The incidence of the myelodysplastic syndromes (MDS) in the United States is reported as 3.4 per 100,000 people, translating to over 10,000 new diagnoses annually. This figure is considered to be an underestimate as our data capture techniques improve, and probably translates to a prevalence of approximately 60,000 people or more living with the disease. Patients are in their seventh or eighth decades at diagnosis, typically present with cytopenias, and have substantive transfusion requirements. The most common risk factors for developing MDS include advanced age, male gender, previous exposure to chemotherapy or radiation therapy, smoking, or, in rare cases, exposure to industrial chemicals.
Patients with a blood picture compatible with the myelodysplastic syndromes (MDS) were first described at the beginning of the 20th Century, whereas the first MDS case series was published approximately 35 years ago. This timing places the recognition of MDS and development of effective therapies a full 50 to100 years behind what has occurred for other hematologic malignancies. Similarly, the depth of understanding of MDS epidemiology lags behind that of other cancers.
Within the past decade three drugs, azacitidine, lenalidomide, and decitabine, have been approved by the US Food and Drug Administration (FDA) specifically for MDS. Other active therapies used off-label for treating MDS include hematopoietic growth factors used to treat cytopenias associated with MDS (particularly erythropoiesis stimulating agents [ESAs]) ; cytotoxic drugs, such as cytarabine and clofarabine; and those with immune modulating mechanisms of action, such as thalidomide and antithymocyte globulin. The availability of such therapies, along with their acknowledged differential activity in various MDS subtypes, has in part spurred the maturation rate of epidemiologic knowledge to quantify the societal impact of MDS and ascertain numbers of patients responsive to specific therapies and to identify risk factors for developing MDS.
This article reviews the most recent published incidence rates and characteristics of patients with MDS, and known risk factors for developing this collection of diseases.
Myelodysplastic syndromes: incidence and prevalence
In 2001 in the United States, the Surveillance, Epidemiology, and End Results (SEER) program of the National Cancer Institute and the Centers for Disease Control and Prevention started to track incidence rates of MDS, alongside other cancers. Based on these SEER data, collected from 2001 to 2003, the age-adjusted incidence rate of MDS in the United States was estimated to be 3.4 per 100,000 people, which translates to approximately 10,000 new cases per year. Over this 3-year period, the incidence rate increased from approximately 3.3 per 100,000 people in 2001 to 3.4 in 2002 and then to 3.6 in 2003, not from an epidemic of MDS over this time period but because cancer registries were still fine tuning their identification and classification of the disease. In 2004, the incidence rate was estimated at 3.8 per 100,000 people, cresting the rate of acute myeloid leukemia (AML) and potentially making MDS the most common type of leukemia, with new yearly diagnoses estimated to be close to 15,000 citizens in the United States. Rates were lowest for people younger than 40 years, at 0.14 per 100,000, and highest with increasing age, at 36 per 100,000 for patients 80 years and older. As these data derive from cancer registries, they do not include detailed patient information other than age at diagnosis, gender, race, French-American-British (FAB) classification at diagnosis, and survival. The incidence rate in the United States is similar to that reported in England/Wales and Sweden (3.6 per 100,000), Germany (4.1 per 100,000), and France (3.2 per 100,000), but higher than is seen in Japan (1.0 per 100,000).
Defining prevalence rates (numbers of people living with MDS, as opposed to new diagnoses) has been elusive. Preliminary data from Germany reveals a prevalence rate of 20.7 per 100,000 people. If we assume that incidence, and thus prevalence rates, between the United States and Germany are similar, this would translate to approximately 60,000 people living with MDS in the United States. However, even this is thought to be a gross underestimate because of failure to diagnose the disease.
In a study by Guralnik and colleagues in 2004, the prevalence of anemia in the United States was estimated from 2000 blood samples collected from people 65 years of age or older as part of the third National Health and Nutrition Examination Survey. The overall prevalence was 10.6%, divided approximately equally into three categories: people with nutrient-deficiency anemia (ie, anemia associated with vitamin or iron deficiency); people with anemia of chronic inflammation with or without renal insufficiency; and unexplained anemia. Within this last category, 17% of people had macrocytic anemia, leucopenia, or thrombocytopenia (ie, peripheral blood findings typical of MDS). This percentage would in turn translate to a prevalence of 170,000 people. Complicating the matter further, these data were derived from an era before the approval of MDS therapies by the FDA. As at least one of these therapies (azacitidine) has prospectively demonstrated a survival advantage in higher-risk patients with MDS, prevalence rates can be expected to increase because of case finding. Thus, although a prevalence rate of 170,000 people with MDS can be assumed to be an overestimate, a rate of 60,000 people is almost assuredly underestimating the impact of the disease.
Myelodysplastic syndromes characteristics
What is the clinical picture of MDS in the United States? This question can be answered from data derived from SEER and the North American Association of Cancer Registries (NAACR), and from a recent study characterizing patients with MDS that was based on over 4500 surveys completed by 101 physicians.
The SEER/NAACR study is based on data from 24,798 subjects over the years 2001 to 2003 and encompassing approximately 82% of the population in the United States. In addition to age-dependent incidence rates discussed earlier, men have higher age-adjusted rates per 100,000 people than women (4.4 vs 2.5), as do whites compared with blacks (3.3 vs 2.4), though one study that uses Veterans Administration data belies this latter difference. The 3-year relative survival rates for all participants is 45%.
In the survey study of 4514 subjects, 670 were newly diagnosed, of whom 38% were women, whereas the remainder were established patients. The median age at diagnosis was 71 years and among established patients was 72 to 75 years. Secondary MDS was seen in approximately 10% of all subjects, most following chemotherapy (76%).
Among recently diagnosed subjects with MDS, the majority had some degree of pancytopenia: the median hemoglobin value was 9.1 g/dL (interquartile range 8–10 g/dL); the median platelet count was 100,000/mm 3 (interquartile range 56,000–150,500/mm 3 ); and the median absolute neutrophil count was 1780/mm 3 (interquartile range 1070–2800/mm 3 ). A minority of subjects had circulating blasts: a mean of 16% had 1% to 5% blasts, whereas a mean of 10% had more than 5% blasts.
Lower-risk MDS (FAB categories of refractory anemia [RA] and RA with ring sideroblasts [RARS]; World Health Organization [WHO] categories of RA, RARS, refractory cytopenia with multilineage dysplasia, refractory cytopenia with multilineage dysplasia and ring sideroblasts, MDS with deletion of chromosome 5q [del (5q)], and MDS unclassified; and International/Prognostic Scoring System (IPSS) scores of low and intermediate-1) was more common in established than in recently diagnosed cases, comprising 60% to 69% of established versus 50% of recently diagnosed subjects with MDS using FAB criteria; 56% to 66% versus 51%, respectively, using WHO criteria; and 75% to 79% versus 64%, respectively, using IPSS criteria.
Among lower-risk, newly diagnosed subjects with MDS, 22% were dependent on red blood cell transfusions, whereas 57% had ever received a red blood cell transfusion. Only 5.5% were dependent on platelet transfusions, whereas 37% had ever received a platelet transfusion. Corresponding percentages were much higher in higher-risk subjects. Among those newly diagnosed, 68% were dependent on red blood cell transfusions, whereas 88% had ever received a transfusion; and 33% were dependent on platelet transfusions, whereas 58% had ever received such a transfusion. Regardless of timing of diagnosis, or severity of MDS, ESAs were used by more than 50% of this MDS population. The only potentially curative therapy for MDS, bone marrow transplantation, had been performed or was even being considered in less than 5% of all subjects, even in the era of reduced intensity transplantation.
Myelodysplastic syndromes characteristics
What is the clinical picture of MDS in the United States? This question can be answered from data derived from SEER and the North American Association of Cancer Registries (NAACR), and from a recent study characterizing patients with MDS that was based on over 4500 surveys completed by 101 physicians.
The SEER/NAACR study is based on data from 24,798 subjects over the years 2001 to 2003 and encompassing approximately 82% of the population in the United States. In addition to age-dependent incidence rates discussed earlier, men have higher age-adjusted rates per 100,000 people than women (4.4 vs 2.5), as do whites compared with blacks (3.3 vs 2.4), though one study that uses Veterans Administration data belies this latter difference. The 3-year relative survival rates for all participants is 45%.
In the survey study of 4514 subjects, 670 were newly diagnosed, of whom 38% were women, whereas the remainder were established patients. The median age at diagnosis was 71 years and among established patients was 72 to 75 years. Secondary MDS was seen in approximately 10% of all subjects, most following chemotherapy (76%).
Among recently diagnosed subjects with MDS, the majority had some degree of pancytopenia: the median hemoglobin value was 9.1 g/dL (interquartile range 8–10 g/dL); the median platelet count was 100,000/mm 3 (interquartile range 56,000–150,500/mm 3 ); and the median absolute neutrophil count was 1780/mm 3 (interquartile range 1070–2800/mm 3 ). A minority of subjects had circulating blasts: a mean of 16% had 1% to 5% blasts, whereas a mean of 10% had more than 5% blasts.
Lower-risk MDS (FAB categories of refractory anemia [RA] and RA with ring sideroblasts [RARS]; World Health Organization [WHO] categories of RA, RARS, refractory cytopenia with multilineage dysplasia, refractory cytopenia with multilineage dysplasia and ring sideroblasts, MDS with deletion of chromosome 5q [del (5q)], and MDS unclassified; and International/Prognostic Scoring System (IPSS) scores of low and intermediate-1) was more common in established than in recently diagnosed cases, comprising 60% to 69% of established versus 50% of recently diagnosed subjects with MDS using FAB criteria; 56% to 66% versus 51%, respectively, using WHO criteria; and 75% to 79% versus 64%, respectively, using IPSS criteria.
Among lower-risk, newly diagnosed subjects with MDS, 22% were dependent on red blood cell transfusions, whereas 57% had ever received a red blood cell transfusion. Only 5.5% were dependent on platelet transfusions, whereas 37% had ever received a platelet transfusion. Corresponding percentages were much higher in higher-risk subjects. Among those newly diagnosed, 68% were dependent on red blood cell transfusions, whereas 88% had ever received a transfusion; and 33% were dependent on platelet transfusions, whereas 58% had ever received such a transfusion. Regardless of timing of diagnosis, or severity of MDS, ESAs were used by more than 50% of this MDS population. The only potentially curative therapy for MDS, bone marrow transplantation, had been performed or was even being considered in less than 5% of all subjects, even in the era of reduced intensity transplantation.
Risk factors for developing myelodysplastic syndromes
As discussed in the first section of this article, the single greatest risk factor for developing MDS is advancing age, with yearly incidence rates increasing tenfold for octogenarians compared with the rest of the population.
The majority of secondary MDS cases arise following chemotherapy for other cancers, particularly alkylating agents or topoisomerase inhibitors, and following radiation therapy. The typical latency period for secondary MDS after exposure to alkylating agents or radiation therapy is 5 to 10 years, and the risk appears to be dose dependent. These specific types of secondary MDS are characterized by unbalanced translocations involving chromosome 5 or chromosome 7, or complex cytogenetics. MDS following exposure to topoisomerase inhibitors is much less common, with a latency period of approximately 2 years. It is more often characterized by a balanced translocation often involving 11q23 (the mixed lineage leukemia gene); long-term prognosis is poor for either type of secondary MDS.
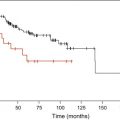
For example, two recent studies have explored the rates of secondary myeloid malignancies (MDS and AML) among patients with non-Hodgkin lymphoma who have undergone autologous bone marrow transplantation. In both series, subjects were heavily pretreated with alkylating agents and topoisomerase inhibitors, and received Cytoxan/total body irradiation or busulfan/Cytoxan preparative regimens for their transplantation. Rates of secondary MDS/AML approached 7% at 10 years, or 20% at 20 years of follow-up. MDS has also been reported at definable, lower rates following alkylating, topoisomerase-inhibitor, or radiation therapy for breast and other solid tumor cancers, and following exposure to purine analogs for lymphoid malignancies. Specific polymorphisms in the methylene tetrahydrofolate reductase gene (involved in DNA synthesis) may predict for a higher risk for secondary MDS/AML after treatment with cyclophosphamide, particularly in patients with breast cancer.
Other therapies examined for a subsequent risk for developing MDS include radioimmunotherapy (eg, with I 131 -tositumomab), which does not appear to have an association. The use of granulocyte colony-stimulating factor (G-CSF) in children may increase the incidence of secondary MDS and AML, which has also been reported as a possible complication following breast cancer therapy. MDS may also evolve from an antecedent hematologic disorder, particularly polycythemia vera after treatment with P 32 or busulfan.
Though several other risk factors have been proposed for de novo MDS development, few have been confirmed by epidemiologic studies. One of the more common established risk factors, in addition to age and male gender, is environmental and occupational exposure to organic solvents, such as benzene and its derivatives. The association of benzene exposure to MDS development may be greater in those with specific nicotinamide adenine dinucleotide phosphate (NADPH): quinine oxidoreductase (NQO1) polymorphisms. Case-control studies confirm an increasing risk for MDS in association with family history of hematopoietic cancer and exposure to agricultural chemicals (insecticides, pesticides, herbicides, or fertilizer); solvents; and radiation exposure. One such study in the United States found the odds ratios for an MDS association and environmental factors to be 4.55 for agricultural chemical exposure, 2.05 for solvent exposure, and 3.22 for smokers who were also exposed to agricultural chemicals or solvents. Other studies have linked the development of MDS to exposure to genotoxic industrial agents, including radiation, halogenated organics, metals, and petroleum products, in addition to pesticides and solvents.
A recent meta-analysis examined the association between smoking or alcohol intake and the development of MDS. Across 10 studies, composed of 2105 cases and 3363 controls, the odds ratio for MDS developing in smokers was 1.45 (95% CI 1.21, 1.74), indicating a 45% increase in risk. The association between alcohol intake and MDS was examined in five studies, composed of 745 cases and 1642 controls. The overall association was 1.31 (95% CI 0.79–2.18), indicating a possible increase in risk of 31%, though confidence intervals crossed parity.
MDS is not considered a familial or congenital disorder. This being said, rare cases of familial MDS and AML have been reported, mostly in association with loss of 5q and or 7q, or with familial platelet disorders in which there appears to be differential expression of genes involved in signal transduction. MDS has also been associated with a family history of hematologic cancers, with an odds ratio of 1.92. A rare G-CSF receptor polymorphism may also predispose to high-risk MDS, also through altered signal transduction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree