and Paul Telfer2
(1)
Department of Haematology, Guy’s and St Thomas’ Hospital, London, UK
(2)
Department of Haematology, Royal London Hospital, London, UK
Introduction
Surgery is often necessary in patients with SCD, the most common procedures being tonsillectomy and splenectomy in children and laparoscopic cholecystecomy and joint replacement surgery in adults. There is an increased risk of surgical complications (infection, thrombosis), and complications related to SCD (painful sickle crisis and acute chest syndrome). For optimal outcomes, it is important to co-ordinate care given by surgeons, anesthetists and hematologists. The medical condition of the patient should be optimized before surgery, and planned procedures should be postponed if the patient is febrile or has a sickle cell crisis.
Preoperative Screening for SCD and Carrier Status
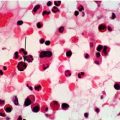
Whilst most patients will be aware that they have SCD, it is prudent to ensure testing has been done on all non-Northern Europeans prior to surgery. For routine surgery this can be done in the preoperative assessment clinic, by requesting full blood count, film and haemoglobinopathy screen (by HPLC or alternative laboratory method). Patients who are identified to have SCD should be discussed with the hematology and anesthetic team and a management plan developed as outlined below. In the emergency setting, where the sickle cell status is not known at the time of surgery, an urgent sickle solubility test, full blood count and haemoglobinopathy screen should be requested, but often the result of the haemoglobinopathy screen will be not be available immediately. A negative sickle solubility test will exclude a sickling disorder. If positive it will not discriminate between carrier or disease status. In this situation the full blood count result and blood film should be reviewed. If the patient has a normal hemoglobin concentration and no history of painful crises then HbSS is unlikely. A normal hemoglobin may be seen in HbSC but the blood film will show characteristic changes. The hematology team should be contacted for advice. If surgery is urgent it should proceed and the patient should be treated as if they have SCD until confirmatory tests are available.
Preoperative Management
All patients with SCD who need general anesthesia should be discussed with their hematologist prior to planned surgery to co-ordinate management. Suggested preoperative investigations are outlined in Table 17.1.
Table 17.1
Preoperative blood tests
Investigation | Purpose |
|---|---|
Full blood count | To compare Hb with previous results. Current Hb level is required for decision on pre-operative transfusion |
Haemoglobin analysis by HPLC | Recommended for evaluating current pre-transfusion HbS% |
Renal function | To assess for sickle nephropathy |
Group and antibody screen | To confirm there are no red cell antibodies |
Extended red cell phenotype | If this has not previously been done
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|