Fig. 10.1
Enucleation of a 1.5 cm insulinoma on the posterior surface of the pancreatic head in a adult
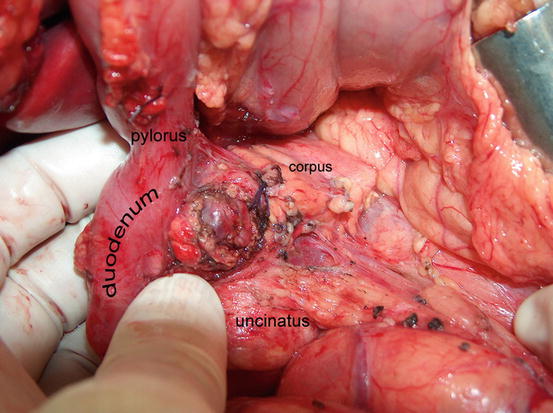
Fig. 10.2
Enucleation of a 1.5 cm insulinoma on the anterior surface of the pancreatic head in a 9-year-old child
Consider intraoperative secretin stimulation (2 units of secretin per kg body weight, as single intravenous bolus dose) if you are not sure whether there is a relevant lesion to the pancreatic duct or to a related contributing duct.
If a leak of pancreatic juice occurs on stimulation, cover the defect with a Roux-en-Y (side-to-side pancreatojejunostomy) or pursue a standard pancreatic resection (e.g., distal spleen-preserving pancreatic resection).
If there is intraoperative suspicion of malignancy, attempt verification by frozen section and revert to an oncological resection type (right: pylorus-preserving partial pancreatoduodenectomy (PPPD), left: distal pancreatectomy).
Never resort to “blind” resections. If you do not identify the insulinoma, close the abdomen and reevaluate diagnosis and imaging. Consider regionalization of the insulin-producing source with ASVS if not yet done.
Laparoscopic surgery
Since palpation is not available, intraoperative ultrasound with a laparoscopic probe is mandatory for precise tumor localization and its topographical relation to the pancreatic duct.
Laparoscopic enucleation may be considered for superficially localized insulinomas that are mainly of the body and tail of the pancreas and that lack contact with major vessels or the pancreatic duct.
If the insulinoma lies in the tail and cannot be reasonably enucleated laparoscopically, laparoscopic distal spleen-preserving pancreatectomy may be an appropriate option.
Insulinoma (MEN1 Related)
May be multifocal
May be present in addition to other functioning or nonfunctioning pNEN, therefore:
Insist on preoperative regionalization (ASVS test, Imamura test) to ascertain the NEN responsible for hyperinsulinemia
In presence of multiple pNEN
Insist on a complete biochemical work-up, including gastrin, glucagon, somatostatin, pancreatic polypeptide (PP), and chromogranin A (CrA); include vasoactive intestinal polypeptide (VIP) only in cases with specific typical clinical symptoms.
Plan for a resection type that meets the requirements of multiple MEN1-related NEN (usually spleen-preserving distal pancreatectomy, eventually combined with enucleation in the head).
Gastrin-Producing NEN of the Duodenum/Pancreas (Gastrinoma): Zollinger-Ellison Syndrome (ZES)
Hallmarks
Most gastrinomas are small and located in the duodenum or pancreatic head (“gastrinoma triangle”) (see Chap. 9).
The clinical manifestations comprise recurrent (often complicated) peptic ulcer disease, chronic secretory diarrhea, and peptic esophagitis.
All gastrinomas should be considered malignant.
Up to 45 % of patients have lymph node involvement at diagnosis and 10 % present with liver metastasis.
Hypergastrinemia leads to ECL-cell hyperplasia in the stomach that can cause the development of ECL-omas (type II).
20–30 % of gastrinomas are MEN1 associated.
Gastrinomas represent approximately 15 % of pNEN.
Work-Up
Insist on:
A properly taken family history concerning MEN1
A proper clinical and biochemical work-up (see Chap. 8)
Evaluation for typically elevated fasting gastrin
Exclusion of other conditions leading to high gastrin levels:
Medication with proton pump inhibitors (PPIs)
Chronic atrophic gastritis (CAG)
Chronic renal insufficiency
Helicobacter pylori infection
Short bowel syndrome
Gastric outlet obstruction
Secretin stimulation test (see Chap. 8)
Biochemical screening for other potential MEN1-associated diseases
Preoperative localization work-up (see Chap. 9)
Intraoperative Prerequisites
Intraoperative ultrasound – to localize the gastrinoma within the pancreas
Frozen section – to prove the resection of a neuroendocrine tumor and safe resection margins based on histopathological criteria
Intraoperative gastroduodenoscopy – for transillumination to detect gastrinomas in the duodenal wall
Indication for Surgery
There is general agreement that all patients with sporadic gastrinoma without evidence of hepatic metastasis and no relevant comorbidities should undergo explorative surgery with the intention to cure.
Arguments:
Up to 95 % of gastrinomas are localized intraoperatively.
Biochemical cure is achieved in up to 60 %.
Surgery prolongs disease-free survival and reduces the development of hepatic metastasis.
Even in situations without positive localization in imaging studies, but with positive regionalization by ASVS to the duodenum/head of the pancreas, patients should be operated upon because they are very likely to have a small, resectable gastrinoma of the duodenum.
Surgical Technique
Gastrinomas in the body or tail of the pancreas: distal pancreatectomy with splenectomy and clearance of the regional lymph nodes.
Gastrinomas in the head of the pancreas: if locally appropriate, plan an enucleation with regional lymph node clearance and lymphadenectomy along the hepatoduodenal ligament. However, consider pylorus-preserving partial pancreatoduodenectomy (PPPPD) as an alternative.
Proven or suspected gastrinomas of the duodenum: after complete Kocher’s maneuver, localize gastrinomas by palpation and/or transillumination. Small gastrinomas can be resected in their mucosal layer after longitudinal duodenotomy in the second part of the duodenum. Larger tumors (>5 mm) should be removed with a full-thickness resection of the duodenal wall. Regional lymph node clearance and lymphadenectomy along the hepatoduodenal ligament are mandatory.
Gastrinomas (MEN1 Related)
Indication for Surgery
This issue is and has been the topic of many discussions, with controversial attitudes on how to surgically treat MEN1 patients with ZES without evidence of a hepatic spread.
Facts:
Most MEN1-associated gastrinomas are small, multiple, and located in the duodenum.
MEN1-associated gastrinomas tend to have a much more benign disease course than sporadic ones; this has to be carefully balanced against the morbidity of any surgical intervention.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





