Surgical Management of Metastatic Bone Disease: Pelvic Lesions
Jacob Bickels
Martin M. Malawer
BACKGROUND
Metastatic tumors of the pelvis may cause pain and a major loss of function and weight-bearing capacity. Because of the relatively large size of the pelvic cavity and the elastic nature of the organs it contains and its surrounding muscles, tumors at that site usually reach considerable size before causing symptoms.
Although some locations of these metastases within the pelvis have no impact on pelvic stability and function (eg, ilium, pubis), tumors of the posterior ilium may pose a threat to lumbosacral integrity, and tumors of the acetabulum may profoundly impair hip function and the weightbearing capacity of the lower extremity.
Both primary sarcomas and metastatic tumors usually present with considerable extension into the soft tissues. Because of their inherent sensitivity to radiation therapy, however, the surgical management of metastatic lesions does not require en bloc resection of overlying muscles, and microscopic residua are treated with adjuvant radiation. The complex anatomy of the pelvic girdle mandates detailed preoperative imaging, planning of exposure and reconstruction technique, and careful and meticulous execution of the surgical procedure.
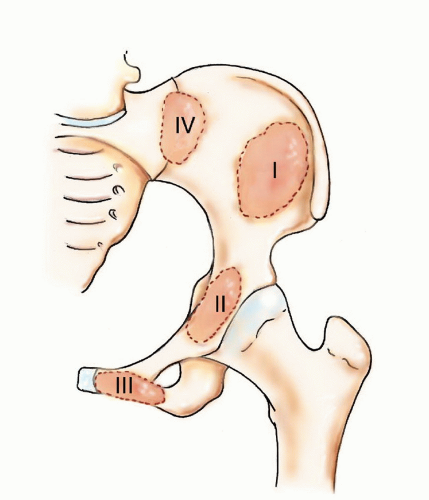
FIG 1 • Metastatic tumors of the ilium, periacetabular region, pubis, and posterior ilium require types I, II, III, and IV pelvic resections, respectively.
Pelvic metastases are treated with either curettage and reconstruction with cemented hardware or by wide resections. These procedures are grouped together and termed pelvic resections, the classification of which is attributed to Enneking and is based on the resected region of the innominate bone:
Type I—ilium
Type II—periacetabular region
Type III—pubis
ANATOMY
Ilium
The iliac crest is the attachment site for abdominal wall musculature and quadratus lumborum (FIG 2).
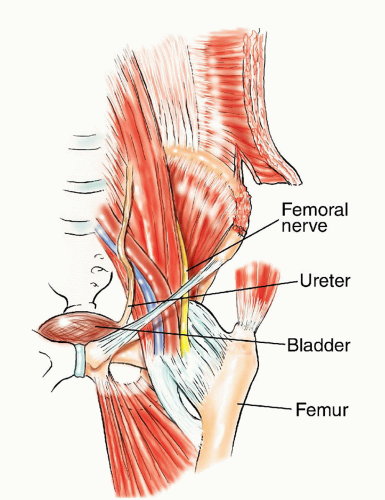
The iliacus muscle overlies the inner iliac table and the femoral nerve lies medial to it in the groove between the iliacus and the psoas muscle.
Gluteal muscles overlie the outer iliac table.
Acetabulum
The upper medial mechanical support of the hip joint
No muscle attachments
Pubis
Origin of hip adductors from its inferior aspect
The neurovascular bundle runs along the anterior aspect of the pubis.
The urinary bladder attaches to its posterior wall.
