Treatment modality
Potential side effects
Chemotherapy
Bacterial overgrowth
Bile acid malabsorption
Pancreatic insufficiency
Neutropenic enterocolitis
Edema, ulceration, atrophy
Increased bowel permeability
Transmural infection
Radiation therapy
Radiation enteritis
Stricture
Inflammation/cell death
Progressive ischemia
Fibrosis
Loss of stem cells
Surgery
Ileus
Adhesion formation
Postoperative intussusception
Table 7.2
Etiology of acute abdomen in pediatric oncology patients
Clinical scenario | Underlying etiologies |
|---|---|
Infection | Bacterial |
Viral | |
Fungal | |
Opportunistic | |
Inflammation (acute) | Neutropenic enterocolitis |
Perforation | |
Graft-versus-host disease | |
Pancreatitis | |
Perirectal abscess | |
Appendicitis | |
Inflammation (chronic) | Bowel obstruction |
Adhesions/strictures | |
Intussusception | |
Graft-versus-host disease | |
Pancreatitis | |
Ischemia | Mesenteric ischemia |
Metabolic | Malabsorption |
Hepatic insufficiency | |
VIP secretion | |
Vascular | Mesenteric vascular insufficiency |
Mesenteric thrombosis | |
Venoocclusive disease/sinusoidal obstructive syndrome | |
Primary tumor/secondary malignancy | Obstruction |
Perforation | |
Hemorrhage | |
Abdominal compartment syndrome | |
Pancreatitis | |
Congenital/anatomic | Meckel’s diverticulum |
Intestinal duplication |
Table 7.3
Summary of treatment strategies and level of evidence for management of acute abdomena
Clinical scenario | Recommendations | Level of evidenceb |
|---|---|---|
Neutropenic enterocolitis/typhlitis | Initial evaluation with ultrasound | 1C |
CT if high clinical suspicion and US nondiagnostic | 1C | |
Initial complete gut rest (NPO) | 2C | |
Parenteral nutrition while NPO | 1C | |
Nasogastric suction for decompression | 2C | |
Narcotics for analgesia | 1C | |
Consideration for GCSF utilization | 2C | |
Broad antimicrobial coverage | 1C | |
Surgery only if supportive care fails to improve clinical picture | 1C | |
Appendicitis | Initial evaluation with US | 1C |
CT if US equivocal | 1C | |
Surgical management if strong concern for appendicitis based on exam or imaging findings | 1C | |
Perirectal abscess | Sitz baths for symptomatic relief | 1C |
Laxatives and stool softeners to minimize painful defecation and prevent trauma | 1C | |
Broad-spectrum antibiotics | 1C | |
Surgery only if supportive care fails to improve clinical picture | 1C | |
GI hemorrhage | Acute stabilization; fluid support, PRBC transfusion, vasopressors | 1C |
Elevate head of bed to 30–45° | 2C | |
Keep hemoglobin >8 g/dL and platelets >75 × 109/L | 1C | |
Correction of coagulopathy with FFP | 1C | |
Consideration for gastric lavage | 2C | |
Endoscopic evaluation and management | 1C | |
Pancreatitis | CT with IV contrast for evaluation | 1C |
Consideration for US as primary imaging modality | 2C | |
Early introduction of enteral feeding | 1C | |
Early oral refeeding in those with mild pancreatitis | 2C | |
Narcotics for analgesia | 1C | |
Antiemetics as needed | 1C | |
Broad-spectrum antibiotics in the patient with necrotic pancreatitis and clinical deterioration | 1B | |
Consideration for octreotide | 2C | |
Bowel obstruction | Initial evaluation with KUB followed by abdominal CT | 1C |
Avoidance of barium in neutropenic patients | 1C | |
Initial complete gut rest (NPO) | 1C | |
Parenteral nutrition while NPO | 1C | |
Nasogastric suction for decompression | 1C | |
Narcotics for analgesia | 1C | |
Antiemetics as needed | 1C | |
Surgery if with persistent bleeding, intraperitoneal perforation, clinical deterioration, or presence of a mass | 1C | |
Tumor rupture/organ perforation | Acute stabilization; fluid support, PRBC transfusion, vasopressors | 1C |
Initial complete gut rest (NPO) | 1C | |
Nasogastric suction for decompression | 1C | |
Broad-spectrum antibiotics | 1C | |
Surgical evaluation/intervention | 1C | |
Abdominal compartment syndrome | Diagnosis based on IAP ≥20 mmHg | 2C |
Nasogastric suction for decompression | 1C | |
Avoidance of elevation of head of bed, sedatives, and analgesics which may all increase IAP | 2C | |
Percutaneous catheter decompression of intraperitoneal air or fluid | 1C | |
Optimize fluid balance with hypertonic crystalloids and colloids | 1C |
7.2 Gastrointestinal Infection
Infection is a common complication of children undergoing cancer treatment; nearly one-third of these infections originate from the GI tract (Hobson et al. 2005). GI tract infection results from direct chemotherapeutic toxicity, opportunistic infections, and common conditions such as rotavirus or Clostridium difficile that also affect healthy children. Typhlitis and appendicitis were the most common surgical complications in pediatric leukemia patients, occurring at frequencies of 1.7 % and 1.5 %, respectively, among children treated at a single institution (Hobson et al. 2005). Detailed history and physical exam, neutrophil count, stool cultures, and appropriate diagnostic imaging studies are necessary to establish the correct diagnosis and guide treatment. When the etiology remains unclear, diagnostic laparoscopy offers a minimally invasive approach to visually inspect the peritoneal cavity.
7.2.1 Neutropenic Enterocolitis
Neutropenic enterocolitis refers to necrotizing inflammation of the small or large intestine that occurs in the setting of neutropenia. Typhlitis specifically refers to necrotizing inflammation of the cecum, the most commonly affected bowel segment (Arul and Spicer 2008). Though usually seen with prolonged neutropenia (i.e., >7 days), typhlitis has been reported without neutropenia (McCarville et al. 2005). The watershed vasculature and distensibility of the cecum may explain its predilection for infection compared to other bowel segments. With earlier diagnosis and intervention, current mortality rates for typhlitis are approximately 2.5 % (Haut 2005; Pizzo 2011). Factors that may contribute to the development of neutropenic enterocolitis include: (1) prophylactic antibiotics which alter normal colonic flora; (2) cytotoxic chemotherapy which disrupts the bowel mucosal barrier permitting microbial and fungal invasion which may lead to hemorrhage and necrosis; and (3) prolonged neutropenia which prevents adequate infection clearance and predisposes to sepsis (Arul and Spicer 2008).
Bacterial pathogens account for >90 % of enterocolitic infection. The most common bacterial pathogens include Escherichia coli, Pseudomonas aeruginosa and Clostridium difficile (Haut 2005). Less common bacterial pathogens include coagulase-negative staphylococcus and alpha-hemolytic streptococcus. The most common fungal pathogens are Candida spp. (Albano and Sandler 2004; Fisher and Rheingold 2011; Pizzo 2011). Typhlitis typically develops in patients >10 years of age and within 2–3 weeks of receiving intensive chemotherapy (McCarville et al. 2005; Sundell et al. 2012). Case series suggest that patients with acute myelogenous leukemia (AML) are at high risk for typhlitis in any phase of therapy (Gray et al. 2010).
Symptoms of neutropenic enterocolitis are nonspecific and highly variable and include abdominal pain, vomiting, diarrhea and GI bleeding (McCarville et al. 2005; Sundell et al. 2012). Signs can include fever, abdominal distension, tachycardia, hypotension, sepsis, and peritoneal irritation that can be diffuse or localized to the right lower quadrant (Sundell et al. 2012). Uncommonly a cecal mass is palpable (Haut 2005; Gray et al. 2010). Appendicitis, pancreatitis, pseudomembranous colitis, intussusception, and pelvic or peritoneal abscess should be considered in the differential diagnosis.
In the neutropenic patient with acute abdominal pain, a two-view plain radiograph should first be obtained as it may show an appendicolith, pneumatosis, or free air. Plain radiographs may support the diagnosis of enterocolitis with findings of pneumatosis and bowel wall thickening although most findings are nonspecific (Fisher and Rheingold 2011; Pizzo 2011; Sundell et al. 2012). Presence of free air will require immediate surgical consultation and intervention. Contrast enema is contraindicated if neutropenic enterocolitis is suspected as it may lead to perforation (Arul and Spicer 2008; Morgan et al. 2011).
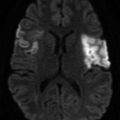
Ultrasound (US) is the preferred imaging modality for demonstrating bowel wall thickening (McCarville et al. 2005). A diagnosis of enterocolitis consists of bowel wall thickening >3 mm, and mortality rates increase when bowel wall thickening exceeds 10 mm (Pizzo 2011; Sundell et al. 2012). If US results are inconclusive, computed tomography (CT) is the current definitive imaging study (Cloutier 2010; Pizzo 2011). CT is very sensitive for identifying cecal wall thickening, transmural inflammation, soft tissue masses and pneumatosis. A characteristic feature of typhlitis on CT is necrosis localized to the cecum. Both US and CT may reveal a target sign, an echogenic center with a wide hypoechogenic periphery, at the cecum in typhlitis. CT may overestimate bowel wall thickening leading to false-positive diagnoses of enterocolitis and typhlitis. Magnetic resonance imaging (MRI) for the diagnosis of neutropenic enterocolitis has not been reported in the medical literature.
Supportive management of enterocolitis has typically included complete gut rest (NPO) during the acute phase of symptomatic pain, parenteral nutrition while NPO and nasogastric suctioning for decompression (Sundell et al. 2012). However, evidence regarding the benefit of these interventions is lacking. Narcotics should be utilized for analgesia. Vasopressor support may be required; hypotension is associated with poor outcome. Patients may require packed red blood cell and platelet transfusions (Albano and Sandler 2004; Pizzo 2011). The utility of granulocyte colony-stimulating factor (GCSF) in patients with enterocolitis is unclear, and the use of GCSF is discussed in more detail in Chap. 15. A non-evidence-based argument to support GCSF use is generally that resolution of neutropenia parallels resolution of typhlitis (Fisher and Rheingold 2011). On the other hand, GCSF could theoretically increase inflammation and cause obstruction.
Early imaging and rapid initiation of antimicrobials are vital, as these interventions may decrease mortality in neutropenic enterocolitis. Antibacterial therapy should be broad to cover for enteric pathogens, especially Gram-negative and anaerobic microbes in addition to Gram-positive enterococcal species. Cloutier (2010) suggests that monotherapy with piperacillin-tazobactam or imipenem-cilastatin or dual therapy with either ceftazidime or cefepime with metronidazole is sufficient initial coverage for neutropenic enterocolitis. Metronidazole is the generally preferred anaerobic coverage given the similar clinical features of typhlitis and pseudomembranous enterocolitis due to C. difficile (Sundell et al. 2012). Such regimens have not been specifically studied in pediatric neutropenic enterocolitis. Typhlitis is an oncologic emergency because it may lead to bowel obstruction or perforation requiring surgical intervention (Haut 2005). Consultation with surgery should be requested early, even if surgery is not anticipated. Surgery should be deferred until supportive therapy has clearly failed or the following complications develop: perforation, hemorrhage despite correction of thrombocytopenia and coagulopathies, obstruction, necrosis, abscess or peritonitis requiring drainage, fistula, toxic megacolon, or septic shock (Gray et al. 2010; Morgan et al. 2011; Sundell et al. 2012). Surgery consists of visualization and management of bleeding, resecting necrotic portions of the bowel, and possible transient diversion via colostomy (Pizzo 2011).
7.2.2 Appendicitis
Incidence of appendicitis in pediatric leukemia and lymphoma is the same as the general population, ranging from 0.5–1.5 % (Hobson et al. 2005; Fisher and Rheingold 2011). Signs and symptoms of appendicitis may overlap with neutropenic colitis; in the patient who does not improve with medical management for enterocolitis, the physician should consider appendicitis (Albano and Sandler 2004). In the review by Hobson et al. (2005), they found that pediatric oncology patients had inconsistent clinical signs and symptoms of appendicitis, routinely lacked fever and often lacked localizing signs on abdominal exam. However, in a similar cohort, Chui et al. (2008) reported that fever was common and the majority presented with localizing abdominal signs prior to surgery. In both cohorts, a delay in diagnosis was common (Hobson et al. 2005; Chui et al. 2008).
Although a KUB may show an appendicolith to diagnosis appendicitis, a staged protocol with US followed by CT in those patients with an equivocal US has been found accurate and cost-efficient in the regular pediatric population while reducing radiation exposure (Wan et al. 2009; Krishnamoorthi et al. 2011). Whether this methodology is effective for pediatric oncology patients is unknown. Hobson et al. (2005) noted that CT evaluation was not accurate in their cohort of pediatric oncology patients, with only 2 of 7 patients having classic CT findings. Again, Chui et al. (2008) reported dissimilar results as 8 of 10 patients had CT imaging consistent with appendicitis. Additionally, patients with typhlitis have been noted to have appendiceal thickening of uncertain significance in a small percentage of cases and not correlated with development of appendicitis (McCarville et al. 2004). Isolated appendiceal typhlitis has also been noted in case reports (McAteer et al. 2014).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree