© Springer International Publishing Switzerland 2015
Joel Faintuch and Salomão Faintuch (eds.)Obesity and Diabetes10.1007/978-3-319-13126-9_11. The Dual Burden of Obesity and Diabetes: Old Problems Die Hard
(1)
Gastroenterology Department, University of Sao Paulo, Hospital das Clinicas, Sao Paulo, Brazil
(2)
Radiology Department, Harvard Medical School, Beth Israel Deaconess Medical Center, Boston, MA, USA
Abstract
The array of efforts to control obesity is as wide and diversified as the mechanisms of the disease. From jaw wiring to fecal transfer, there have been virtually no limits for surgical and medical ingenuity. Initial results are always encouraging, if not for other reasons, because some placebo effect is always operative. The patient wants to lose weight, trusts the doctor, and is psychologically motivated, which can be a winning association, at least for a while.
That’s why all the tenets of scientific investigation, including not only sound pathophysiological basis but also adequate controls and long-term follow-up, are indispensable. In the present chapter some creative and promising techniques will be reviewed, even though not all of them have been sufficiently tested in the bariatric population, or are ready for application.
1.1 Introduction
Obesity is the major nutritional challenge worldwide. Its companion is type 2 diabetes, the number one international endocrine and metabolic disease. Together they represent the diabesity epidemic, which is draining resources, overwhelming healthcare facilities, and impairing life expectancy and quality everywhere. Of course prevention is the best medicine, and lifestyle shifts are being recommended everywhere. Nevertheless ingrained sedentarism, deleterious dietary patterns, and unbound hedonism are not only troublesome to antagonize. They may require expensive, and legally challenging, remodeling of the very premises of modern consumer-based, car-moved, screen-gazing, and daylong-snacking civilization.
Overeating or preference for calorie-dense foods is not equaled to antisocial behavior, or susceptible to punishment. Indeed the obese population, particularly children, is to a large extent victim of the obesogenic environment, as sometimes discussed in lawsuits (Mello et al. 2003). Yet exclusively relying on the society to solve the epidemic may not be sufficient. Personal engagement and alertness, along with well-taught and drilled healthy habits, are of fundamental importance.
1.2 History of Obesity Treatment
Avicenna (980–1037), in the famous treatise Cannon of Medicine, already reports many of the features and complications of obesity such as shortness of breath, sudden death, stroke, infertility, and reduced libido. In more recent times Charles Dickens (1812–1870), in The Posthumous Papers of the Pickwick Club (London, 1836), writes about Fat Boy Joe, a puffy adolescent who is constantly hungry, is very red in the face, and is always falling asleep. William Osler, in 1918, anticipated on such basis the Pickwickian syndrome, encompassing obesity and somnolence.
Early publications notwithstanding, obesity has not always been considered a pathologic aberration, requiring prompt and effective management, except for extreme cases. During centuries, exuberant or deviant somatic proportions were perceived as a mere variant of normal. Anatomical compendia highlighted “habitus brevilineus,” in contrast to “habitus longilineus,” as morphological entities, not as illnesses.
Bariatric pioneers in the 1960s and 1970s faced difficulties with health plans and reimbursing agencies, as these tended to classify weight loss interventions as merely cosmetic, not as essential metabolic therapy, and refused to provide coverage. Scott, one of the introductors of the intestinal bypass, is credited with the coining of the expression “morbid obesity,” in order to differentiate conditions with major health implications and life-shortening hazards, from lesser accumulations of body fat (Scott et al. 1970).
Yet, multiple empirical classifications of severe obesity were employed by surgeons along the years, such as two or three times the ideal weight (Scott et al. 1970), 50 pounds above it, ponderal index, and Broca’s index (Organ et al. 1984), until modern BMI (body mass index) driven indications, and EWL (excess weight loss) postoperative monitoring routines, eventually crystallized.
1.3 Type 2 Diabetes Treatment
The association of diabetes with obesity, or diabesity, is not peacefully enshrined in medical texts either. Of course exaggerated body fat, primarily in the visceral compartment, triggers insulin resistance and glucose intolerance. Also, during diabetes onset, hyperinsulinemia may be prominent, exaggerating protein and lipid anabolism. Yet in early times overweight people were not so plentiful, lean diabetics predominating. Moreover, before long-acting insulin modalities (NPH) became available, and particularly before oral antidiabetics started to be manufactured, in the 1940s and 1950s, diabetic ketoacidosis in type 2 diabetes was frequent, rather than an exception during disease decompensations.
This is a phenomenon associated with anorexia, catabolism, and undernutrition. Indeed, classically diabetes featured polydipsia, polyphagia, polyuria, and weight loss, and many patients died with cachexia.
Pharmacological assistance for diabetes, nominally regular insulin, has been available for nearly one century; nevertheless prolonged remission or cure is still an elusive target for sedimented disease. In parallel, a diversified lifestyle and therapeutic arsenal can now be prescribed for obesity. Long-term results are sometimes comparable to bariatric intervention in moderate stages of the disease, including obesity-triggered diabetes when just prediabetes is present (Perreault et al. 2012).
Such progress notwithstanding, only surgery has consistently been followed by major weight loss in all categories of severe obesity, sustained for over two decades, along with significant remission rates of established type 2 diabetes. This additional bonus naturally gave rise to specific metabolic or antidiabetic operations.
1.4 Ongoing Controversies
After thousands of scientific studies and millions of bariatric interventions, the debate is not exhausted. There are voices suggesting that optimal multidisciplinary clinical management, or perhaps polytherapeutic prescription strategies, could still come close if not fully mimic surgery, for long-term amelioration or cure of obesity and diabetes (Scott et al. 1970; Organ et al. 1984; Perreault et al. 2012).
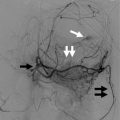
New possibilities aiming at manipulation of the hormonal milieu, beta-cell reserve, basal energy expenditure, satiety and appetite, and of course new drugs and therapeutic regimens might pave the way for more comprehensive nonsurgical protocols. Parasurgical approaches including endoscopic procedures, and even selective arterial embolization, are also the focus of interest.
1.5 Nonbariatric Nonmetabolic Gastrointestinal Operations
Of course basic pathophysiologic questions remain which have not been answered, or not even asked. What happens when gastrointestinal anatomy in diabetic patients is rearranged, in shapes somehow mimicking bariatric or metabolic interventions, however the patient is not obese and was operated for another reason, nominally cancer?
In the case of cancer gastrectomy the doubts have been around for some time. A few reports appeared in the literature, however, with widely divergent results, ranging from 90 % remission to virtually no advantage at all. In a prospective series including retrospective findings, with a control population and a very long follow-up period, we documented remission of diabetes however in somewhat lower proportions than after Roux-en-Y procedures for morbidly obese candidates. After 7–9 years, attenuation of diabetes occurred in 32.4 % of the nonobese patients submitted to cancer gastrectomy, contrasting with 68.6 % after Roux-en-Y bypass for morbid obesity (Hayashi et al. 2013).
Such disagreement was actually expected, because lean diabetics usually suffer from more adverse genetic backgrounds and more severe pancreatic exhaustion. The cancer population was older as well. Still, the investigation starkly demonstrated that it’s the reshaping of the gut architecture that improves glucose homeostasis, not necessarily weight loss.
And after colorectal resections? Here the conflict should be even more serious, because few if any roles in glucose homeostasis have been attributed to the distal gut. In the large bowel digestion is over, nutrient absorption is essentially nil, and few hormones are expressed. Yet moderate but significant amelioration of diabetes was recorded after cancer operations. As many as 42.4 % of the population exhibited improvement in the diabetic profile, compared to 7.1 and 7.7 % in two control groups (Faintuch et al. 2014). The hypothesis was linked to changes in gut microbioma, even though some hormonal changes are possible, and will require further studies.
1.6 Electrical Stimulation of the Gastrointestinal Tract and Vagus Nerve
Gastric and vagus nerve electrical stimulation have a long and scientifically rich, however somewhat convoluted history. Appetite regulation and obesity treatment are relatively recent goals, related aims being control of gastrointestinal physiology including gastric emptying. Retrograde modulation via vagi of certain brain centers, including the hypothalamic–pituitary–adrenal axis, as well as of selected psychiatric as well as immunoinflammatory phenomenons have been experimentally reported, and therapeutic indications in epilepsy and severe depression can be encountered.
Almost one century ago (McCrea and McSwiney 1926), the abdominal vagi were already experimentally submitted to faradic shocks, with changes in pyloric contractions. Along the subsequent decades, multiple mechanisms were hypothesized for the wide spectrum of visceral effects, and sometimes for the lack thereof, after different stimulation patterns.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree