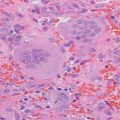
Fig. 20.1
Intraoperative parathyroid hormone levels after sequential resection of hyperplastic right inferior and left inferior parathyroid glands to treat tertiary hyperparathyroidism in a patient with pseudohypoparathyroidism type Ib
Outcome
At 10-year follow-up, she felt well. Her serum calcium remained in the normal range with consistent use of 1000 mg elemental calcium daily, 1,25-dihydroxyvitamin D 0.25 mcg daily, and hydrochlorothiazide 25 mg every other day over 10 years of follow-up. PTH remained elevated but stable at 7.8 pmol/L. BMD remained normal and above average for age.
Clinical Pearls/Pitfalls
Chronic stimulation by mild ionized hypocalcemia due to chronic PTH resistance and related disorders may result in parathyroid gland hyperplasia and even greater extent of PTH elevation sufficient to cause mild hypercalcemia.
Tissue-specific decreases in Gsα expression in the proximal renal tubules with preserved expression in bone and other tissues may be clinically evident in disorders such as pseudohypoparathyroidism type Ib and may influence determination of optimal PTH concentrations in such patients.
In patients with underlying conditions for whom elevated serum concentrations of PTH may be necessary to optimize physiologic functions related to calcium and phosphorus, need for and extent of parathyroidectomy should be carefully discussed with an endocrine surgeon.
Conflicts of Interest
All authors state that they have no conflicts of interest.
References
1.
2.
3.
Jüppner H, Gardella T, Brown E. Parathyroid hormone and parathyroid hormone-related peptide in the regulation of calcium homeostasis and bone development. In: DeGroot L, Jameson J, editors. Endocrinology: adult and pediatric. 7th ed. Philadelphia: Elsevier; 2015.
4.
5.
Moallem E, Kilav R, Silver J, Naveh-Many T. RNA-protein binding and post-transcriptional regulation of parathyroid hormone gene expression by calcium and phosphate. J Biol Chem. 1998;273:5253–9.PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree