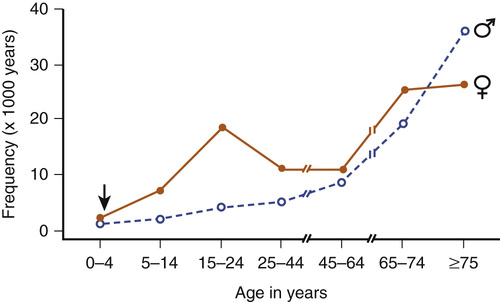
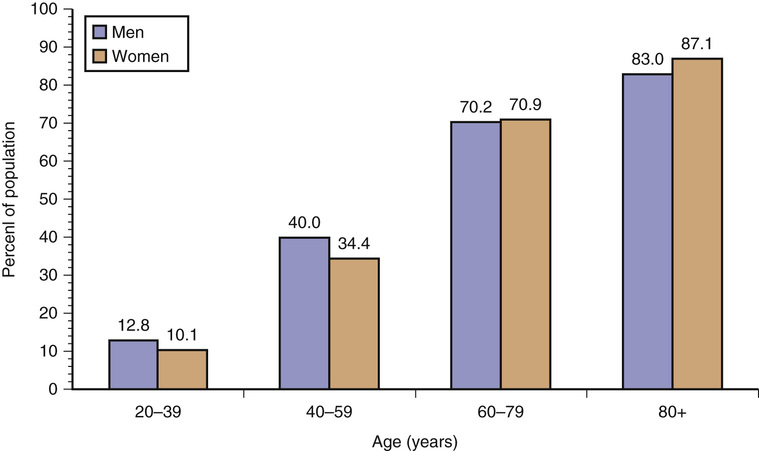
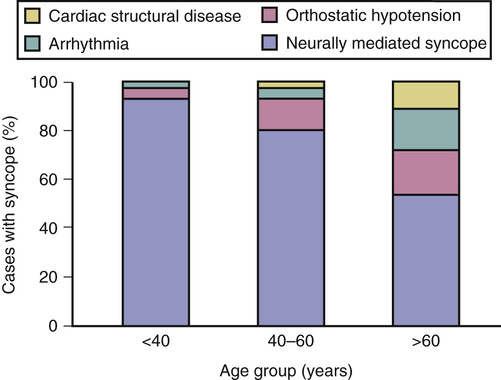
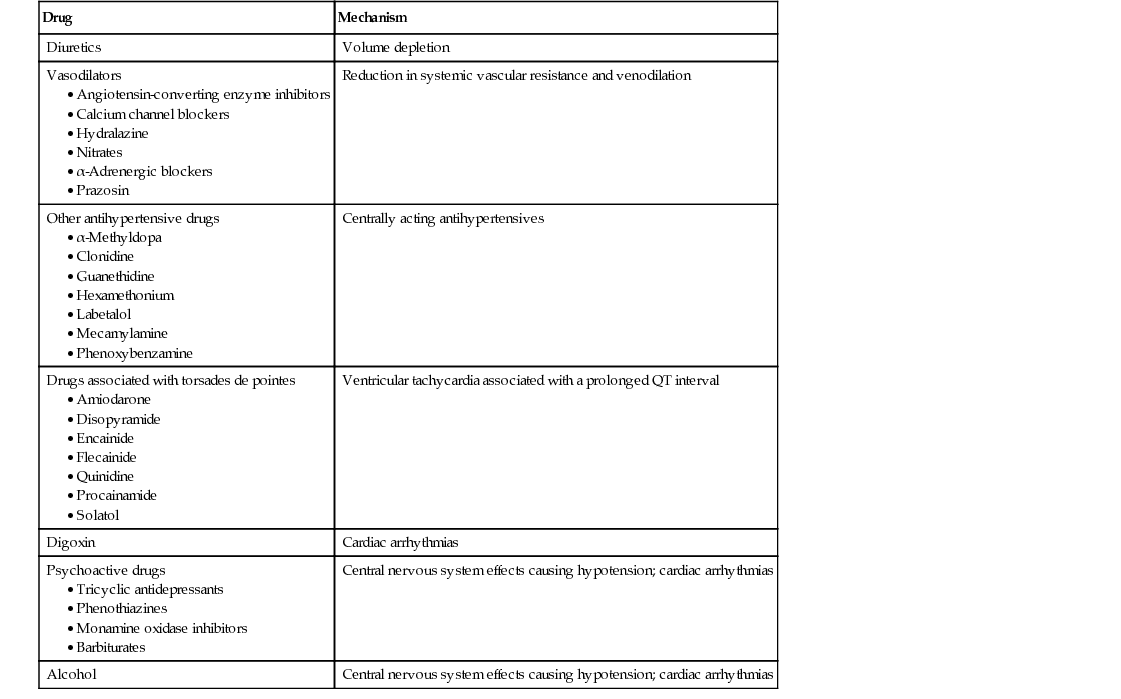
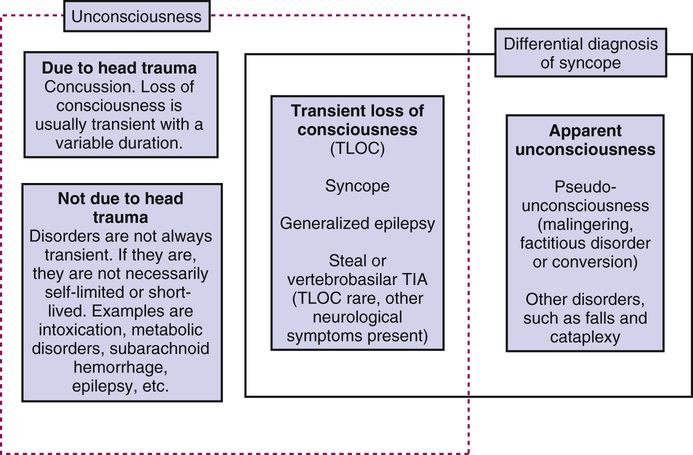
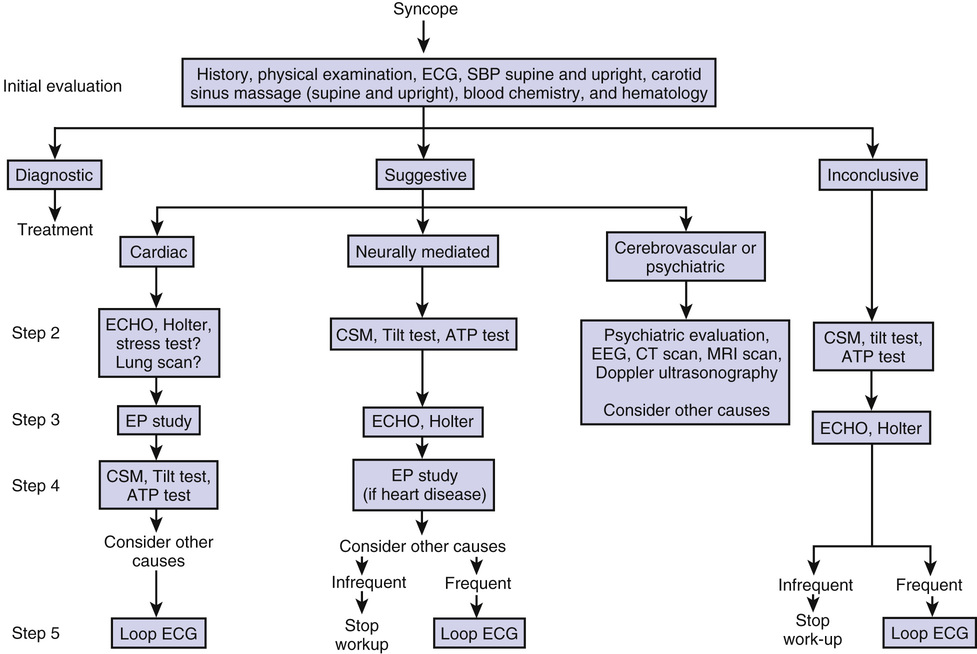
Rose Anne Kenny, Jaspreet Bhangu Syncope is a transient loss of consciousness (TLOC) due to transient global cerebral hypoperfusion and is characterized by rapid onset, short duration, and spontaneous complete recovery. TLOC is a term that encompasses all disorders characterized by self-limited loss of consciousness, irrespective of mechanism. By including the mechanism of unconsciousness—transient global cerebral hypoperfusion—the current syncope definition excludes other causes of TLOC such as epileptic seizures and concussion, as well as certain common syncope mimics such as psychogenic pseudosyncope.1 Syncope is a common symptom, experienced by up to 30% of healthy adults at least once in their lifetime.2 Syncope accounts for 3% of emergency department visits and 1% of medical admissions to a general hospital.3,4 Syncope is the seventh most common reason for emergency admission of patients older than 65 years.5 The cumulative incidence of syncope in a chronic care facility is close to 23% over a 10-year period, with an annual incidence of 6% and recurrence rate of 30% over 2 years. The age of first faint, a commonly used term for syncope, is younger than 25 years in 60% of persons, but 10% to 15% of individuals have their first faint after the age of 65 years.6–8 Syncope due to a cardiac cause is associated with higher mortality rates, irrespective of age.9 In patients with a noncardiac or unknown cause of syncope, older age, a history of congestive cardiac failure, and male gender are important prognostic factors of mortality.10 It remains undetermined whether syncope is directly associated with mortality or is merely a marker of more severe underlying disease.2 Figure 45-1 details the age-related difference in prevalence of benign vasovagal syncope compared to other causes of syncope The Irish Longitudinal Study on Ageing (TILDA; www.tilda.ie) is a population-based study of people aged 50 years and over that has incorporated questions on syncope and falls in addition to a broad spectrum of health, social, and economic questions. A number of community-dwelling adults (N = 8163), mean age 62 years ( range, 50 to 106 years), were asked whether they experienced fainting in their youth, throughout their life, or over the past 12 months. A total of 23.6% had one or more episodes in the previous 12 months, of which 4.4% were syncope and 19.2% were falls (Table 45-1). Although the prevalence of syncope rose with age, the increase in falls was much more remarkable; in particular, the increase in nonaccidental or unexplained falls was most striking. Unwitnessed syncope most commonly presents as an nonaccidental or unexplained fall, supporting the rising prevalence of atypical syncope with advancing years. The General Practitioners’ Transition Project in the Netherlands has demonstrated that the age distribution of patients presenting to their physician with syncope shows a peak in females at 15 years of age and a second peak in older patients (see Figure 45-1).11 The Framingham Offspring study has similarly demonstrated a bimodal peak of first syncope in those in their the mid-teens and the second in those older than 70 years.9 The true prevalence of syncope is underestimated due to the phenomenon of amnesia for TLOC. Amnesia has been reported in patients with vasovagal syncope (VVS) and carotid sinus syndrome (CSS)12–14 but is likely to be present in all causes of syncope. The overlap between syncope and falls also leads to underreporting (see Table 45-1 and Figure 45-1). The temporary cessation of cerebral function that causes syncope results from transient and sudden reduction of blood flow to parts of the brain responsible for consciousness (brain stem reticular activating system). The predisposition to VVS starts early and lasts for decades. Other causes of syncope are uncommon in young adults, but are much more common as persons age.15,16 Regardless of the cause, the underlying mechanism responsible for syncope is a drop in cerebral oxygen delivery below the threshold for consciousness. Cerebral oxygen delivery, in turn, depends on cerebral blood flow and oxygen content. Any combination of chronic or acute processes that lowers cerebral oxygen delivery below the consciousness threshold may cause syncope. Age-related physiologic impairments in heart rate, blood pressure, cerebral blood flow, and blood volume control, in combination with comorbid conditions and concurrent medications, account for the increased incidence of syncope in older adults. Blunted baroreflex sensitivity manifests as a reduction in the heart rate response to hypotensive stimuli. Older adults are prone to reduced blood volume due to excessive salt wasting by the kidneys as a result of a decline in plasma renin and aldosterone levels, a rise in atrial natriuretic peptide level, and concurrent diuretic therapy.15 Low blood volume, together with age-related diastolic dysfunction leading to low cardiac output, coupled with inadequate heart rate responses to stress, increases susceptibility to orthostatic hypotension and VVS.17 Cerebral autoregulation, which maintains a constant cerebral circulation over a wide range of blood pressure changes, is altered in the presence of hypertension and possibly by aging; the latter factor is still controversial.18 In general, it is agreed that sudden mild to moderate declines in blood pressure can affect cerebral blood flow markedly and render an older person particularly vulnerable to presyncope and syncope. Syncope may thus result from a single process that markedly and abruptly decreases cerebral oxygen delivery or from the accumulated effect of multiple processes, each of which contributes to reduced oxygen delivery. Reflex syncope and orthostatic hypotension (OH) are the most frequent causes of syncope in all age groups and clinical settings and responsible for most episodes in younger patients. However, cardiac causes of syncope, structural and arrhythmic, become more common in older patients and are responsible for one third of syncope in patients seen in the emergency room and chest pain unit.1,19–21 The prevalence of unexplained syncope varies according to diagnostic facilities and age from 9% to 41% (see Table 45-1). In the older patient, history may be less reliable, and multiple causes of syncope may also be present (Box 45-1).5,20,22–24 Multimorbidity and polypharmacy are more common in older patients with syncope and can add to the complexity of identifying an attributable cause of events (Figures 45-2 and 45-3).25–27 Previously, up