11 Surgical Biopsy
Introduction
Nonpalpable masses are identified by imaging, primarily screening mammography. The use of screening mammography has significantly increased over the last 20 years. The National Health Interview Survey showed that the percentage of eligible women undergoing mammography has increased from 29% in 1987 to 76% in 2000.1 This significant escalation has led to an increase in the way in which breast biopsies are performed and has provided the impetus for changes in technology. Biopsies are performed for both palpable and nonpalpable lesions, and current techniques incur less morbidity with more accurate tissue sampling.
The use of breast biopsy as part of the algorithm in diagnosing breast cancer is a relatively new component in the workup of breast cancer. Only a few decades ago a woman with a breast mass would go to the operating room not knowing whether she would wake up with a mastectomy or an intact breast. The ability to biopsy both palpable and nonpalpable lesions as early as possible has led to a decrease in breast cancer mortality and morbidity. Current practice guidelines recommend core biopsy, if possible, before surgical intervention for both palpable and nonpalpable lesions.2
Evaluation of a Palpable Breast Lesion
Most palpable breast masses are benign (Box 11-1). Nevertheless, a breast mass that is palpable on physical examination requires careful evaluation. A thorough history, physical examination, and imaging are necessary before obtaining a sample of tissue for pathologic diagnosis (Boxes 11-2 and 11-3). Depending on the age of the patient and other risk factors, imaging might include mammography, ultrasound, or both. Mammography is performed to gather further information about the known lesion as well as screen the breast for other occult lesions. Although mammography is our best tool for screening, it has a high false-negative rate and cannot be relied on exclusively for diagnosis. Ultrasound is an important tool for evaluating a palpable abnormality and is very reliable in discriminating a solid mass from a cyst. It is also helpful in differentiating discrete masses from fibroglandular change, which can also have a lumpy texture. If a patient with a complaint of a palpable mass that has benign characteristics on clinician physical examination has a negative targeted ultrasound, the negative predictive value for cancer is 99.8%.3 Nevertheless, a discrete, persistent breast mass—whether or not it is visible on ultrasound—should have a tissue diagnosis.
Box 11-2 Pertinent Information From Patient History
Length of time mass has been present
Personal history of previous masses or biopsies
Box 11-3 Pertinent Physical Examination Findings
Lymphadenopathy in the axillary, supraclavicular, or infraclavicular basins
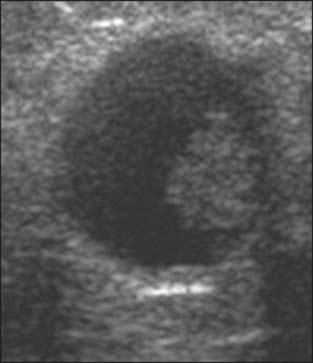
A simple cyst identified by ultrasound does not require any further diagnostic evaluation or therapeutic intervention (Fig. 11-1). If the cyst is symptomatic, however, a cyst aspiration can be performed to relieve pain or to deflate the palpable abnormality. The technique for aspiration of a cyst involves infiltration of local anesthetic into the skin overlying the lesion. Using a 21- or 22-gauge needle attached to a 20-mL or larger syringe, the needle is advanced into the lesion and fluid is aspirated. Cyst aspirations can also be performed under ultrasound guidance.
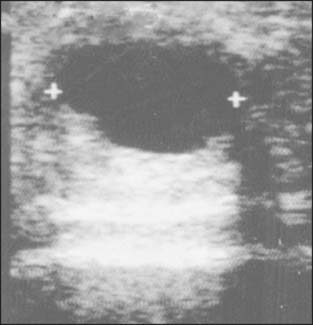
Figure 11-1 A simple cyst has smooth borders, no internal echoes, and good through transmission on ultrasound.
Cyst fluid may be clear or cloudy yellow, green, gray, or brown. This fluid can be discarded, because many studies have shown that cytologic evaluation of benign cystic fluid has no value.4 A purely blood aspirate or an aspirate of what appears to be old blood should be sent for cytology, and excision of the lesion should be performed. After aspiration of the cyst, the mass should disappear. A mass that persists, recurrent masses, or a bloody aspirate constitutes an indication for surgical excision.
Several techniques are available for biopsy of a palpable complex cyst or a solid mass. These include fine-needle aspiration (FNA), core biopsy, and surgical biopsy. The most appropriate technique is determined by the characteristics of the target lesion.
Complex Cyst
A complex cyst is a cystic lesion that contains a solid component, either extending from the wall of the cyst or contained within the cystic portion (Fig. 11-2). Careful consideration needs to be given to the biopsy technique selected for sampling a complex cyst. If the cystic component is ruptured and the fluid evacuates without obtaining an adequate sample of the solid component, the lesion may not be identifiable on subsequent ultrasound. Therefore, FNA would not be appropriate. If the solid component is significant so that evacuation of the cystic contents is not a concern, then an ultrasound-guided core biopsy is an option. If there is concern about loss of the landmarks, however, then a surgical excisional biopsy should be performed.
Biopsy Techniques
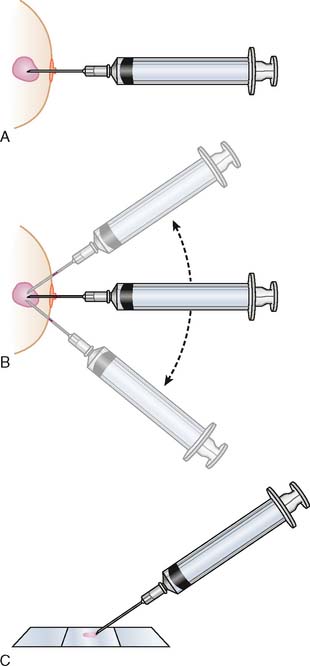
Fine-Needle Aspiration
FNA is a simple procedure that can be performed in the office without anesthesia (Fig. 11-3). It can be helpful to identify fibroadenomas, other benign lesions, and cancers. Several advantages exist for using FNA as a first-line diagnostic test. It is simple and quick to perform, carries a low risk of morbidity, involves very little patient discomfort, and has a low cost. With a skilled cytopathologist, the false-positive rate can be as low as 0.5%. The disadvantages of FNA include an inability to discriminate between an in situ and an invasive lesion, a high false-negative rate in the hands of pathologists without significant experience, and the requirement of further biopsy to obtain histologic confirmation if the cells appear malignant.5 The use of FNA versus core biopsy for initial diagnosis depends on the local resources of the practice. It is best applied in a practice that has quick access to an experienced cytopathologist who can provide a diagnosis with a very short turn-around time, that is, in less than 24 hours, or who can obtain a tissue diagnosis in a probable benign lesion such as a fibroadenoma, in which the patient wants to avoid a larger biopsy procedure. Nondiagnostic results, discordant results, papillary lesions, and hypercellular lesions need to proceed to a larger biopsy for definitive diagnosis. Malignant lesions, of course, need to proceed to further treatment planning.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree