Surgical Management of Metastatic Bone Disease: General Considerations
Jacob Bickels
Martin M. Malawer
BACKGROUND
The skeleton, after the lungs and liver, is the third most common site of metastatic disease.4,11 Prostate, breast, lung, kidney, and thyroid cancers account for 80% of skeletal metastases.4,11 The prolonged survival with disease of more cancer patients has led to continuously growing numbers of patients with metastatic bone disease (MBD). The exact incidence of bone metastases is unknown, but it is estimated that in the United States alone, 350,000 people die with bone metastases from primary carcinomas.13
MBD is a major factor contributing to deterioration of the quality of life in patients with cancer. These patients may require surgical intervention for the management of impending or present pathologic fracture or for the alleviation of intractable pain associated with a locally progressive lesion. Those skeletal crises are associated with a considerable loss of function, pain, and the associated impairment of quality of life. Surgery may also be performed to remove a solitary bone metastasis with the intent of improving long-term survival in selected patients,1,9 but other than this rare exception, these surgical interventions are mainly palliative and aimed at achieving local tumor control, structural stability of the surgically treated site, and restoration of normal function as quickly as possible. Failure to achieve one of these goals usually necessitates a second surgical intervention, and this is associated with additional impairment of an already compromised quality of life. Reports show failure rates of surgeries done for MBD as high as 40% and occurring as the result of a poor initial fixation, improper implant selection, and progression of disease in the operative field.3,8,14,15
An attempt to treat a pathologic fracture as one would treat a traumatic fracture will fail in most cases because the underlying disease impedes the fracture healing process. The prognosis for union of a pathologic fracture is also determined to some extent by the tumor type: Those associated with metastatic adenocarcinomas of breast and prostate, multiple myeloma, and lymphoma successfully unite far more frequently than do those associated with malignancies of the lung, kidney, and gastrointestinal tract.5,6,7 Even when healing does occur, it does so after an unreasonably long period of time and is of a less than satisfactory quality. Reduction and immobilization used in the management of traumatic fractures are, therefore, not applicable in the management of pathologic fractures due to MBD.
Gainor and Buchert5 analyzed 129 pathologic fractures and found that the long bone fractures that healed most predictably were those which had been internally fixed and irradiated and were in patients who survived for more than 6 months postoperatively. Similar observations were made by Harrington et al.7
Cemented hardware or prostheses are preferentially used for fixation to achieve immediate stability, and reconstruction techniques that rely on a biologic process of bone healing (such as autologous bone grafts, allografts, or allografts prosthetic composites) are inappropriate for the surgical management of MBD.2,6,7,10
INDICATIONS
Existing pathologic fracture
Impending pathologic fracture
Intractable pain associated with locally progressive disease that had shown inadequate response to narcotics and preoperative radiation therapy
Solitary bone metastasis in selected tumor types
It is agreed that surgical intervention for MBD is appropriate for patients who are expected to survive longer than 3 months. Patients who are expected to survive less than 3 months are less likely to benefit from an operation because they usually do not have the physical strength required for rehabilitation or the time needed for its completion. Those patients are treated with nonoperative approaches, such as sling and arm brace for the upper extremities or protected weight bearing for the lower extremities.
PREOPERATIVE EVALUATION
Although planned surgery for patients with MBD should not be delayed, preoperative evaluation and staging must not be compromised but rather thoroughly mapped out. This evaluation allows the understanding of the morphology of the lesion and its relation to adjacent structures, determining the overall skeletal staging of the patient, and detecting any other metastases that may require simultaneous surgery.
Because most patients who present with skeletal metastases have an established diagnosis of cancer, clinical and radiologic evaluations are usually aimed at evaluating the extent of the disease and the presence of its complications rather than at identifying its site of origin.
Patient History and Physical Findings
Medical history should include current oncologic status and related treatments and medications. It is crucial to question the patient and/or family members about his or her overall functional status and, specifically, about the status of the
affected extremity prior to the occurrence of the metastatic lesion.
For example, a surgeon would be justifiably reluctant to perform major surgery on a lower extremity in a patient who was bedridden or wheelchair-bound, given that stabilization of the extremity for greater ease in maintaining pain-free personal hygiene in that patient would require a less extensive procedure. The orthopaedic surgeon should also inform the responsible medical oncologist of the impending operation, verify the oncologic information given to him or her, and be provided with the patient’s estimated life expectancy.
The physical examination should include evaluation of the principal symptomatic area as well as other symptomatic sites. Examination should focus on the extent of soft tissue tumor extension and its relation to the neurovascular bundle of the extremity, muscle strength and range of motion of the adjacent joints, neurovascular status of the affected extremity, and limb edema.
Laboratory Studies
A complete blood count and blood chemistries should be ordered. Of specific concern in those studies is the calcium level because hypercalcemia may be a life-threatening complication of MBD. Acquiring an ionized calcium level is helpful in the diagnosis of hypercalcemia because low albumin levels may lower total calcium levels. Hypercalcemia should be treated prior to any surgical intervention. Levels of specific tumor markers should be evaluated if applicable to the specific tumor type.
Imaging Studies
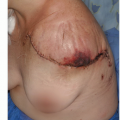
Plain radiographs and computed tomography (CT) of the affected site should be done as well as plain radiographs of any additional site in which the patient reports of a joint or bone pain. The combined results of these studies will define the extent of bone destruction and soft tissue extension (FIG 1). If the investigated metastasis is located in a long bone, plain radiographs of reasonable quality of its entire extent should also be done to exclude additional metastases because these data are crucial for surgical planning: Missed metastases could cause pathologic fractures upon weight bearing postoperatively and require an extensive surgery for their repair (FIG 2).

FIG 1 • A. Plain radiograph showing a metastatic tumor of the right acetabulum in a 72-year-old male with a known history of thyroid carcinoma. B. CT scan shows an extensive bone destruction and soft tissue extension. Attempt at resection based on the radiographic findings alone would probably result in intralesional debulking and potential exsanguination due to the extensive vascularity of this tumor. Given these radiologic findings, this patient underwent preoperative angiographic embolization that diminished blood loss in surgery and allowed successful resection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access