Fig. 13.1
A D1 solitary osteolytic metastasis; the 56-year- old patient underwent en bloc vertebrectomy and reconstruction with homoplastic diaphysis segment filled with the autoplastic morcellized bone, plates, and screws; (a) preoperative CT scan showing an osteolytic lesion in the D1 vertebral body, (b) preoperative MRI, (c) intraoperative imaging showing posterior stabilization, and (d) a 2-year follow-up X-ray
Cervical en bloc vertebrectomy is technically more difficult so no case is evident in literature for metastatic patients.
13.1.2 Stabilization and Intralesional Surgery (Curettage)
In case of risk of fracture, or in case of spinal cord compression, patients enrolled in group II of Tokuhashi (intermediate survival) decompression and/or stabilization could be a good solution.
In 2012, Crnalic et al. [13] identified a new specific score for patient with cord compression from prostate cancer; the items include hormone status of prostate cancer, Karnofsky performance status, evidence of visceral metastasis, and preoperative serum prostate-specific antigen (PSA). They identified three specific prognostic groups corresponding to different score:
Group A (score 0–1), with a median survival of 3 months
Group B (score 2–4), with a median survival of 16 months
Group C (score 5–6), where more the half part of the patients were alive at publication of their experience
Patients with a score higher than 2 are more suitable to undergo surgery in case of spinal cord compression.
Stabilization alone is rare, considering the high frequency of osteoblastic lesions; nevertheless it can be fundamental in case of spinal cord compression; indeed, the following decompression can cause an iatrogenic instability.
Decompression can be performed both from anterior and posterior approach basing on the metastasis-specific localization, the spine level, and the surgeon expertise. In the thoracic spine, decompression should be performed from an anterior approach because the presence of the spinal cord could make difficult and effective decompression from a midline posterior access; nevertheless, cutting roots could be useful to have access to the vertebral body from behind.
At lumbar levels the presence of cauda equina allows an easier access to the anterior metastatic bodies.
Posterior stabilization is the most commune; it is performed by posterior midline incision or also by minimally invasive approach consisting in little incisions corresponding to the pedicles necessary for the screw insertion through the pedicle [14].
Several instrumentations are commercially available, but nowadays carbon fiber-reinforced rods should be preferred [15]. Indeed, they should allow a more effective adjuvant radiotherapy because it is characterized by a lower level of artifacts.
The artifacts at CT scan blind some areas in the surrounding tissue, introducing diffraction and refraction phenomena, so the actual dose administered to the tissues becomes unpredictable.
13.1.3 Augmentation Technique
Cement plasty (Kyphoplasty, vertebroplasty, vesselplasty): these techniques are very commune in osteoporotic fractures; nevertheless they can have indication also in metastatic lesion.
In case of metastatic spinal fracture, they can be able to stabilize it in a minimally invasive way, even if attention has to be paid for possible posterior cement or tumor migration.
Indeed, spine metastasis from prostate cancer difficultly causes body fracture, but they can cause important not responsive pain that can be effectively treated with these techniques [18, 19].
The procedure can be performed by monoportal or biportal transpedicular approach basing on the specific necessity of stabilization; the integrity of the posterior body wall is essential for safety performing the procedure (Fig. 13.2).


Fig. 13.2
A percutaneous vertebroplasty performed by biportal approach
13.2 Femoral Metastases Techniques
Proximal femur is the most commune site of metastasis, after the spine [20].
Even if the treatment of these lesions should not modify directly the survival from a biological/oncological point of view, the patient constricted to bed because of risk of fracture is exposed to complications that could interfere with medical therapies decreasing survival [21, 22].
Otherwise survival estimation is important as in the other sites for the best therapeutic strategy, but in case of metastases located in the limbs and moreover in the proximal femur, an important problem is to value the fracture risk [23].
Several systems are available, but the most used is the Mirel’s classification [24]; it identifies four items: location of the metastasis, its nature and radiographic appearance, its size related to the diameter of the entire segment, and the presence of pain.
Each item is scaled from 1 to 3.
When the total score is 7 or less, observation and radiation therapy is advisable; when it is 9 or more, prophylactic fixation is suggested; if the score is 8, the indication is uncertain, and it should be valued basing on clinical conditions as well.
1 | 2 | 3 | |
|---|---|---|---|
Location | Upper extremity | Lower extremity | Intertrochanteric |
Radiographic appearance | Blastic | Mixed | Lytic |
Size | <1/3 | 1/3–2/3 | >2/3 |
Pain | Mild | Moderate | Severe and functional |
The metastasis of prostate cancer is usually osteoblastic so surgical indication is usually less frequent than metastases from other primitive tumors.
13.2.1 Proximal Femur Resection and Prosthesis Reconstruction
In case of solitary lesion, in a healthy patient after several years from the primary tumor eradication, wide surgery has to be preferred. This means performing a resection of the proximal part of the femur which is extended distally about 2 cm distally to the inferior edge of the disease.
Reconstruction is performed with a modular prosthesis which is assembled to reach the resection size [25–27]; the intramedullary stem should be as long as possible to reinforce the entire femur, stabilizing the segment also in case of further distal metastasis onset. When the greater and the lower trochanters are not involved, they should be spared to maintain the muscular insertion (Fig. 13.3). The psoas muscle is the most important stabilizer.
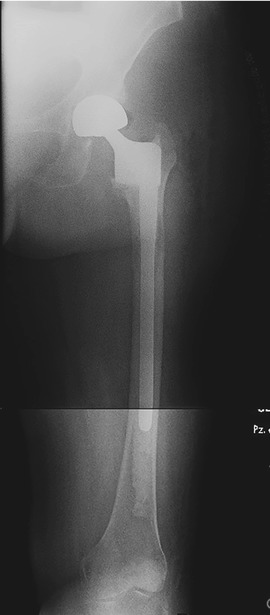
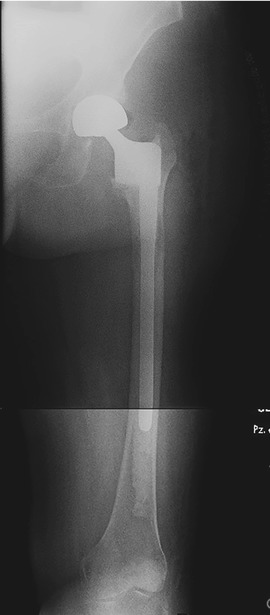
Fig. 13.3
A postoperative X-ray showing a hip prosthesis where the greater and lower trochanters and their muscular insertions were spared
An ideal modular prosthesis should allow a minimal resection, arming the entire femur when necessary; it should be cemented to assure the grip even in case of further metastasis.
Resection has to be preferred also in case of multimetastatic patients when the disease extends also in the head and femoral neck; intramedullary nailing should complicate with proximal screws cut out.
13.2.2 Diaphysis Resection and Reconstruction
The indication to resection in the diaphysis is the same of that of the proximal femur. Obviously it is very rare. Reconstruction can be performed with a diaphyseal prosthesis (Fig. 13.4) or a homologous diaphysis filled with cement and stabilized with plate and screws [28].
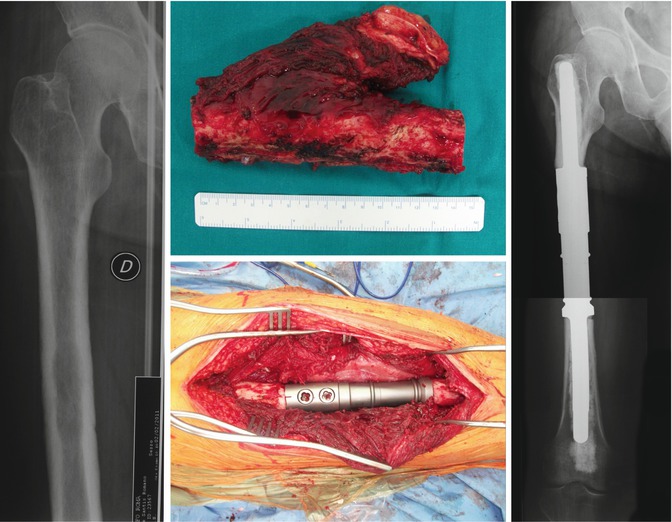
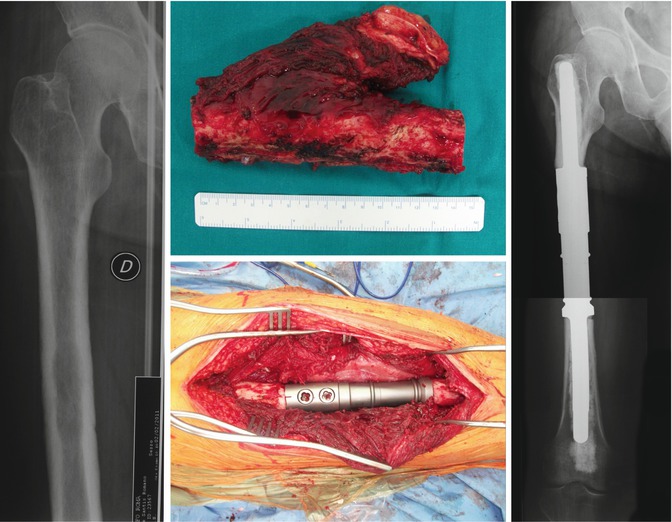
Fig. 13.4
A solitary lesion of the femur diaphysis on the left; in the upper center figure the resected specimen and in the lower center picture a diaphyseal prosthesis; on the right the postoperative X-ray
13.2.3 Intramedullary Stabilization
Intramedullary stabilization is the mainstay treatment in case of fractures or impeding fractures of lesions located from the trochanteric area until the distal diaphysis in multimetastatic patient [29]. Surgery aims to allow weight bearing as soon as possible so that the patient can undergo chemotherapy.
The nail must be always long and stabilizes the entire femur; it has to be distally locked, and a cervical screw must be always present even in case of diaphyseal metastasis considering the high frequency of femoral neck lesions: the screw in the femoral head will stabilize the femur also in case of successive metastasis (Fig. 13.5) even if a recent study sustains that it is not always necessary [30].