INDICATIONS
Pathologic fracture of the acetabulum
Impending pathologic fractures of the acetabulum, which are defined as lesions that extend to the acetabular roof and are associated with cortical destruction and considerable pain on weight bearing
Intractable pain associated with locally progressive disease that had shown inadequate response to narcotics and preoperative radiation therapy
Solitary bone metastasis in selected patients
IMAGING AND OTHER STAGING STUDIES
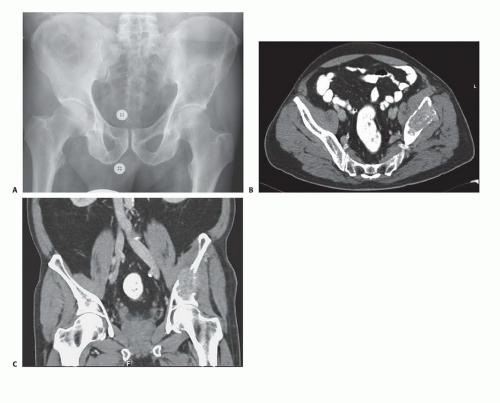
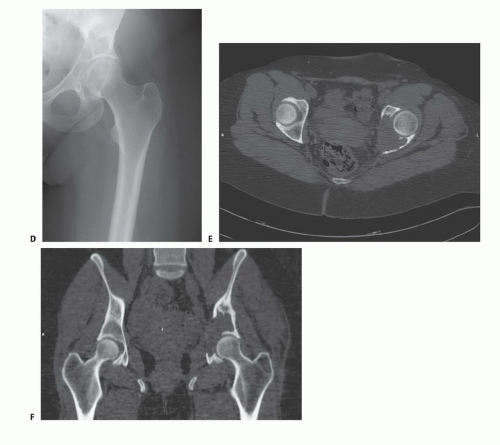
Plain radiographs and computed tomography of the pelvis and hip joints are mandatory to evaluate the full extent of bone destruction, soft tissue extension, and integrity of the hip joint. Magnetic resonance imaging rarely adds additional information: It is indicated in lesions which have diffused intramedullary extension that is commonly underestimated by computed tomography, such as multiple myeloma. Total body bone scintigraphy is done for detecting synchronous metastases elsewhere in the skeleton. At the conclusion of imaging, the surgeon should be able to answer the following questions:
What is the full extent of bone destruction and soft tissue extension that are related to the tumor? Is the lesion an impending fracture? If not, it should probably be treated nonsurgically.
What incision should be used to obtain optimal exposure (FIG 3)?
What would be the best technique for resection and reconstruction, if required?
Are there additional skeletal metastases and, if so, can they be managed by nonoperative techniques or do they require surgery?
SURGICAL MANAGEMENT
Positioning
Types I, II, and III resection: The patient is placed supine on the operating table with a slight elevation of the ipsilateral hip.
Type IV resection: The patient is placed in a true lateral position with the affected side of the pelvic girdle uppermost. The operating table is bent with the breakage point just below the contralateral hip: Such a position widens the space between the iliac crest and the lower aspect of the chest wall, allowing a comfortable approach and easier maneuvering at that site (FIG 4).
Approach
The most useful approach to pelvic resections is the utilitarian pelvic incision. All or part of the incision can be used for adequate exploration and resection of pelvic girdle metastases.
The incision begins at the posterior inferior iliac spine and extends along the iliac crest to the anterior superior iliac spine. It is then separated into two arms: One extends along the inguinal ligament up to the symphysis pubis, and the other turns distally over the anterior thigh for one-third the length of the thigh and then curves laterally just posterior to the shaft of the femur below the greater trochanter and follows the insertion of the gluteus maximus muscle.
Reflection of the posterior gluteus maximus flap exposes the proximal third of the femur, the sciatic notch, the sacrotuberous and sacrospinous ligaments, the origin of the hamstrings from the ischium, the lateral margin of the sacrum, and the entire buttock (FIG 5A).
Posteriorly, the incision extends along the posterior iliac crest, posterior superior iliac spine, and ipsilateral hemisacrum (FIG 5B).
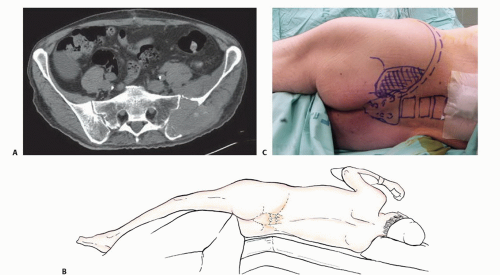 FIG 4 • A. Metastatic carcinoma of the posterior ilium. B,C. The patient is placed in a true lateral position and the operating table is broken at the hip level to allow easier access to the flank. |
TECHNIQUES
▪ Exposure
Type I Resection
The middle component of the utilitarian incision is used to expose the iliac crest. Using electrocautery, the glutei are detached and reflected from the outer iliac table. The iliacus muscle is similarly detached and reflected from the inner table (TECH FIG 1).
Type II Resection
Lesions with lateral cortical destruction
The middle component of the utilitarian incision up to the anterior superior iliac spine with a 5-cm extension along the lateral thigh arm of the incision is used for these lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree