Chapter 9
Syncope
Introduction
Definition
Syncope is a temporary loss of consciousness due to transient global cerebral hypoperfusion, characterised by rapid onset, short duration and spontaneous complete recovery (1).
Background
Syncopal events account for approximately 3% of ED visits and up to 6% of hospital admissions (2). Up to 25% of syncopal events in older people present as unexplained falls, and the morbidity and mortality of syncope in older patients is greater than in the general population due to the higher frequency of resulting trauma such as fractures or significant head injuries (2). Syncope in geriatric patients can be a complex phenomenon: younger patients tend to develop syncope due to a single cause, whereas geriatric patients often experience multifactorial syncope (3, 4). In addition to this, there is significant overlap between falls, syncope and other disorders of consciousness; many patients, both with and without cognitive impairment, will have difficulty detailing the exact events surrounding their presentation.
Why are older patients pre-disposed to syncope?
A number of physiological changes, particularly to the autonomic nervous system, predispose older patients to syncope (4):
- Reduction in β-adrenergic vasodilatory response
- Reduction in α-adrenergic vasoconstrictive responses
- Decreased β-adrenergic–mediated cardioacceleratory response to sympathetic activation
- Reduced parasympathetic tone leading to reduced heart rate variability
- Decreased baro-reflex sensitivity leading to reduced heart rate augmentation with low blood pressure
- Reduced numbers of sinoatrial cells
- Increased rate of salt and water loss by the kidneys
- Reduced thirst response
Types of syncope in the older population
Neurally mediated syncope, otherwise termed reflex syncope, remains the commonest cause of syncope in older patients; however, proportionally, older patients have higher rates of orthostatic hypotension, arrhythmias and structural cardiac causes (5). The cause of syncope in older patients is not always clear, and in studies of older patients presenting with and being investigated for syncope, between 10.4% and 47.5% remained undiagnosed (6) (Figure 9.1).
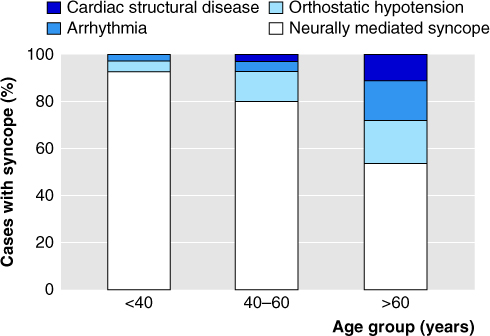
Figure 9.1 Causes of syncope by age.
Source: From Parry SW, Tan MP. An approach to the evaluation and management of syncope in adults. BMJ. 2010 Feb 19;340(feb19 1):c880–c880.
History
History-taking provides the diagnosis in 50% of cases where the cause of syncope can be established (7).
It is important to ask about specific triggers and associated symptoms before, during and after the event. A general systems enquiry may identify potential causes of decreased intravascular volume, such as diarrhoea, vomiting or internal and external haemorrhage (Table 9.1).
Table 9.1 Types of syncope with associated triggers and symptoms (1, 2, 8)
| Types | Triggers | Associated features |
| Reflex/neurally mediated Neurocardiogenic (vasovagal) | Orthostatic stress/emotional distress/pain/noxious stimuli | Prodrome of
|
| Situational |
| |
| Carotid sinus | ||
| Cardioinhibitory Vasodepressive | Activities involving pressure over the neck: e.g. shaving/head turning/tight collar | |
| Orthostatic hypotension | Rapid postural change Hypovolaemia Haemorrhage Medication induced: particularly recent dose changes or new drugs | Typical prodrome with documented blood pressure drop |
| Cardiac | ||
| Electrical | Tachyarrythmias/bradyarrythmias/AV blocks | Lack of prodrome should raise suspicion of cardiac cause Abnormal ECG Chest pain, palpitations, SOB, sweating |
| Structural | Valvular disease/MI/Cardiomyopathy/pulmonary hypertension/tumour | |
| Neurological | ||
| Posterior circulation stroke | No trigger | Dysarthria, diplopia, vertigo, nausea |
| Subclavian steal | Activities involving arms being raised for prolonged time: painting, hair combing etc | |
| SAH | No trigger | Headache |
| Rare causes | Pulmonary embolism/Hyperventilation/Psychiatric | Associated symptoms depend on underlying cause |
SOB, shortness of breath.
Conditions that may be mistaken for syncope, e.g. causing loss of consciousness or loss of postural tone or both but in the absence of cerebral hypoperfusion, include (but are not limited to) the following (1):
- Epilepsy
- Metabolic disturbance, e.g. hypoglycaemia
- Cataplexy
- Drop attacks
- Psychogenic or functional causes
- Falls
Examination
General examination
General aspects of the examination should include skin and mucous membrane assessment for hydration status, consideration of rectal examination to check for melaena, a search for evidence of sepsis and focal infection and any signs of traumatic injury sustained during the collapse.
Examination can identify the cause of syncope in 20% of cases where the cause can be established (7). However, patients presenting with syncope can have a normal examination even with a potentially life-threatening cause for their collapse.
Specific areas of focus on examination
Cardiovascular
Look for jugular venous distension or other signs of cardiac failure, listen for heart murmurs and bruits and feel for the cardiac apex, central and peripheral pulses and note their rate, rhythm and character, and check for signs of abdominal aortic aneurysm (AAA).
Neurological
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