to 40% of patients with recurrent syncope remained undiagnosed, despite extensive investigation, particularly older patients, who have marginal cognitive impairment and for whom a witnessed account of events is often unavailable. More recently, diagnostic yield for all ages has improved with the application of guidelines.28 Although diagnostic investigations are available, the high frequency of unidentified causes in clinical studies may occur because patients failed to recall important diagnostic details,14,29 because of the stringent diagnostic criteria used in clinical studies or, probably most often, because the syncopal episode resulted from a combination of chronic and acute factors rather than from a single obvious disease process.22 A multifactorial cause likely explains most cases of syncope in older adults who are predisposed because of multiple chronic diseases and medication effects superimposed on the age-related physiologic changes described earlier.30 Common factors that in combination may predispose to or precipitate syncope include anemia, chronic lung disease, chronic heart failure, and dehydration. Medications that may contribute to or cause syncope are listed in Table 45-2. Common causes of syncope are listed in Box 45-1. The most frequent individual causes of syncope in older patients are neurally mediated syndromes, including CSS, orthostatic hypotension, and postprandial hypotension, as well as arrhythmias, including tachyarrhythmias and bradyarrhythmias. These disease processes are described in the next section. Disorders that may be confused with syncope and that may or may not be associated with loss of consciousness are listed in Table 45-3. TABLE 45-3 Differential Diagnosis of Syncope in the Older Adults Metabolic disorders, including hypoglycemia, hypoxia, hyperventilation with hypocapnia Vertebrobasilar TIA Drop attacks Falls TIA (anterior circulation) Manifestations in this age group are challenging, and often recognition is the first step to optimizing management and care of these patients. To start with, syncope in the older patient is underrecognized, particularly in acute-care settings, because the presentation is frequently atypical. The older patient is less likely to have a warning or prodrome prior to syncope, commonly has amnesia for loss of consciousness, and frequently experiences an unwitnessed event,12 thus presenting with a fall rather than TLOC.14,22,31 These events are typically described as nonaccidental (not a trip or slip) or unexplained falls. Therefore, history alone cannot be relied on when assessing the older patient. Injurious events such as fractures and head injuries are also more common, further emphasizing the importance of thorough early investigation and diagnosis.32 The underlying mechanism of syncope is transient cerebral hypoperfusion. In some forms of syncope, there may be a premonitory period in which various symptoms (e.g., lightheadedness, nausea, sweating, weakness, visual disturbances) warn of an impending syncopal event.33 Often, however, loss of consciousness occurs without warning or recall of warning.14,29 Recovery from syncope is usually accompanied by almost immediate restoration of appropriate behavior and orientation. Amnesia for loss of consciousness occurs in many older adults and in those with cognitive impairment. The postrecovery period may be associated with fatigue of varying duration. In younger patients, nausea, blurred vision, and sweating predict noncardiac syncope, but only dyspnea predicts cardiac syncope in older patients.33 Syncope and falls are often considered two separate entities with different causes. Recent evidence suggests, however, that these conditions may not always be distinctly separate.34 In older adults, determining whether patients who have fallen have had a syncopal event can be difficult. At least half of syncopal episodes are unwitnessed, and older patients may have amnesia for loss of consciousness.14 Amnesia for loss of consciousness has been observed in 30% of patients with CSS who present with falls and 25% of all patients with CSS, irrespective of presentation.35 Emerging evidence has suggests a high incidence of falls in addition to traditional syncopal symptoms in older patients with sick sinus syndrome and atrioventricular conduction disorders. Thus, syncope and falls may be indistinguishable and may, in some cases, be manifestations of similar pathophysiologic processes. Specific causes of syncope are presented in the following sections.36 The initial step in the evaluation of syncope is to consider whether there is a specific cardiac or neurologic cause or whether the cause is likely multifactorial.1,37,38 The starting point for the evaluation of syncope is a careful history and physical examination. A witness account of events is important to ascertain, when possible.39,40 Three key questions should be addressed during the initial evaluation: Differentiating true syncope from other nonsyncopal conditions associated with real or apparent loss of consciousness is generally the first diagnostic challenge and influences the subsequent diagnostic strategy. A strategy for differentiating true syncope and nonsyncope is outlined in Figures 45-4 and 45-5. The presence of heart disease is an independent predictor of a cardiac cause of syncope, with a high sensitivity of 95% but a low specificity of 45%.41 Patients frequently complain of dizziness alone or as a prodrome to syncope and unexplained falls. Four categories of dizzy symptoms—vertigo, dysequilibrium, lightheadedness, and others—have been recognized. The categories have neither sensitivity nor specificity in older, as in younger, patients. Dizziness, however, may more likely be attributable to a cardiovascular diagnosis if associated with pallor, syncope, prolonged standing, palpitations, or the need to lie down or sit down when symptoms occur. Initial evaluation may lead to a diagnosis based on symptoms, signs, or electrocardiographic findings. Under such circumstances, no further evaluation is needed and treatment, if any, can be planned. More commonly, the initial evaluation leads to a suspected diagnosis (see Figure 45-3), which needs to be confirmed by directed testing.3,42 If a diagnosis is confirmed by specific testing, treatment may be initiated. On the other hand, if the diagnosis is not confirmed, patients are considered to have unexplained syncope and should be evaluated following a strategy such as that outlined in Figure 45-5. It is important to attribute a diagnosis, if possible, rather than assume that an abnormality known to produce syncope or hypotensive symptoms is the cause. To reach a diagnosis, patients should have symptom reproduction during investigation and preferably alleviation of symptoms with specific intervention. It is not uncommon for more than one predisposing disorder to coexist in older patients, rendering a precise diagnosis difficult. In older adults, treatment of possible causes without clear verification of an attributable diagnosis may often be the only option. An important issue in patients with unexplained syncope is the presence of structural heart disease or an abnormal electrocardiogram (ECG). These findings are associated with a higher risk of arrhythmias and a higher mortality at 1 year.43 In these patients, cardiac evaluation, consisting of echocardiography, stress testing, and tests for arrhythmia detection (e.g., prolonged electrocardiographic and loop monitoring, electrophysiologic study) are recommended. The most alarming electrocardiographic sign in a patient with syncope is probably alternating complete left and right bundle branch block or alternating right bundle branch block with left anterior or posterior fascicular block, suggesting trifascicular conduction system disease and intermittent or impending high-degree atrioventricular (AV) block. Patients with bifascicular block (right bundle branch block plus left anterior or left posterior fascicular block, or left bundle branch block) are also at high risk of developing high degree AV block. A significant problem in the evaluation of syncope and bifascicular block is the transient nature of high-degree AV block and, therefore, the long periods required to document it by electrocardiography. In patients without structural heart disease and a normal ECG, evaluation for neurally mediated syncope should be considered. The tests for neurally mediated syncope consist of tilt testing and carotid sinus massage. The presentation, evaluation, and management of other common causes of syncope are presented in the following sections. These may occur as the sole cause of a syncopal episode or as one of multiple contributing causes. Orthostatic or postural hypotension is arbitrarily defined as a 20-mm Hg fall in systolic blood pressure or a 10-mm Hg fall in diastolic blood pressure on assuming an upright posture from a supine position. Orthostatic hypotension implies abnormal blood pressure homeostasis and is a frequent observation in older adults. Prevalence of orthostatic hypotension varies between 4% and 33% among community-living older persons depending on the method used. Higher prevalence and larger falls in systolic blood pressure have been reported with increasing age and often signify general physical frailty. Prevalence of OH in older community-dwelling adults is 30%44 and increases to more than 50% in geriatric ward patients,45 making its diagnosis highly relevant. Orthostatic hypotension is an important cause of syncope, accounting for 14% of all diagnosed cases in a large series. In a tertiary referral clinic dealing with unexplained syncope, dizziness, and falls, 32% of patients older than 65 years had orthostatic hypotension as a possible attributable cause of symptoms. A recent population-based study that used beat-to-beat measurement of orthostatic blood pressure has demonstrated a significant age gradient for orthostatic blood pressure; in 7% of 50- to 55-year-olds systolic and diastolic blood pressures failed to stabilize by 2 minutes after standing compared with 41% of those 80 year of age and older.46 Failure of stabilization was associated with falls, depression, and global cognitive impairment.46–49 The heart rate and blood pressure responses to orthostasis occur in three phases: (1) an initial heart rate rise and blood pressure drop; (2) an early phase of stabilization; and (3) a phase of prolonged standing. All three phases are influenced by aging. The maximum rise in heart rate and the ratio between the maximum and minimum heart rates in the initial phase decline with age, implying a relatively fixed heart rate, irrespective of posture. Despite a blunted heart rate response, blood pressure and cardiac output are adequately maintained on standing in active, healthy, well-hydrated and normotensive older adults because of decreased vasodilation and reduced venous pooling during the initial phases and increased peripheral vascular resistance after prolonged standing. However, in older adults with hypertension and cardiovascular disease who are receiving vasoactive drugs, these circulatory adjustments to orthostatic stress are disturbed, rendering them vulnerable to postural hypotension.50 More recent research has suggested that the velocity of the initial orthostatic heart rate response at 10 and 20 seconds predicts mortality and morbidity.51 This age-related gradient may reflect autonomic dysfunction, increased arterial stiffness, and muscle pump defects.52 Traditionally, orthostatic hypotension is defined as a reduction in systolic blood pressure (BP) of at least 20 mm Hg or in diastolic BP of at least 10 mm Hg within 3 minutes of standing 53 Orthostatic intolerance refers to symptoms and signs with an upright posture due to circulatory abnormality.1 Syndromes of orthostatic intolerance that may cause syncope include the following: initial orthostatic hypotension, during which symptoms of lightheadedness and dizziness or visual disturbance are experienced seconds after standing; classic orthostatic hypotension, during which dizziness, presyncope, fatigue, weakness, palpitations, and visual and hearing disturbances are experienced; delayed orthostatic hypotension, during which there is a prolonged prodrome, frequently followed by rapid syncope; delayed orthostatic hypotension and reflex syncope, during which a prolonged prodrome is always followed by syncope; reflex syncope triggered by standing, during which there is a classic prodrome and triggers, always followed by syncope; and postural orthostatic tachycardia syndrome, during which there is symptomatic heart rate (HR) increases and instability of BP without syncope.1 Many older patients with orthostatic hypotension also have postprandial hypotension. Causes of orthostatic hypotension include volume depletion or disturbance of the autonomic nervous system, resulting in failure in the vasoconstrictor compensatory mechanisms induced by an upright posture.54 Hypertension further increases the risk of hypotension by impairing baroreflex sensitivity and reducing ventricular compliance. Hypertension increases the risk of cerebral ischemia from sudden declines in blood pressure. Older adults with hypertension are more vulnerable to cerebral ischemic symptoms, even with modest and short-term postural hypotension, because the threshold for cerebral autoregulation is altered by prolonged BP elevation. In addition, antihypertensive agents impair cardiovascular reflexes and further increase the risk of orthostatic hypotension.55,56 Drugs are important causes of orthostatic hypotension (see Table 45-2). Ideally, establishing a causal relationship between a drug and orthostatic hypotension requires identification of the culprit medicine, abolition of symptoms by withdrawal of the drug, and rechallenge with the drug to reproduce symptoms and signs. Rechallenge is often omitted in clinical practice in view of the potential serious consequences. In the presence of polypharmacy, which is common in older adults, it becomes difficult to identify a single culprit drug because of the synergistic effect of different drugs and drug interactions. Thus, all drugs should be considered as possible contributors to orthostasis.57,58 A number of non-neurogenic conditions are also associated with postural hypotension. These conditions include myocarditis, atrial myxoma, aortic stenosis,59 constrictive pericarditis, hemorrhage, diarrhea, vomiting, ileostomy, burns, hemodialysis, salt-losing nephropathy, diabetes insipidus, adrenal insufficiency, fever, and extensive varicose veins. Volume depletion for any reason is a common sole or contributing cause of postural hypotension and, in turn, syncope. There are three distinct clinical autonomic syndromes associated with orthostatic hypotension—pure autonomic failure (PAF), multiple system atrophy (MSA), or Shy-Drager syndrome (SDS)—and autonomic failure associated with idiopathic Parkinson disease (IPD). PAF, the least common condition and a relatively benign entity, was previously known as idiopathic orthostatic hypotension. This condition presents with orthostatic hypotension, defective sweating, impotence, and bowel disturbances. No other neurologic deficits are evident, and resting plasma epinephrine levels are low. MSA is the most common of these and has the poorest prognosis. Clinical manifestations include features of dysautonomia and motor disturbances due to striatonigral degeneration, cerebellar atrophy, or pyramidal lesions. Additional neurologic deficits include muscle atrophy, distal sensorimotor neuropathy, pupillary abnormalities, restriction of ocular movements, disturbances in rhythm and control of breathing, life-threatening laryngeal stridor, and bladder disturbances. Psychiatric manifestations and cognitive defects are usually absent. Resting plasma epinephrine levels are usually within the normal range but fail to rise on standing or tilting. The prevalence of orthostatic hypotension in Parkinson disease (PD) rises with advancing years and with the number of medications prescribed. Cognitive impairment, in particular abnormal attention and executive function, is more common in PD with orthostatic hypotension, suggesting a possible causal association with hypotension, including watershed hypoperfusion and infarction. Orthostatic hypotension in PD can also be due to autonomic failure and/or to side effects of antiparkinson medications.
Syncope
Introduction
Definition
Epidemiology
Pathophysiology
Causes of Syncope in Older Adults
Multifactorial Causes.
Individual Causes.
Conditions With LOC or Partial LOC
Conditions Without LOC
Epilepsy
Cataplexy
Intoxication (e.g., alcohol, medication overdose [sedatives, analgesics])
Presentation
Evaluation
Orthostatic Hypotension
Pathophysiology
Causative Factors
Aging
Medications
Other Conditions
Association With Primary Autonomic Failure Syndromes
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Syncope
45