Surgical Management of Metastatic Bone Disease: Femoral Lesions
Jacob Bickels
Martin M. Malawer
BACKGROUND
The femur is the most common site for metastatic bone disease requiring surgery. Because it is a major weight-bearing bone with minimal space for surgical errors, the operative procedure must be carefully planned and meticulously executed, with the aim of achieving durable reconstruction. Detailed preoperative clinical and imaging evaluation is essential to define the morphologic characteristics of the lesion that validate surgical intervention and to distinguish between lesions that can be managed with curettage and cemented fixation and those that require resection with endoprosthetic reconstruction.1,6,7
Unlike primary sarcomas of the femur, metastatic tumors usually have a small soft tissue component, even in the presence of extensive bone destruction. This feature allows the sparing of extracortical structures, such as the joint capsule, overlying muscles, and muscle attachments, and the possibility of applying them for reconstruction and preservation of function.
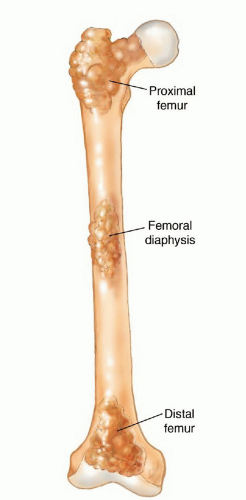
Because of distinctive differences in anatomic and surgical considerations, surgeries around the proximal femur, femoral diaphysis, and distal femur will be discussed separately (FIG 1).
ANATOMY
Proximal Femur
A thick joint capsule encircles the femoral head and neck and attaches to the base of the neck.
Key elements at the lateral aspect: The greater trochanter is the insertion site for the gluteus medius muscle (lateral stabilizer and hip abductor) and the origin for the vastus lateralis muscle.
Key elements at the medial aspect: The minor trochanter is the insertion site for the psoas muscle (medial stabilizer and hip flexor).
Femoral Diaphysis
The femoral diaphysis is encircled by two muscle layers:
First layer: the vastus intermedius muscle
Second layer: The rectus femoris and vastus medialis muscles intersect at the anteromedial aspect, and the rectus femoris and the vastus lateralis muscles intersect at the anterolateral aspect.
Distal Femur
The medial femoral condyle is positioned below the insertion site of the vastus medialis muscle.
The lateral femoral condyle is positioned below the insertion site of the vastus lateralis muscle.
INDICATIONS
Pathologic fracture
Impending pathologic fracture
Intractable pain associated with locally progressive disease that has shown inadequate response to narcotics and radiation therapy
Solitary bone metastasis in selected patients and tumor types (eg, those with breast cancer and renal cell carcinoma)
IMAGING AND OTHER STAGING STUDIES
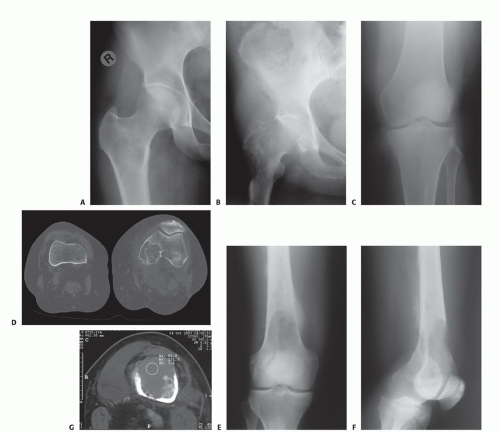
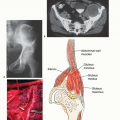
Plain radiographs of the entire femur are mandatory to rule out coexisting metastases that may influence the extent and technique of surgery. Computed tomography
of the lesion will clearly define the extents of soft tissue component and bone destruction. Total body bone scintigraphy is done to detect coexisting metastases elsewhere in the skeleton (FIG 2). The results of imaging should provide the surgeon with answers to the following questions:
Is the lesion an impending fracture? (If not, it should probably be treated nonoperatively.)
Are there additional femoral metastases? If so, can they be managed by nonoperative techniques or do they also require surgery?
What is the appropriate surgical approach? As a rule, tumor curettage with cemented fixation is indicated for lesions in which the remaining cortices allow containment of the fixation device. Otherwise, surgery consists of resection of the affected bone segment with prosthetic reconstruction.
TECHNIQUES
▪ Proximal Femur
Position and Incision
The patient is placed supine on the operating table, with the buttock of the affected side close to its edge. The operating table is positioned in a 30-degree tilt away from the surgeon.
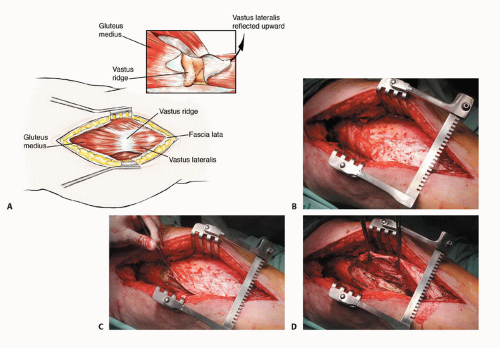
A straight longitudinal incision is made along the tip of the greater trochanter and femoral diaphysis (TECH FIG 1). It should begin 5 cm proximal to the greater trochanter to allow the introduction of a femoral nail and 5 cm below the lower edge of the lesion to enable adequate tumor curettage.
Exposure
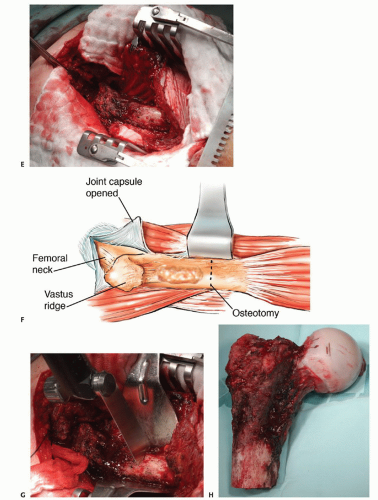
The fascia lata is divided longitudinally and retracted to expose the lower edge of the gluteus medius muscle and its insertion site at the greater trochanter muscle, the vastus ridge, and the upper part of the vastus lateralis muscle (TECH FIG 2A,B).
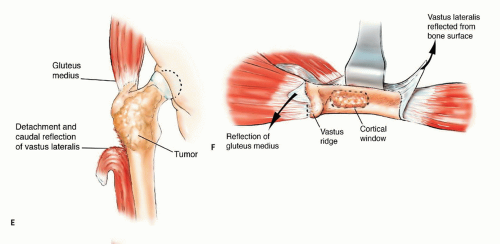
Using electrocautery, the vastus lateralis muscle is detached from the vastus ridge and the lower aspect of the proximal diaphysis and reflected anteriorly to expose the diaphyseal cortex (TECH FIG 2C-E). A longitudinal cortical window with oval edges is made below the vastus ridge (TECH FIG 2F).
Tumor Removal
Gross tumor is removed with hand curettes (TECH FIG 3A,B). Curettage should be meticulous and should leave only microscopic disease in the tumor cavity. It is followed by high-speed burr drilling of walls of the tumor cavity (TECH FIG 3C,D).
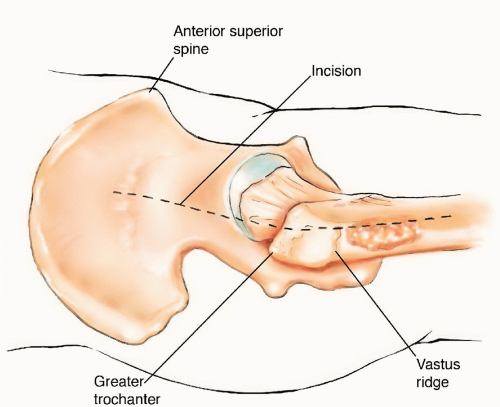
TECH FIG 1 • A straight longitudinal incision is made along the tip of the greater trochanter and femoral diaphysis.
When a proximal femur resection is done, the gluteus medius muscle is detached and reflected from its insertion site at the greater trochanter muscle (TECH FIG 3E), the joint capsule is opened and the femoral head is dislocated from the acetabulum, the medial aspect of the proximal femur is freed of muscle attachments, and then an osteotomy is performed below the lower aspect of the tumor (TECH FIG 3F-H).
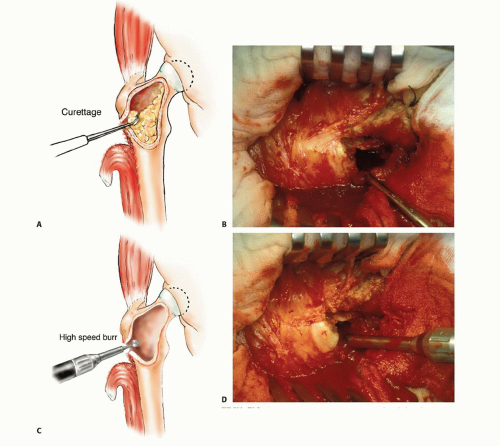 TECH FIG 3 • A,B. Gross tumor is removed with hand curettes. C,D. Curettage is followed by high-speed burr drilling of the walls of the tumor cavity. (continued) |
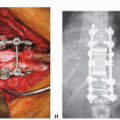
Mechanical Reconstruction
Reconstruction begins with the introduction of an intramedullary nail. After proper positioning and length are verified, the nail is partially withdrawn and the entire tumor cavity is filled with cement (TECH FIG 4A). The nail is then pushed back into the medullary canal and fixed with interlocking screws (TECH FIG 4B,C). Alternatively, a side plate and a sliding screw can be similarly used for reconstruction. After resection of the proximal femur, a cemented tumor prosthesis is used to reconstruct the bone defect (TECH FIG 4D).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree