Adrenocortical carcinoma frequently presents with sequelae of steroid precursor overproduction and has a proclivity for aggressive local growth, early metastasis, and recurrence. En bloc surgical resection with negative margins is the cornerstone of therapy for localized disease, and re-resection has a role in selected recurrent cases. Presence of occult micrometastatic disease at the time of presentation is confirmed by frequent distant failure after apparent negative margin resection. Data for many aspects of therapy are limited or nonexistent. This review critically considers existing evidence with a particular focus on surgical management.
Key points
- •
Adrenocortical carcinoma is an aggressive malignancy; prognosis is determined by tumor stage at presentation and completeness of surgical resection.
- •
Complete resection with negative margins is the goal of surgical management and may require multivisceral resection, tumor thrombectomy, or vascular resection with or without reconstruction.
- •
Extended resection including adjacent organs not obviously involved by tumor is not indicated. Regional lymphadenectomy may provide valuable staging information or be associated with a disease-free or overall survival advantage and is underutilized.
- •
Minimally invasive approaches have been advocated by select centers with expertise; notwithstanding, likely malignant and locally advanced lesions in particular are most safely managed with an open approach.
- •
Recurrence is associated with a poor prognosis; however, selected patients with limited or symptomatic disease may benefit from aggressive surgery.
Introduction
Adrenocortical carcinoma (ACC) is a rare malignancy with an annual incidence of 1 to 2 cases per million individuals. Notwithstanding, frequent presentation with sequelae of steroid precursor overproduction, proclivity for aggressive local growth, early metastasis and recurrence, and the scarcity of effective systemic treatment options contribute to a substantial burden of disease. Women are more affected than men, at a ratio of 1.5:1. Although ACC affects individuals of all ages, cases are clustered in early childhood or middle age. Most cases are seemingly sporadic; however, ACC may arise in association with hereditary syndromes, including multiple endocrine neoplasia-1 and Li-Fraumeni syndrome. Overall prognosis is poor; estimates of 5-year survival range from 30% to 50%; metastatic disease is associated with a median survival of less than 1 year. Surgery is the cornerstone of therapy for localized disease and has a role in selected recurrent cases. Although an association between complete resection with negative margins and survival has been reproduced in numerous series, the frequent presentation with at least locally advanced disease and presence of major vascular invasion or direct invasion of discontiguous structures undermine effective surgical therapy in many cases. Moreover, presence of occult micrometastatic disease at the time of presentation is confirmed by frequent distant failure after apparent negative margin resection. Owing in part to its low incidence, data for many accepted elements of therapy are limited or nonexistent. This review critically considers the existing evidence for elements of the evaluation and treatment of patients with ACC, with a particular focus on surgical management.
Introduction
Adrenocortical carcinoma (ACC) is a rare malignancy with an annual incidence of 1 to 2 cases per million individuals. Notwithstanding, frequent presentation with sequelae of steroid precursor overproduction, proclivity for aggressive local growth, early metastasis and recurrence, and the scarcity of effective systemic treatment options contribute to a substantial burden of disease. Women are more affected than men, at a ratio of 1.5:1. Although ACC affects individuals of all ages, cases are clustered in early childhood or middle age. Most cases are seemingly sporadic; however, ACC may arise in association with hereditary syndromes, including multiple endocrine neoplasia-1 and Li-Fraumeni syndrome. Overall prognosis is poor; estimates of 5-year survival range from 30% to 50%; metastatic disease is associated with a median survival of less than 1 year. Surgery is the cornerstone of therapy for localized disease and has a role in selected recurrent cases. Although an association between complete resection with negative margins and survival has been reproduced in numerous series, the frequent presentation with at least locally advanced disease and presence of major vascular invasion or direct invasion of discontiguous structures undermine effective surgical therapy in many cases. Moreover, presence of occult micrometastatic disease at the time of presentation is confirmed by frequent distant failure after apparent negative margin resection. Owing in part to its low incidence, data for many accepted elements of therapy are limited or nonexistent. This review critically considers the existing evidence for elements of the evaluation and treatment of patients with ACC, with a particular focus on surgical management.
What is the appropriate diagnostic and imaging workup for patients with suspected adrenocortical carcinoma?
The presentation of ACC is highly variable. Smaller nonfunctional ACCs are sometimes identified incidentally. Approximately 50% to 60% of ACCs are functional and present with signs or symptoms of hormone excess. As with all tumors of the adrenal gland, directed laboratory testing and high-resolution imaging are critical and allow appropriate management. The former should include serum metanephrines to exclude pheochromocytoma. Glucocorticoid excess may be discerned through measurement of levels of serum cortisol and plasma adrenocorticotropic hormone or 24-hour free urinary cortisol; a more definitive diagnosis may require low-dose dexamethasone suppression. Levels of sex steroids and steroid precursors, including dehydroepiandrosterone sulfate (DHEA-S), 17-OH progesterone, androstenedione, testosterone, and 17-β-estradiol (in men and postmenopausal women), may be elevated in serum. Mineralocorticoid excess may be driven by glucocorticoid-mediated mineralocorticoid receptor activation in the occasional patient with hypercortisolism and is detected through measurement of the plasma aldosterone/renin ratio. Urinary steroid metabolomic profiling has emerged as a promising diagnostic tool, but it has yet to be validated in larger prospective multicenter series.
Computed tomography (CT) and MRI are similarly effective at discriminating between benign and malignant adrenal tumors and identifying metastases. The choice of one imaging study over another is largely a question of institutional preference with some caveats: (1) CT is less expensive and (2) MRI is preferable when pheochromocytoma is suspected because of the purported risk of a hypertensive crisis after intravenous infusion of iodinated CT contrast. Hounsfield units less than 10 on unenhanced CT, rapid washout at 15 minutes on delayed contrast-enhanced CT, or signal intensity loss using opposed-phase MRI are consistent with a benign tumor. ACCs are typically heterogeneous with irregular margins and irregular enhancement of solid components ( Fig. 1 ). With ACC, invasion of adjacent structures or extension into the inferior vena cava (IVC), locoregional lymph node metastases, and distant metastases may be seen. PET with fluorodeoxyglucose F 18 may have additional sensitivity in identifying metastases. Use of radiolabeled metomidate, highly specific for adrenal cortical cells via targeted binding to both 11β-hydroxylase and aldosterone synthase, for either PET- or single-photon emission CT–based functional imaging is another emerging technique with high sensitivity and specificity for ACC.
Percutaneous biopsy of a potentially resectable suspected ACC is rarely indicated. It is infrequently helpful owing to poor sensitivity and may result in complications (eg, bleeding and pneumothorax). An increased risk of biopsy site or peritoneal recurrence is often invoked but is largely unproven. In the rare circumstance when biopsy is undertaken (eg, to discriminate a metastasis from a primary adrenal malignancy or in anticipation of neoadjuvant therapy), the diagnosis of pheochromocytoma must first be excluded.
What are the pathologic determinants of malignancy? What factors are prognostic in resected adrenocortical carcinoma?
Histopathologic differentiation between benign and malignant adrenocortical tumors is often challenging. Given that the definitive criteria for malignancy are distant metastasis and local invasion, Weiss proposed a system encompassing 9 morphologic criteria associated with locally recurrent and metastatic adrenocortical tumors ( Box 1 ). The subjective identification of 3 of these 9 criteria represents the current standard in establishing adrenocortical malignancy. This classification system, although simple and prognostic, has significant limitations: (1) the criteria do not perform well in the identification of special variants (eg, myxoid, sarcomatoid, pediatric, and oncocytic) and (2) their diagnostic accuracy is lower when by applied by nonexpert pathologists ; subjectivity of assessment generates substantial interoperator variability, which limits diagnostic reproducibility. Several immunohistochemical markers have emerged as adjuncts to standard histopathologic analysis and may reduce ambiguity (eg, Ki67 proliferation index, steroidogenic factor-1 [SF-1], tumor protein P53, insulin-like growth factor (IGF) 2, cyclin E, reticulin, E3 ubiquitin-protein ligase [MIB-1]). Although promising, these markers have not consistently discriminated ACC from benign adrenal lesions in retrospective studies, and large-scale validation is lacking.
- •
High nuclear grade (grade 3 or 4)
- •
Mitosis 6/50 high-powered field or higher
- •
Atypical mitosis
- •
Clear cells 25% or less
- •
Diffuse architecture 33% surface or more
- •
Confluent necrosis
- •
Venous invasion
- •
Sinusoidal invasion
- •
Capsular infiltration
The identification of 3 of these 9 criteria represents the current standard in establishing adrenocortical malignancy.
Once malignancy has been established using biochemical, imaging, or pathologic criteria, tumor stage is prognostic of outcome. Although the TNM (tumor, node, metastasis) system from the American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (IUCC) was introduced in 2004, the European Network for the Study of Adrenal Tumors (ENSAT) classification has emerged as a more discerning predictor of cancer-specific mortality risk ( Table 1 ). Although the two systems classify stage I and II tumors identically (ie, node-negative tumors ≤5 cm or >5 cm, respectively), ENSAT stage III tumors are defined by the presence of positive lymph nodes, infiltration of periadrenal tissue and/or adjacent organs, or venous (ie, IVC or renal vein) tumor thrombus; stage IV ACC includes patients with distant metastasis only. In 492 patients from the German ACC registry, this modification yielded a stage-stratified 5-year disease-specific survival of 82% (stage I), 61% (stage II), 50% (stage III), and 13% (stage IV). The prognostic superiority of the ENSAT, compared with the AJCC/UICC, classification was corroborated in an independent North American cohort of 573 patients. Further improvements to the prognostic value of the ENSAT system, such as addition of tumor grade or molecular markers (eg, SF-1), have been advocated and may be on the horizon.
| Primary tumor (T) | |
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| T1 | Tumor <5 cm in greatest dimension, no extra-adrenal invasion |
| T2 | Tumor ≥5 cm in greatest dimension, no extra-adrenal invasion |
| T3 | Tumor of any size with local invasion (periadrenal tissue) but not invading adjacent organs |
| T4 | Tumor of any size with invasion of adjacent organs (kidney, diaphragm, great vessels, pancreas, spleen, liver) |
| Involvement of regional nodes (N) | |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in regional lymph nodes |
| Distant metastasis (M) | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
| Stage | AJCC/UICC/WHO | ENSAT |
|---|---|---|
| I | T1, N0, M0 | T1, N0, M0 |
| II | T2, N0, M0 | T2, N0, M0 |
| III | T3, N0, M0 | T3-4, N0, M0 |
| T1-2, N1, M0 | T1-4, N1, M0 | |
| IV | T3, N1, M0 T4, N0-1, M0 Any M1 | Any M1 |
Beyond ENSAT/AJCC tumor stage, completeness of resection (ie, R0 margin status) is a dominant contributor to disease-free and overall survival in resected ACC. In a retrospective study of 113 patients, patients undergoing complete primary resection demonstrated significantly improved median (74 vs 12 months) and 5-year actuarial survival (55% vs 5%) compared with those undergoing incomplete resection. In an analysis of 3982 patients with ACC from the National Cancer Data Base (NCDB), R0 resection was associated with a 5-year relative survival rate of 50.4%, compared with rates of 23.2% and 10.8% for R1 and R2 resection, respectively. After adjusting for age, tumor size, grade, nodal involvement, presence of distant metastasis, type of resection, and receipt of multimodality therapy, margin-positive resection remained associated with worse risk-adjusted mortality (hazard ratio [HR], 2.06; 95% confidence interval, 1.74–2.43; P <.0001).
In this and other studies, older age, sex, hormone hypersecretion, poorly differentiated histology, multivisceral resection, and nodal or distant metastasis are also associated with poor prognosis. Tumor size, although firmly entrenched in staging classifications, is inconsistently associated with prognosis. Conversely, pathologic characteristics such as mitotic rate, atypical mitotic figures, intratumor hemorrhage, tumor necrosis, and Ki67 index are more reproducibly associated with long-term outcomes. Finally, gene expression profiling has identified molecular signatures (eg, DLG7 , PINK1 , and BUB1B ) predictive of malignancy and survival ; however, prognostic stratification using such techniques have yet to be widely adopted into clinic practice.
What are the principles of surgical and perioperative management for primary tumors? How should patients who have undergone resection be surveilled?
Surgical resection remains the cornerstone of treatment and the only curative modality for patients with localized ACC. The surgeon’s involvement in the care of these patients should begin in the preoperative setting. In patients with hypercortisolism, perioperative steroid replacement, typically with tapering doses of intravenous hydrocortisone, is recommended to mitigate the risk of adrenal insufficiency following adrenalectomy due to a suppressed contralateral gland. The duration of steroid therapy is dictated by time to recovery of the hypothalamic-pituitary axis.
Once the decision to proceed with resection has been made, aggressive local surgical control should be attempted to achieve negative resection margins. Unilateral or bilateral subcostal or J- or L-shaped incisions afford adequate access to sites of potential local invasion and metastatic spread. A thoracoabdominal incision is rarely indicated because of its incident morbidity but may be helpful when concomitant pulmonary metastasectomy is planned (see section “Is there a role for an aggressive surgical approach in locally recurrent or metastatic disease?”). En bloc resection of contiguous or discontiguous periadrenal viscera (eg, kidney, colon, spleen, pancreas, stomach) is often required to maintain capsule integrity and prevent tumor spillage.
A unique consideration during surgical resection of ACC is the potential for intracaval extension and/or tumor thrombus (especially for right-sided lesions), observed in up to 25% of cases. Although local vascular invasion carries a poor prognosis (ie, approximately 30% 3-year overall survival), it is not a contraindication to aggressive surgery per se. Careful preoperative planning is necessary to delineate the location and extent of venous involvement, because the principles of resection vary based on these factors. Tumor thrombectomy in the infrarenal IVC can be achieved by vascular control (via cross-clamping or hepatic vascular exclusion ), followed by cavotomy and primary closure or vein resection and reconstruction with or without graft interposition; if tumor extraction is not feasible, the infrarenal IVC can be safely resected with or without replacement. If suprahepatic IVC control is necessary, venovenous bypass is sometimes a useful adjunct. In cases of extension above the diaphragm, or especially into the right atrium, cardiopulmonary bypass may be necessary. Preoperative or intraoperative identification of thrombus in these locations is critical, because clamping of a thrombus-filled IVC can result in tumor thromboembolism, with ensuing hemodynamic instability or tumor dissemination. Management of isolated adrenal vein thrombus (AVT) without caval involvement is laterality specific: (1) for right-sided AVT, resection of a vascular cuff and primary closure of the IVC may be necessary to achieve negative margins; (2) for left-sided AVT, kidney-sparing left renal vein resection may be feasible if the azygous and gonadal venous drainage is intact; if the latter systems are involved, ipsilateral nephrectomy may be necessary (see section “Is there benefit to routine en bloc resection of adjacent organs or aggressive regional lymphadenectomy?”).
Hormone function should be monitored closely in the postoperative setting. As discussed earlier, postoperative adrenal insufficiency is managed with glucocorticoid and mineralocorticoid replacement as necessary, until recovery of the hypothalamic-pituitary axis. Postoperative hypercortisolism, typically observed after R1/R2 resections for hormonally overactive tumors, may be managed with a variety of agents, including metyrapone, aminoglutethimide, ketoconazole, mitotane (see section “What are the current and emerging options for multimodality management of adrenocortical carcinoma?”), mifepristone (glucocorticoid receptor antagonist), or etomidate. Sex steroid excess can be controlled with androgen receptor inhibitors bicalutamide or finasteride (in virilizing tumors) or antiestrogen therapies, such as tamoxifen or aromatase inhibitors (in estrogen-producing tumors).
Oncologic surveillance of patients who have undergone resection is recommended for up to 10 years and entails cross-sectional imaging with or without biochemical evaluation, depending on the functional status of the primary tumor. Patients with nonfunctional tumors should be under surveillance with periodic CT or MRI because of the risk for early and frequent recurrence (see section “Is there a role for an aggressive surgical approach in locally recurrent or metastatic disease?”). Patients with steroid-producing ACC should be monitored periodically with steroid tumor markers (eg, cortisol, DHEA-S, androstenedione). An increase in hormone levels may indicate recurrence and/or progression before radiographic detection.
Is there benefit to routine en bloc resection of adjacent organs or aggressive regional lymphadenectomy?
Although multivisceral resection for margin clearance is clearly indicated, the role for prophylactic organ resection, particularly nephrectomy, is more equivocal. Although early studies advocated for concomitant nephrectomy to improve oncologic outcomes, this premise has since been challenged. Bellatone and colleagues reported on 140 patients undergoing radical resection for advanced ACC; 22 (15.7%) underwent ipsilateral nephrectomy. The disease-free interval (16.6 vs 22.3 months) and recurrence rates (36.4% vs 37.3%) did not differ significantly between patients undergoing and not undergoing nephrectomy, respectively. In a preliminarily reported study by Porpiglia and colleagues, 20 of 82 (24.4%) underwent ipsilateral nephrectomy during curative-intent adrenalectomy; at a median follow-up of 60 months, disease-free and overall survival did not differ between nephrectomy and nonnephrectomy cohorts. Based on these limited data, routine ipsilateral nephrectomy is not recommended unless obvious renal infiltration by tumor or associated renal vein tumor thrombus is encountered intraoperatively.
Nodal status is not only an integral component of staging but also an important prognostic feature in resected ACC. Despite this, surgical extirpation of regional lymph nodes is infrequently performed, in part owing to lack of consensus regarding the optimal extent of regional lymphadenectomy during primary resection. Based on studies from the German ACC registry and NCDB, nodal metastasis is identified in approximately 25% of patients with resected ACC ; however, the alarmingly high rates of locoregional failure, up to 85% in some series, despite curative-intent resection ; substantially greater rates of nodal positivity, as high as 68%, in autopsy studies ; and widely variable survival statistics in patients with presumed node-negative stage II resected ACC (ie, indicating overlooked nodal metastasis in worse performers) suggest that the contribution of surgical understaging to poor long-term outcomes may be underappreciated.
The strongest evidence in support of routine regional lymphadenectomy is derived from a retrospective series of 283 patients who had undergone complete resection from the German ACC registry. In the absence of consensus guidelines defining adequate lymph node dissection (LND), an empiric threshold of 5 or more lymph nodes was chosen to discriminate patients in whom nodes were excised inadvertently from those in whom LND was intended. Using this threshold, only 47 (16.6%) underwent LND during primary resection. Although increased nodal retrieval in these cases may have been self-recommending because of the requirement for more extensive surgery—patients with LND underwent multivisceral resection more frequently and had larger tumors and more locally advanced (ie, ENSAT stage III) disease—removal of at least 5 regional lymph nodes was associated with significant reductions in both risk of recurrence (by 35%) and disease-related mortality (by 46%) despite controlling for age, tumor stage, multivisceral resection, and adjuvant treatment. Despite its methodologic limitations (eg, arbitrary determination of a 5-node LND threshold, lack of knowledge of surgical and/or pathologic quality), the greater than 70% 5-year disease-specific survival in the LND cohort makes a compelling argument for an aggressive surgical approach incorporating regional lymphadenectomy for primary ACC.
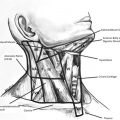
The optimal anatomic extent of such nodal dissections remains incompletely understood. Recent efforts to define a systematic approach to regional lymphadenectomy have drawn upon the current anatomic understanding of lymphatic drainage from the adrenal glands, as well as an evolving knowledge of locoregional recurrence patterns following complete resection. A recent report suggested that first-order drainage pathways from the adrenals encompass renal hilar nodes, nodes associated with the celiac axis, and ipsilateral para-aortic and/or paracaval nodes. These descriptive anatomic pathways correspond closely with actual patterns of postresection locoregional failure, observed most often in the ipsilateral para-aortic/paracaval and renal hilar regions, without contralateral extension. Based on these findings, Gaujoux and Brennan proposed a systematic dissection involving celiac, renal hilum, para-aortic, and/or paracaval lymph nodes ipsilateral to the tumor extending from the aortic hiatus to the renal vein. Reibetanz and colleagues proposed a similar, but laterality-specific, approach: for right-sided ACC, boundaries for lymphadenectomy are the lower edge of liver (upper), border of the IVC (left lateral), and renal pedicle (lower). For left-sided ACC, boundaries are the diaphragmatic crus (upper), border of aorta (right lateral), and renal pedicle (lower).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree