Fig. 19.1
Schematic examples of HGF/MET and/or VEGF/VEGFR inhibitors mechanism of action. VEGFR vascular endothelial growth factor receptor, PDGFR platelet-derived growth factor receptor, HGF hepatocyte growth factor, FLT3 FMS-like tyrosine kinase 3, PI3K phosphoinositide 3-kinase, AKT protein kinase B, mTOR mammalian target of rapamycin, PTEN phosphatase and tensin homolog
HGF/MET
The HGF/MET axis has been targeted using both monoclonal antibodies and small molecule tyrosine kinase inhibitors (TKI). Rilotumumab (AMG102) is a fully human monoclonal antibody against HGF. A phase II trial randomized 142 men with progressive taxane-refractory CRPC to mitoxantrone (12 mg/m2 every 3 weeks) with prednisone (5 mg twice daily) plus rilotumumab (15 mg/kg IV every 3 weeks), rilotumumab (7.5 mg/kg IV every 3 weeks) or placebo (1:1:1 randomization) [41]. Rilotumumab did not improve OS or progression-free survival (PFS) (median OS: 12.2 vs 11.1 months, HR 1.10; median PFS 3 vs 2.9 months, HR 1.02, in the combined rilotumumab vs control). Rilotumumab was well tolerated with peripheral edema (24 vs 8 %) being more common compared to control. The MET TKI tivantinib (ARQ197) is currently being studied in a randomized, blinded, placebo-controlled phase II trial in asymptomatic or minimally symptomatic metastatic CRPC. Planned enrollment is 78 patients and an estimated primary completion date of July 2014 (NCT01519414). Another small molecule MET inhibitor (AMG 208) was tested at a dose ≤400 mg daily in a phase I study and had manageable toxicities with evidence of anti-tumor activity, especially in prostate cancer [42]. Several other compounds targeting HGF/MET signaling are in early phases of clinical development, including the monoclonal antibodies onartuzumab (MetMab), TAK-701, and ficlatuzumab (SCH900105) and small molecule TKIs SGX523, PF-04217903, EMD 1214063, EMD 1204831, PF-02341066 (crizotinib), BMS-777607, SAR125844, JNJ 38877605.
VEGF/VEGFR
Four anti-angiogenesis compounds have been tested in phase III trials in CRPC; none, however, improved OS. A fifth agent is currently undergoing phase III evaluation (Table 19.1).
Table 19.1
Phase III trials with HGF/MET and/or VEGF/VEGFR inhibitors in patients with CRPC
Trial identifier | Agent | Disease | Number of patients | Arms | Primary endpoint | Outcome |
|---|---|---|---|---|---|---|
(CALGB 90401) NCT00110214 | Bevacizumab | Metastatic CRPC (chemotherapy-naive) | 1,050 | Docetaxel/prednisone + bevacizumab 15 mg/kg IV every 3 weeks or placebo | OS | No difference in OS |
NCT00676650 | Sunitinib | Metastatic CRPC (chemotherapy-treated) | 873 | Sunitinib 37.5 mg po daily or placebo | OS | No difference in OS |
NCT01234311 | Tasquinimod | Metastatic CRPC (chemotherapy-naive) | 1,200 (target) | Tasquinimod (0.25, 0.5, 1 mg po daily) or placebo | PFS | Ongoing |
(VENICE) NCT00519285 | Aflibercept | Metastatic CRPC (chemotherapy-naive) | 1,224 | Docetaxel/prednisone + aflibercept (6 mg/kg every 3 weeks) or placebo | OS | No difference in OS |
(MAINSAIL) NCT00988208 | Lenalidomide | Metastatic CRPC (chemotherapy-naive) | 1,059 | Docetaxel/prednisone + lenalidomide (25 mg po daily, days 1–14) or placebo | OS | No improvement in OS |
(COMET-1) NCT01605227 | Cabozantinib | Metastatic CRPC (treated with docetaxel and either abiraterone or enzalutamide) | 960 (target) | Cabozantinib 60 mg po daily or prednisone 5 mg po twice daily | OS | Ongoing |
(COMET-2) NCT01522443 | Cabozantinib | Metastatic CRPC (treated with docetaxel and either abiraterone or enzalutamide) | 246 (target) | Cabozantinib 60 mg po daily or mitoxantrone/prednisone (maximum of 10 infusions of chemotherapy or placebo) | Confirmed pain response | Ongoing |
Bevacizumab
Based on phase II data from trials of docetaxel, bevacizumab, thalidomide, and prednisone, as well as bevacizumab combined with docetaxel/estramustine [43, 44], CALGB 90401 randomized 1,050 patients with progressive, metastatic CRPC to docetaxel (75 mg/m2 every 3 weeks), prednisone (5 mg twice daily), and either bevacizumab (15 mg/kg IV every 3 weeks) or placebo [45]. There was no significant difference in OS (22.6 vs 21.5 months, respectively; HR 0.91; p = 0.181). Median PFS (9.9 vs 7.5 months; p < 0.001) and objective response rate (49.4 vs 35.5 %; p = .0013), as well as treatment-related toxicity (75.4 vs 56.2 %; p ≤ .001) and treatment-related deaths (4 vs 1.2 %; p = .005) were higher in the bevacizumab arm. Enrollment of patients with more co-morbidities in the bevacizumab arm and treatment duration were suggested as potential reasons for the discordant PFS and OS in this trial [46, 47]. Patients discontinued bevacizumab at the time of PSA or radiographic progression before consensus guidelines were implemented discouraging discontinuation of therapy on the basis of PSA progression alone without clinical progression. The analysis of prospectively collected biomarkers in this study may identify a subset of patients who may have benefited from the combination therapy.
Sunitinib
Sunitinib showed anti-tumor activity in two phase II trials of patients with metastatic CRPC who had progressed on docetaxel [48, 49]. Unplanned post-hoc analyses of bone scans from one of these trials noted a relatively high rate of bone scan response to sunitinib, with none of patients with bone scan response experiencing concordant lowering of PSA or CT evidence of response by accepted criteria [50]. A phase III trial randomized 873 men with metastatic CRPC progressive after docetaxel to sunitinib (37.5 mg daily) or placebo (2:1 ratio). Results from a second interim analysis reported PFS but no OS improvement (median OS 13.1 vs 12.8 months, respectively; HR 1.03; p = 0.58) and the trial was terminated due to futility [51]. The most common treatment-related grade 3/4 adverse events were fatigue (18.8 vs 7.3 %) and anemia (6.2 vs 5.5 %). A strategy of sunitinib maintenance (50 mg daily on 4/2 week on/off cycle) after response to docetaxel was investigated in a phase II trial [52]. Three grade 4 adverse events occurred in the 23 men enrolled: hepatitis, myelosuppression, pneumonia. Most men had immediate PSA increase without evidence of disease progression. Although sunitinib was well tolerated with predictable toxicity, median PFS of 133 days was lower than the predefined threshold of 180 days. PSA level was not informative, since significant increases were noted as early as second cycle. Finally, a phase I/II trial evaluated sunitinib (2 weeks on, 1 week off) in combination with docetaxel/prednisone in chemotherapy-naive metastatic CRPC [53]. The recommended phase II dose of sunitinib was 37.5 mg daily, with standard dose chemotherapy. During the phase II portion, confirmed PSA response occurred in 56.4 % of patients. Median time to PSA progression was 9.8 months; 42.4 % of assessable men had confirmed partial response. Median PFS and median OS were 12.6 and 21.7 months, respectively. The most frequent treatment-related grade 3/4 adverse events were neutropenia (53 %; 15 % febrile) and fatigue/asthenia (16 %).
Tasquinimod
Tasquinimod is an oral quinolone-3-carboxamide derivative with anti-angiogenic properties resulting in a decrease vascular density. The mechanism of anti-tumor activity is not completely known [54]. In a double-blinded phase II trial, 201 men with metastatic CRPC were randomized to either tasquinimod 1 mg daily after a titration phase (0.25 mg daily for 2 weeks followed by 0.5 mg daily for 2 weeks) or placebo [54]. After 6 months therapy, the blind was broken and asymptomatic men on placebo and those on tasquinimod without disease progression were offered open-label treatment. Six-month progression-free proportion was higher with tasquinimod (69 vs 37 %, p < 0.001) and median PFS was longer (7.6 vs 3.3 months, p = 0.0042). Updated results showed the time to symptomatic progression to be longer with tasquinimod (p = 0.039, HR = 0.42) [55]. Median time to death (34.2 vs 30.2 months) favored tasquinimod particularly in the bone-metastatic subgroup (34.2 vs 25.6 months). These results led to an ongoing phase III trial in men with asymptomatic or mildly symptomatic metastatic chemotherapy-naive CRPC. A total of 1,200 men will be randomized (2:1) to tasquinimod or placebo (NCT01234311); PFS is the primary and OS the secondary endpoint. The estimated study completion date is January 2016. Another study (CATCH) attempts to determine the safety, tolerability, and recommended dose of tasquinimod in combination with cabazitaxel/prednisone in men with chemotherapy-refractory metastatic CRPC (NCT01513733). A third study evaluates the role of maintenance tasquinimod in patients with metastatic CRPC not progressing after docetaxel (NCT01732549).
Aflibercept
Aflibercept is a fusion protein composed of the extracellular domains of VEGFR-1/2 and the constant region (Fc) of the human IgG1 antibody. Aflibercept acts as a decoy receptor, competitively binding VEGF. A phase I dose-escalation trial combined aflibercept with docetaxel in men with advanced solid tumors with preliminary evidence of anti-tumor activity in several tumor types including prostate cancer [56]. Without further assessment of this combination in a prostate cancer-specific phase II study, the VENICE phase III trial randomized 1,224 men with CRPC to docetaxel (75 mg/m2 every 3 weeks)/prednisone (10 mg daily) and either aflibercept (6 mg/kg once every 3 weeks) or placebo [57]. With a median follow-up of 35.4 months and 873 deaths, there was no difference in time to skeletal-related events, PFS and OS in the two arms, and there was a higher incidence of all-grade hypertension, stomatitis, appetite disorders, diarrhea, dehydration, epistaxis, dysphonia, cough, headache, and infections in the aflibercept arm.
Lenalidomide
Lenalidomide is an oral immune-modulatory compound which also inhibits VEGF signaling and angiogenesis [58]. It has a favorable safety profile compared to thalidomide, and showed activity as single agent in non-metastatic biochemically recurrent prostate cancer [59]. A double-blinded phase III trial (MAINSAIL) randomized 1,059 men with chemotherapy-naive, progressive, metastatic CRPC to docetaxel (75 mg/m2 every 3 weeks) with prednisone (5 mg twice daily) and either lenalidomide (25 mg daily, days 1–14) or placebo [60]. In November, 2011, the data monitoring board recommended that the trial is stopped, since it was unlikely to meet its primary endpoint of OS. The median OS was 77 weeks in the lenalidomide arm; the median was not reached in the placebo arm. Treatment with lenalidomide was associated with more neutropenia, febrile neutropenia, and diarrhea. A phase II trial in men with chemotherapy-naïve metastatic CRPC combined lenalidomide and bevacizumab with docetaxel and prednisone in [61]. PSA response >50 % was reported in 85.2 % of patients (N = 54) with objective radiological response in 86.7 % of patients with measurable disease. Most common grade ≥2 adverse events included neutropenia (63 %), anemia (43 %), thrombocytopenia (13 %), hypertension (22 %), and jaw osteonecrosis (22 %). This phase II trial used enoxaparin and peg-filgrastim prophylactically to prevent thromboembolic events and neutropenia and thus maintain patients on therapy [62]. These supportive care measures allowed the combination therapy to be administered for more cycles compared to the MAINSAIL and CALGB 90401 trials potentially resulting in longer PFS, ORR, and possibly OS with an improved adverse event profile. These data suggest that supportive measures may improve the success of intensive combination regimens and are hypothesis-generating for future combination therapy trials. Ongoing trials are further assessing the role of lenalidomide in men with CRPC.
Sorafenib
Sorafenib, a multi-targeted TKI, is FDA-approved for the treatment of metastatic renal cell carcinoma and advanced hepatocellular carcinoma. Several phase II trials have evaluated sorafenib monotherapy in metastatic CRPC reporting modest activity with some discordance between PSA and radiographic response [63–66]. A phase II trial of sorafenib combined with bicalutamide in 39 men with chemotherapy-naive CRPC reported that 47 % of patients had either PSA response or stable disease ≥6 months [67]. PSA decline of ≥50 % occurred in 32 % of assessable patients, including 26 % with prior anti-androgen therapy. Median time to treatment failure was 5.5 months; grade ≥3 adverse events included fatigue, skin rash, and hand-foot syndrome. A phase II study of sorafenib and docetaxel in men with metastatic CRPC was launched but its status is unknown (NCT00589420).
Other Agents
Vandetanib is an oral agent which selectively inhibits VEGFR and epidermal growth factor receptor (EGFR). In men with metastatic CRPC, vandetanib combined with docetaxel/prednisone did not provide any benefit when compared to placebo [68]. The combination of vandetanib with bicalutamide in CRPC is currently being evaluated (NCT00757692, NCT00659438). A phase II trial reported that cediranib, a highly potent VEGFR inhibitor, was well tolerated with some anti-tumor activity in heavily pre-treated men with metastatic CRPC who had progressed after docetaxel-based therapy [69]. A randomized phase II study of docetaxel/prednisone with or without cediranib in men with chemotherapy-naive metastatic CRPC reported that the addition of cediranib to chemotherapy had increased toxicity but may have been associated with higher rate of PSA response and clinical response [70]. Two trials are currently evaluating cediranib in the management of men with metastatic CRPC (NCT01260688, NCT00436956). A phase I study evaluated nintedanib (BIBF 1120), an oral, potent, multi-targeted TKI with anti-VEGFR activity, in combination with standard dose of docetaxel/prednisone in men with metastatic, chemotherapy-naïve CRPC, and reported that 200 mg twice daily was the nintedanib recommended dose [71]. This combination was well tolerated, with preliminary signal of efficacy and no indication of pharmacokinetic interaction between nintedanib and docetaxel. Another study investigated ramucirumab (IMC-1121B, human monoclonal antibody against VEGFR2) vs IMC-A12 (monoclonal antibody against IGF-1R) with mitoxantrone/prednisone in men with prostate cancer progressive on docetaxel [72]. Ramucirumab/mitoxantrone/prednisone was reasonably tolerated, while composite PFS and OS endpoints appeared encouraging. Pazopanib (VEGFR multi-targeted TKI), TRC105 (chimeric IgG1 k monoclonal antibody binding to human endoglin), and AMG386 (selective angiopoietin 1/2 neutralizing peptibody; recombinant peptide-FC fusion protein) are also being evaluated in clinical trials in men with prostate cancer (NCT00486642, NCT00454571, NCT01090765, NCT01553188).
MET/VEGFR
As noted above, cabozantinib is the agent targeting both of these pathways which is furthest along the development pathway. Other therapies that inhibit both MET and VEGFR signaling are in early phases of clinical development, including foretinib (GSK1363089), golvatinib (E7050), GSK1363089 (XL880), and MGCD265.
Cabozantinib
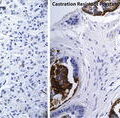
Based on phase I data, a phase II randomized discontinuation study was conducted in nine selected tumor types (study XL184-203), including CRPC. Patients received cabozantinib 100 mg daily during a 12-week lead-in stage. Patients with response by mRECIST criteria continued open-label cabozantinib, those with disease progression discontinued therapy, while those with stable disease were randomized to either placebo or cabozantinib [73]. The primary endpoint for the lead-in stage was response rate by mRECIST criteria; the primary endpoint for the randomized stage was PFS. In the CRPC cohort, a total of 171 men with progressive metastatic disease, measurable by mRECIST criteria, with ≤1 prior standard chemotherapy regimen and maintained on androgen deprivation, were enrolled. Randomization in this cohort was suspended after the first 122 men had been accrued due to unexpected high rate of bone scan response at the lead-in stage. Bone disease was present in 87 % of patients at baseline, while 43 % were previously treated with docetaxel. Median duration of cabozantinib therapy excluding patients randomly assigned to placebo was 4.2 months (0.5–17.2). A total of 5 % of patients had a confirmed partial response within the first 12 weeks, with 75 % having stable disease. In addition, four patients with stable disease at week 12 had a confirmed partial response after the lead-in stage. Moreover, 72 % of patients had at least one assessment showing reduction of soft tissue lesions; change in measurable disease was independent of prior treatment. Improvement in bone scan was documented in 68 % of men, including 12 % with complete resolution. These responses correlated with clinical benefit, with 67 % of assessable men reporting decrease in pain, and 56 % reporting decrease in or discontinuation of narcotics. PSA changes did not correlate with the anti-tumor effects in soft tissue and bone. All men had at least one adverse event, and most experienced more than one. The most common all-grade adverse events included a cluster of symptoms consisting of fatigue, decreased appetite, taste alterations, nausea, diarrhea, weight loss, and PPE (hand-foot syndrome) that resulted in dose reductions in 62 % of patients. These events were mostly managed with drug interruption and/or dose reduction. Most common grade 3 adverse events were fatigue (16 %), hypertension (12 %), PPE (8 %), dehydration (8 %), pulmonary embolism (7 %), decreased appetite (6 %) and nausea (5 %). The authors concluded that cabozantinib had substantial anti-tumor activity in men with advanced CRPC with manageable toxicity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree