5. The control of food intake and absorption of nutrients
Anne Payne
LEARNING OBJECTIVES
By the end of this chapter, the reader will be able to:
• Explain both the hormonal and neural control of appetite and food intake;
• Define the role of the stomach, small intestine and colon in the absorption of food and fluids;
• Describe the process for the absorption of fat, protein, carbohydrate, key micronutrients and fluid at the mucosal membrane; and
• Identify immunological cells that confer protection in the gut.
Introduction
The gastrointestinal tract is not a single entity but a system of highly specialist organs working in synergy to enable maintenance of energy balance, nutritional status and physical function. It’s associated immunological and microbiological activity support maintenance of gut health and homeostasis. This chapter will briefly review the process of food intake and nutrient absorption and is intended to link with subsequent chapters to explain and contextualise, for example, drug-nutrient interactions, the complications of enteral and parenteral nutrition, the causes and consequences of symptoms of irritable bowel disease and colorectal cancer and the consequence of surgical intervention in short bowel syndrome.
Overview of the control of food intake
Intake of food is a bio-behavioural response controlled by hunger, the taste and smell of food and psychological effects. Longer-term appetite regulation may be influenced by hormones such as insulin and leptin and governed by the size of adipose stores. Shorter-term regulation and the duration of meals may be influenced by numerous gastrointestinal peptides such as cholecystokinin (CCK), peptide YY, ghrelin and glucagon-like peptide 1 secreted in repose to nutrient stimulation/ inhibition. Integration of these systems at the level of the hypothalamus can then control the release of various neuropeptides influencing appetite regulation. When food is eaten it is ground to a paste in the mouth, mixed with saliva secreted by the salivary glands and then swallowed by reflex action into the oesophagus from where it is passed rapidly by peristaltic motion into the stomach. Saliva contains mucins to lubricate food and salivary amylase to initiate starch digestion. The process of swallowing food is achieved by the musculature of the tongue, pharynx and oesophagus. Difficulty in swallowing, known as dysphagia, is further discussed in Chapter 20, Management of Stroke.
The structure of the GI tract is shown in Figure 5.1.
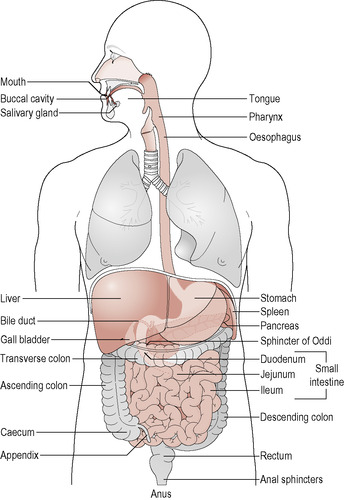 |
| Figure 5.1 • From Clancy J and McVicar AJ (eds) Physiology and Anatomy: A Homeostatic Approach, 2nd edn. London: Arnold, 2002: 236, Fig 10.2. |
The stomach
In the stomach food is mixed with gastric juice and further churned into a bolus termed chyme. The stomach is a highly acidic environment, with a typical pH of 3.0 due to the secretion of hydrogen ions (H +) by the parietal cells of the stomach. The rate of secretion of H + and thus acidity of the stomach is related to both the oral stage of food intake and distension of the stomach by food, with pH decreasing after a meal. The oral stage stimulates the vagus nerve to produce acetylcholine and histamine to activate secretion of H +. Distension of the stomach also activates secretion of H + via the release of the hormone gastrin from G cells in pyloric glands.
The resultant hydrochloric acid produced in the stomach has several actions. It converts inactive pepsinogens, secreted by the chief cells of the gastric glands, into active pepsin enzymes to commence the digestion of protein. It also has a front line role in protection from ingested pathogens as it kills the majority of ingested micro-organisms. Protection of the stomach from its acidic content is achieved by secretion of an alkaline mucus gel, known as the gastric mucosal barrier, onto the surface of the mucosa by gastric epithelial cells. A key function of the stomach is the synthesis and secretion of intrinsic factor by the parietal cells in the lower region of the stomach wall, essential for the subsequent absorption of vitamin B 12 in the ileum of the small intestine. Surgical bypass of the lower stomach due to either stomach carcinoma or bariatric treatment for obesity may require intramuscular vitamin B 12 therapy to avoid the development of symptoms of pernicious anaemia.
The rate of release of the stomach contents into the duodenum is influenced by the volume of food and fluid taken at a meal and by hormonal and neural feedback mechanisms, including that of CCK. The presence of fatty acids in the distal parts of the small intestine also influences food intake and gastric emptying. For example, fatty acids in the ileum stimulate the release of CCK and peptides to inhibit gastric motility and thus reduce the rate of gastric emptying. CCK also stimulates intestinal motility and the secretion of bile and pancreatic enzymes.
The GI tract is predominantly under parasympathetic neural control by the vagus nerve of the autonomic nervous system. This runs from the oesophagus to the upper portion of the colon and is largely composed of sensory neurons. Gastric activity, pancreatic secretions and gall bladder contraction are all under vagal control by the action of sensory receptors to monitor the distension of the GI tract and to respond to changes in concentration of secretions in the lumen. Neurotransmitters include serotonin, noradrenaline and acetylcholine. When a meal is eaten neurotransmitter feedback contributes to a feeling of fullness and satiety to control food intake.
The small intestine
The small intestine is a long coiled tube of approximately 6–10 m in length, comprising the duodenum (25 cm), jejeunum (> 2.5 m ) and ileum (> 3.5 m). The inner surface is often described as having a velvety texture as the highly absorptive villi lining the lumen give its surface a similar physical appearance. Figure 5.2 gives a cross-sectional view of the structure of the small intestine. The large surface area of the mucosa and the abundant capilliary network enmeshed within its mucosa and submucosa aid the rapid adsorption of nutrients. The powerful circular and longitudinal musculature of the intestine propels the food bolus along the length of the GI tract, under the influence of hormones such as CCK, stimulated by the vagus nerve.
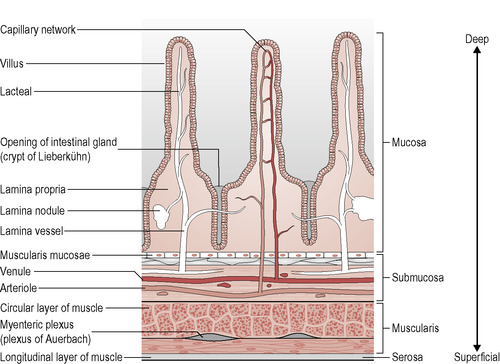 |
| Figure 5.2 • The above figure has been taken from: Geissler C and Powers H (eds) Human Nutrition, 11th edn. London: Elsevier Churchill Livingstone, 2007: 53. |
Bile from the gall bladder is released into the duodenum via the bile duct. The pancreatic duct also joins the small intestine at the duodenum. The pancreas secretes the following enzymes:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



