The discovery of a new Rotavirus that caused adult epidemic diarrhea in China in 1980’s
Outline
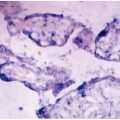
From the winter of 1982 to the spring of 1983, there was an outbreak of acute gastroenteritis, an epidemic caused mostly by water pollution occurred in the northwest, north, northeast, east, and south of China and southwest regions. This epidemic had a sudden onset and could not be effectively treated with antibiotics, but intravenous rehydration therapy could quickly improve the symptoms and shorten the recovery time with good prognosis and no sequelae or death. This epidemic spread quickly to a wide range of geographical areas in China with a high incidence rate, mainly involved in adults in factories and mines. Its symptoms resembled cholera, causing social panic and unrest. In the process of cause investigation, initial assumption and later confirmation, the epidemiologists working in the area of health and epidemic prevention had a rapidly increasing capacity of problem discovery and solving by carrying out a series of field epidemiological investigations. Through description of epidemiological and laboratory evidence, cholera was first excluded, and we affirmed that this epidemic diarrhea was caused by virus with an infection source of patients and carriers rather than the animals. The disease caused the outbreak through fecal contamination of the source water, and then spread through daily contact. Since adults were susceptible, this disease had an outbreak and epidemic with suitable communicable conditions. By using analytic methods, epidemiologists concluded that the cause of the disease was contaminated water. Epidemiological experiments showed that the disease spread through a fecal-oral route and could be terminated after changing water source. Finally, through individual studies and multicollaborative investigations, using modern experimental techniques such as electron microscopy, serological and RNA electrophoresis analysis, the investigators found that the cause was a new rotavirus, which was first reported to the public and then recognized worldwide. The virus was classified as Rotavirus B.
During the early 1980’s, the epidemic of acute adult gastroenteritis resembling cholera occurred in China with an initial impression of adult non-bacterial epidemic diarrhea. Health and epidemic prevention institutes in the epidemic district and epidemiologists had investigated the disease and achieved the same results. Now we take the epidemic in Lanzhou region from November 1982 to February 1983 as an example to demonstrate ideas and use of epidemiological methods by epidemiological workers during field epidemiological investigations, the persistent spirit in exploring the causes, close collaborative style in multi-cooperation, which were attributed to the discovery of the cause in a short time period after the onset.
1. The presentation of the issue
1.1 An outbreak of acute gastroenteritis in adults occurred in a short period in the army located in the downstream of Datong River in the west of Lanzhou in the end of November 1982, and the cases with this disease had a sudden onset with systemic debilitating symptoms resembling cholera, and thus a suspected cholera epidemic was reported, and epidemic communications was reported to local health administration departments. Classical type of cholera occurred and terminated in August 1945 in Lanzhou, although there had been a number of EI Tor cholera interruptions without final confirmation. The suspected cholera epidemic in the 1980s must be quickly confirmed or denied in order to safeguard the health of the people living in the affected areas. The government and the health administration departments paid a close attention to this epidemic and immediately implemented measures of prevention and control as well as investigation and related research work.
1.1.1 A survey on general conditions: the number of cases with the same symptoms increased rapidly in the epidemic area since November 26 from a garrison with seven to eight cases up to more than 10 cases daily and reached the peak with 60% officers affected on December 8. Cases with severe dehydration required intravenous rehydration therapy to relieve the symptoms, because antibiotic therapy failed. The disease course was about four to five days and it required half a month for the patients to complete physical rehabilitation. Although no dead cases and sequelae were found, vomited substances from the cases were collected for the Vibrio cholerae testing.
1.1.2 Investigation of outbreak factors: no suspicious recipes clues were found in collective dining persons and some military dependents had the same disease. The typical clinical features were digestive tract symptoms, therefore the factor of the respiratory tracts was not considered and fecal-oral transmission was given the priority in further consideration. After excluding food factors, the drinking water was the suspected focus. Water source was the Datong River, which was dealt through sedimentation without filtration and artificial bleaching powder disinfection. Cases occurred on the 26th after stopping disinfection on November 20, and the outbreak also occurred in factories and rural areas drinking the water from the same pipe; however, no cases occurred in a nearby garrison squad drinking a spring shared with farmers. Therefore, initial impression was that this epidemic was caused by water pollution and immediate switching to the springs used by the squad terminated the epidemic in the mid-December. Meanwhile Vibrio cholerae was not founded in the bacteria testing, thus suspected cholera epidemic was excluded and the conclusion was an acute diarrhea related to drinking water with an unknown cause.
1.1.3 Relevance to water: there were a factory, three coal mines and a resident community about 3, 5 and 8 km, respectively, away from the water upstream pumping station in the garrison, and industrial and hospital sewage water was discharged into the river without purification, which caused water-borne epidemic.
1.1.4 Unknown cause: the concept and scope of epidemiological investigation as well as modern technology prompted us to conduct further investigation and research to identify the unknown cause.
1.2 What was the nature of the acute gastroenteritis if this was not cholera?
1.2.1 Similar outbreak and epidemic occurred near the garrison region: the number of cases occurred on December 9, increased in the middle of the month and formed an epidemic 3 kilometers downstream the garrison at the No. 205 Factory located in the Haishiwan region on the north shore of Huang River at the convergence point of Datong River and Xishui River. The occurrence of cases began two weeks later than the incidence time of upstream and was terminated in the last third part of December after reinforced disinfection of drinking water and sanitation publicity.
1.2.2 Management of water source at the No. 205 factory: water intake point was located at the convergence point of Datong River and Xishui River, and industrial water and water for domestic use shared the same water conveyance pipelines. Due to a lesson from water-typhoid and dysentery epidemic, automatic chlorination was sustained in the winter. When the outbreak occurred, since the engineer was on his duty and the apprentice engineer forgot to perform chlorination for eight hours from 0:00 ˜ 8:00 on December 8, and cases occurred on December 9 and increased thereafter There were no chlorine volume records in water quality testing records from November 23 to December 10. Obviously, the existing water management system was not seriously implemented during this period.
1.2.3 Pathogen testing: 86 stool specimens of patients with acute enteric pathogens were collected for known intestinal pathogenic bacteria testing. In addition to three samples detected with Fujian’s dysentery, the remaining 83 specimens were found not to have common pathogenic bacteria, such as cholera bacteria, Salmonella, Yersinia enterocolitica Salmonella, Campylobacter jejuni chemoheterotroth, which confirmed that the pathogens leading to the outbreak were not bacteria.
1.2.4 Water quality testing: from the water source of Datong River at the northwest end point of the No. 306 factory to water source of Huangshui River at the No. 205 factory, pollution index of 11 sections in this 40-kilometer distance gradually increased from upstream to downstream, and the situation in downstream was much worse than that of the upstream. TBC (please spell this out) varied from 10 to 43000 per ml. and intestinal bacteria count varied from 23 to 23800 per litter. Pathogenic bacteria and harmful chemicals were not detected at the sewage outfall of factories and mines, and water quality examination records by the environmental protection department were consistent with national standards for sewage disposal
According to pollution index testing results of patient feces, pathogenic bacteria in sewage water and water source may be contaminated by the feces, and in this outbreak of non-bacterial acute gastroenteritis, it was thought that the water was gradually contaminated with increased fecal contents and river water was not disinfected for drinking purpose. Therefore, the cause was water, and it was reasoned that the pathogen may be a virus that possibly caused a larger scale of water-borne diarrhea epidemic and and the transmission was through water. To find out the real pathogens leading to this epidemic, we first conducted a field descriptive epidemiology study to further provide clues to the cause and pathogen
assumptions.
assumptions.
2. Preliminary investigation
2.1 Clinical performance of patients staying in the hospitals
Statistical analysis was conducted on 165-333 case records in three staff hospitals of the No. 306 factory, the mine region and the No. 205 factory.
The latent period was one to 10 days with an average period of 4.6 days. This disease had a sudden onset mostly without obvious prodromal symptoms, starting from diarrhea and vomiting and followed by borborygmus, abdominal distention, and abdominal pain. The stools were watery and yellow in the diarrhea without tenesmus and bloody purulent stools, and a small number of patients had excretion substances like slops. Half patients had different degree of dehydration symptoms, and most cases felt systemic deliberating, uncomfortable, and dizzy with fatigue.
There were 56.3% of the cases having diarrheas 10 to 20 times daily, and 13.8% of the cases having diarrheas more than 20 times daily, in which watery stool accounted for 95.4%, sloppy stool for 1.2%, soft stool for 3.1% and mucous stool for 0.3%. There were 63.1% of the cases having abdominal pains accompanied by press pain, 59.8% of the cases having abdominal distension and borborygmus, and 0.9% cases having sural spasm. There were 49.3% of the cases having dehydration, in which 5.4%-11.0% of the cases had a shock. Most cases had normal body temperature and cases with body temperature higher than 37.5 degrees only accounted for 10.0%. Cases had lower blood pressure and higher levels of hemoglobin and white blood cells with blood condensation. Stool normal testing showed that 75.9% of the cases had a few white blood cells, 14.9% of the cases with a few red blood cells, 4.9% of the cases with a few pus balls and 2.3% of the cases with a few fat balls. Antibiotics treatment showed no efficacy but intravenous rehydration therapy had a significant efficacy. The disease course was 1 to 14 days with an average period of 5.8 days with good prognosis but no death or sequela.
2.2 Population characteristics of this disease natural hisytory
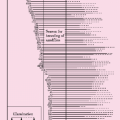
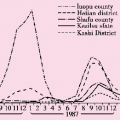
2.2.1 This disease spread fast to a wide range in the affected areas and was concentrated in its course: 10 days before the outbreak in the garrisons downstream the Datong River, and then there had been increasing cases with diarrhea in an upstream mine region. Later the disease spread downstream and upstream along with the river with a center in the Yaojie region where people in the mine region had aggregative activities. Going southeast along with Datong River from the No. 3065 factory through Huangshui River and Yellow River and flowing east through the city and then flowing northeast to Baiyin region, there were outbreak, epidemic or spattered occurrence in miners on the banks of 300-kilometer U-shape valley. Except for Wanchuan River in Yuzhong county and Zhuanglang River in Yongdeng country, 3 counties and 6 regions in the city were all involved, and the incidences in all administration regions from upstream to downstream along the river were listed in Table 7.1. Cases in the Honggu region and Yongdeng County were distributed in the people in the factories and mines on the banks of Huangshui River and Datong River. Analyzed from the aspect
of epidemic time, the No.205 factory experienced a water-borne outbreak lasting for 17 days from December 9 to 25 with a remaining “epidemic tail”. The epidemic curve for the Yaojie mine region was very sharp, which decreased one month later. The epidemic curve for the No. 306 factory seemed like an epidemic process of the living contact type. The disease lasted for 3 months in this city from the middle part of of November in 1982 to the third part of December in 1983, mainly concentrated in the winter.
of epidemic time, the No.205 factory experienced a water-borne outbreak lasting for 17 days from December 9 to 25 with a remaining “epidemic tail”. The epidemic curve for the Yaojie mine region was very sharp, which decreased one month later. The epidemic curve for the No. 306 factory seemed like an epidemic process of the living contact type. The disease lasted for 3 months in this city from the middle part of of November in 1982 to the third part of December in 1983, mainly concentrated in the winter.
Table 7.1 The attack rate of adult epidemic diarrhea in all administration regions in Lanzhou | ||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
2.2.2 Attack rate: There were a total of 5942 cases reported in the city and the attack rate was 97.78 per ten thousand, in which 4477 cases were reported in two epidemic areas in the drainage area of Datong River and Huangshui River with an attack rate of 297.40 per ten thousand as many as 3.04 times the city level. A total of 5670 persons were screened in these two epidemic areas, and 726 cases with diarrhea were detected with an attack rate of 1280.42 per ten thousand as many as 13.09 times the city level, 4.31 times the level of outbreak epidemic areas and 3-4 times the total incidence rate of legal communicable disease in the city. If gastrointestinal dysfunction cases without diarrhea symptoms were added, the actual attack rate would be much higher.
Table 7.2 the attack rate of adult epidemic diarrhea in age groups | ||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree