treat enormous fields termed total lymphoid irradiation (TLI). TLI spared little other than brain, limbs, and some of the lungs, liver, and kidneys. Bulky sites were covered with large radiation field margins, and occasionally, even the lungs and the liver were intentionally irradiated. Mechlorethamine, vincristine (Oncovin), procarbazine, and prednisone (MOPP) chemotherapy was used for consolidation or salvage. The giant radiation field size compensated for lack of good imaging information. The dose was also maximized (the standard dose at Stanford was 44 Gy), and often treatment was given in a technique that delivered even higher doses anteriorly, to the heart and breast.
was then considered incurable. Radiotherapists used the newly available linear accelerators to treat enormous fields termed total lymphoid irradiation (TLI). TLI spared little other than brain, limbs, and some of the lungs, liver, and kidneys. Bulky sites were covered with large radiation field margins, and occasionally, even the lungs and the liver were intentionally irradiated. Mechlorethamine, vincristine (Oncovin), procarbazine, and prednisone (MOPP) chemotherapy was used for consolidation or salvage. The giant radiation field size compensated for lack of good imaging information. The dose was also maximized (the standard dose at Stanford was 44 Gy), and often treatment was given in a technique that delivered even higher doses anteriorly, to the heart and breast.
Although the above approaches are not used anymore, it should be appreciated that, thanks to those pioneering efforts, tens of thousands of young patients who were treated during the 1960s, 1970s, and 1980s survive today, free of HL. Indeed, some succumbed to the early and to the then unknown, late treatment-related toxicities, such as leukemia and lung cancer related to MOPP and other chemotherapy regimens (7), or developed breast, lung, other solid tumors, and coronary heart disease related to radiation.
Through a series of randomized trials, the following treatment principles have been established: ABVD is better than MOPP and is less toxic (8); combined modality is more effective and less toxic than radical radiation alone (9); when combined with chemotherapy, the radiation field could be minimized to include only the involved site (IFRT) (10) and the radiation dose can be reduced from over 40 to 30 Gy and possibly even lower (11), and only four cycles of ABVD are sufficient in early stage (and probably only two cycles in favorable disease) when used with mini-RT (12).
The conversion from large multisite radiation fields to a smaller and better-defined radiation field also allowed for accurate conformal radiation therapy. The large fields of the past limited the radiation technique to two simple opposed anterior and posterior fields. The conversion to smaller and better-defined radiation volumes allowed the utilization of more conformal radiation therapy, based on better imaging, computerized planning programs, and when indicated, advanced tools such as intensity-modulated radiotherapy (IMRT). Modern breakthroughs in RT technology can now be implemented in HL to increase accuracy even further, avoid normal organs irradiation, and thereby improve the therapeutic ratio.
Advanced-Stage Hodgkin’s Lymphoma. The role of consolidation RT after induction chemotherapy depends on several factors: The response to chemotherapy (complete, uncertain, or partial), the presence of bulky disease before chemotherapy, and the type and length of the chemotherapy program. Patients who had no bulky disease, have received the full course of chemotherapy (e.g., ABVD X 6–8), and obtained an unquestionable complete response (CR) are unlikely to benefit from additional RT (13). IFRT should be added in patients with advanced-stage HL who present with bulky disease or to patients who remain in an uncertain or incomplete remission after chemotherapy. When advanced-stage HL is treated with the new highly effective and less toxic treatment program of Stanford V, it is imperative to follow the brief chemotherapy program with IFRT to sites originally >5 cm or to a clinically involved spleen. When RT was fully or partially omitted on this program, the results were inferior (14).
Salvage Programs for Refractory and Relapsed Hodgkin’s Lymphoma. High-dose therapy supported by autologous stem cell transplantation (ASCT) has become a standard salvage treatment for patients who relapsed or remained refractory to chemotherapy or to combined-modality therapy. Many of the patients who enter these programs have not received prior RT or had a relapse at sites outside the original radiation field. These patients could benefit from integrating RT into the salvage regimen.
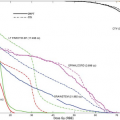
At Memorial Sloan-Kettering Cancer Center (MSKCC), a program that integrated RT into the high-dose regimen for salvage of Hodgkin’s disease (HD) was developed almost 20 years ago, and modified every several years. Accelerated hyperfractionated irradiation (b.i.d. fractions of 1.8 Gy each) is scheduled to start after the completion of reinduction chemotherapy and stem cell collection and before the high-dose chemotherapy and stem cell transplantation. Patients who had not been previously irradiated received IFRT (18 Gy in 5 days) to sites of initially bulky (>5 cm) disease and/or residual clinical abnormalities followed by TLI of 18 Gy (1.8 Gy per fraction, b.i.d.) within an additional 5 days. Patients who had prior RT, received only IFRT (when feasible) to a maximal dose of 36 Gy. This treatment strategy has been in place since 1985, with over 350 patients treated so far. The program has been very effective in salvaging both relapsed and chemotherapy-refractory patients, has a low toxic profile with no mortality for the last 10 years, and compares favorably with programs that do not use RT as critical part of the regimen (15,16).
Non-Hodgkin’s Lymphoma Entities That Are Commonly Treated with Radiotherapy
Follicular Lymphoma
Approximately 20% of patients with low-grade follicular lymphomas present in localized stages (I–II). The standard treatment for these patients is regional RT or IFRT. The reports of patients with stage I and II low-grade follicular lymphoma from Stanford with long-term follow-up indicated that a substantial number of patients in this category have, indeed, been “cured” by RT (17). The median follow-up was 7.7 years and observation has been maintained for up to 31 years. The median survival after RT was 14 years. The actuarial survival rates at 5, 10, 15, and 20 years were 82%, 64%, 44%, and 35%, respectively. Freedom from
relapse (FFR) at 5, 10, 15, and 20 years was 55%, 44%, 40%, and 37%, respectively. Only 5 of 47 patients who reached 10 years without a relapse developed a late recurrence. There was no significant FFR difference between stages I and II or between nodal or extranodal disease. The survival of patients irradiated after the age of 60 was significantly shorter than the survival of younger patients, but the decrease of survival in this age group was strongly affected by death from other causes.
relapse (FFR) at 5, 10, 15, and 20 years was 55%, 44%, 40%, and 37%, respectively. Only 5 of 47 patients who reached 10 years without a relapse developed a late recurrence. There was no significant FFR difference between stages I and II or between nodal or extranodal disease. The survival of patients irradiated after the age of 60 was significantly shorter than the survival of younger patients, but the decrease of survival in this age group was strongly affected by death from other causes.
Most relapses in early stage patients occur in unirradiated sites during the first 5 to 6 years following therapy (18). In the Stanford series, administration of RT to nodal sites on both sides of the diaphragm was associated with a significantly better FFR compared with more localized treatment but did not translate into a clear survival benefit (17). A similar experience was reported from M.D. Anderson (19). In the absence of a clear survival benefit for TLI in this setting, the common involvement of mesenteric nodes that may require whole abdominal irradiation, and considering the fact that almost half of the patients will eventually require chemotherapy for relapse, involved or regional field irradiation is currently employed for these patients.
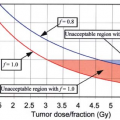
The optimal radiation dose for indolent lymphoma has not been determined in a prospective study. However, most current RT series for stages I and II indolent lymphomas usually employ 30 to 40 Gy, and in-field recurrences have been uncommon. Data from the Princess Margaret Hospital showed in-field disease control in 78% of patients treated with doses of <25 Gy and 91% control with doses >25 Gy (20). At M.D. Anderson, excellent local control was achieved with 30 Gy to lesions <3 cm (19). Fuks correlated the relapse rate in regional areas of follicular lymphoma with the radiation dose delivered to these sites and showed 63% relapse in areas receiving <27.5 Gy, 27% relapse with a dose range of 30 to 35 Gy, 12% and 6% relapse rate for 40 and 44 Gy, respectively (21). A dose of 30 to 36 Gy (in 1.8 Gy daily fractions) to involved sites (40 Gy, if bulky) and 24 to 36 Gy to uninvolved adjacent sites is currently recommended.
Extranodal Marginal Zone Lymphoma of Mucosa-Associated Lymphoid Tissue
The most common organ involved with MALT lymphoma is the stomach. Gastric MALT lymphoma (GML) is often associated with the presence of Helicobacter pylori in the stomach and the antibiotic eradication of this pathogen leads to regression of GML in many patients. Yet, approximately 30% to 50% of patients with H. pylori-positive GML will show persistent or progressing lymphoma even after eradication of H. pylori with antibiotic therapy and even in complete responders, almost 15% will relapse within 3 years, suggesting that about half of the patients with GML will eventually be considered for additional therapies (22). Most of those will still have disease limited to the stomach. In these patients and in those that present with no evidence of H. pylori infection IFRT with relatively low radiation dose is the treatment of choice (2).
Several institutions reported excellent results using IFRT of the stomach in H. pylori-independent GML patients who either failed antibiotic therapy or had no evidence of H. pylori infection (23,24,25,26). The recent update of the MSKCC experience included 51 patients with GML (stage I-39; stage II-10; stage IV-2) who were either H. pylori-negative (30 patients) or remained with persistent lymphoma after antibiotic therapies and adequate observation (21 patients) (27). All patients were treated with radiation to the stomach and perigastric nodes; the median total dose was 30 Gy in 4 weeks. All patients had regular follow-up endoscopic evaluations and biopsies. Forty-nine of fifty-one (96%) patients obtained a biopsy-proven CR. Of the three patients who relapsed, two were salvaged. Three patients died of other malignancies; all second tumors developed outside the radiation field. At a median follow-up of 4 years, freedom from treatment failure, overall survival (OS), and cause-specific survival were 89%, 83%, and 100%, respectively. Treatment was well tolerated, with no significant acute or chronic side effects. The experience from Toronto and Boston, using the same radiation approach, was equally successful (28,29,30) supporting the approach that modest dose IFRT is the treatment of choice for patients with persistent GML who have exhausted the antibiotic therapy approach or are unlikely to respond to it (H. pylori-negative patients) (31,32). The techniques for treatment of gastric lymphoma have been recently published (33).
MALT lymphomas (ML) have also been described in various nongastric sites, such as salivary glands, skin, orbit, conjunctiva, lung, thyroid, larynx, breast, kidney, liver, bladder, prostate, urethra, small intestine, rectum, pancreas, and even in the intracranial dura (32).
The optimal management of non-GMLs has not yet been clearly established. Retrospective series included patients treated with surgery, RT, and chemotherapy, alone or in combination. Marginal zone lymphomas are exquisitely sensitive to relatively low doses of radiation. Specifically, ML in sites such as salivary glands, ocular, conjunctiva, thyroid, breast, and bladder have been successfully eradicated with IFRT encompassing the involved organ alone with a dose of 24 to 36 Gy (28,30). Even unusual sites (such as larynx, base of skull, urethra, and prostate) not easily amenable to surgery have been well controlled by IFRT.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree