Location of tumor
Total
%
Cervical
198
4.2
Upper thoracic
631
13.4
Middle thoracic
2,290
48.7
Lower thoracic
1,224
26.0
Abdominal
247
5.3
EG
31
0.7
EG junction (E = G)
26
0.6
Cardia
6
0.1
Unknown
46
1.0
Total
4,699
Missing
5
10.2 Cervical Esophageal Cancer
Free jejunal transfer is selected for esophageal reconstruction in a case in which the tumor is limited to the cervical esophagus. If the cancer extends to the thoracic portion or another tumor is present in the thoracic esophagus, esophageal reconstruction using the stomach or colon is generally performed after transhiatal esophagectomy. If the stomach or colon does not reach the cervical esophagus or the inferior pharynx, a free jejunal graft is additionally transferred between the proximal organ and the distal conduit.
10.2.1 Free Jejunal Transfer
The transverse coli artery and the superior thyroid artery are the respective first and second choices as the recipient arteries. The facial artery and the lingual artery are also candidates, but these arteries are hard to handle because of protrusion of the mandible. An external jugular vein (end-to-end fashion) or an internal jugular vein (end-to-side fashion) is used as the recipient vein.
10.2.1.1 Operative Technique
After dissection of the neck nodes, the recipient artery and vein are dissected and prepared. These dissected vessels are covered with wet gauze to avoid drying before vessel anastomosis.
A segment of the jejunum of 30–40 cm in length is harvested at approximately 50 cm distal from the ligament of Treitz. The mesentery of the jejunum to be grafted is transilluminated and the vessels of J2 or J3 to be used as donor vessels are carefully inspected and dissected. A marking suture on the donor jejunum is required to detect the direction of intestinal peristalsis before resection and the jejunal vessels are divided at their roots just before transfer. Irrigation of the vessels in the jejunal graft is not needed.
The resected jejunum is placed in the cervical space with isoperistalsis. The best order of performance of vessel anastomosis and intestinal anastomosis is unclear. Initial anastomosis of the vessels has advantages that microscopic vessel anastomosis can be performed without limitation of mobilization of the jejunal graft and that blood flow patency can be checked for a longer time during the operation. Vessel anastomoses are performed microscopically. Regions with arterial plaque are removed and both arteries are anastomosed atraumatically in the whole layer with 9–0 nylon sutures. Before vein anastomosis, the surgeon should check that the veins are not twisted and sagged via direct vision. Vein anastomosis is performed with 9–0 nylon sutures. Clamps on the vein and artery are taken off in order and blood flow and jejunal peristalsis should resume. The mesentery near the vessel anastomoses is secured to the deep cervical fascia to avoid pull on the anastomoses.
The jejunal graft is placed as straightly as possible without tension against the vessel anastomoses. The length of the jejunum for use as the graft is 12–15 cm and unneeded portions of the jejunum on the proximal and distal sides are removed. The redundant mesentery is filled into dead space around the trachea and wrapped around the vessel anastomoses. The jejunum is anastomosed to the orifice of the inferior pharynx layer to layer in an end-to-side fashion and anastomosed to the proximal esophagus using an Albert-Lembert or layer-to-layer suture in an end-to-end manner (Fig. 10.1).
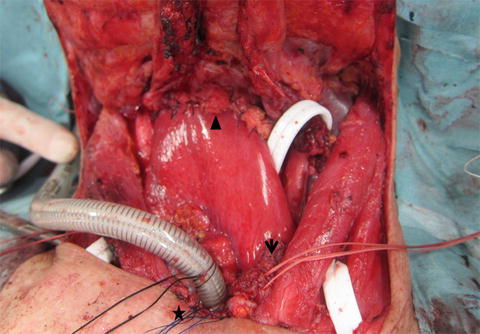
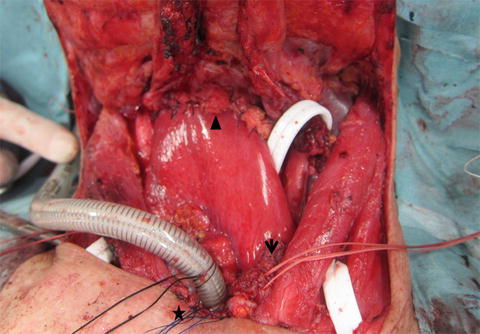
Fig. 10.1
Operative photograph of free jejunal transfer, showing anastomosis between the inferior pharynx and jejunum (arrowhead) and between the jejunum and esophagus (arrow). The tracheostoma is indicated by a star
10.3 Thoracic Esophageal Cancer
The stomach, colon, and jejunum are the main organs used for esophageal reconstruction in thoracic esophageal cancer. The stomach is used most frequently because fewer anastomoses are required, the operative procedure is relatively simple, and there is less surgical stress. In Japan, the stomach is used for reconstruction in 82 % of cases (Table 10.2) [2]. If the stomach cannot be used because of previous gastrectomy or synchronous gastric cancer, the vascular pedicled colon or jejunum is selected as an esophageal substitute.
Table 10.2
Organs used for reconstruction in Japan (2006)
Organs used for reconstruction | Cases | % |
|---|---|---|
None | 46 | 1.8 |
Whole stomach | 109 | 4.3 |
Gastric tube | 1,989 | 77.6 |
Jejunum | 103 | 4.0 |
Free jejunum | 46 | 1.8 |
Colon | 112 | 4.4 |
Free colon | 14 | 0.5 |
Skin graft | 1 | 0.0 |
Others | 140 | 5.5 |
Unknown | 3 | 0.1 |
Total lesions | 2,563 | |
Total cases | 2,541 | |
Missing | 4 |
10.3.1 Stomach
The use of the stomach as an esophageal substitute can involve three types of conduit with different widths: the whole stomach, a subtotal gastric tube, and a narrow gastric tube. This choice is made by the surgeon based on a consideration of the length and blood flow in the conduit. Blood supply in the relocated stomach is mainly from the right gastroepiploic artery and only from intramural blood flow in its upper tip. A wide stomach tube has a rich blood supply but a short length. A narrow stomach is longer, but has poor blood supply at the tip and tends to necrotize.
10.3.1.1 Operative Technique
The gastrocolic omentum is divided 3–4 cm from the right gastroepiploic vessels, the left gastroepiploic vessels are divided near their roots, and the short gastric vessels are also divided. During this series of procedures, a vessel sealing device (LigaSure™ or Enseal™) is useful for reduction of the operative time and blood loss. The portion of the right crus of the diaphragm passing to the left of the esophagus is exposed and the recurrent branch of the left inferior phrenic artery is divided. The lesser omentum is then divided and the portion of the right crus of the diaphragm passing to the right of the esophagus is exposed. The nodes along the celiac artery (No. 9; Japanese classification of lymph node [5]) and the nodes along the left gastric artery (No. 7) are dissected and the root of the left gastric artery is ligated and divided. The thoracic esophagus is pulled out of the esophageal hiatus and the stomach is mobilized with the thoracic esophagus. The esophageal hiatus is sutured and closed in a case in which the anterior mediastinal or subcutaneous route is used.
The surgeon picks up the fundus to find the highest point of the stomach [6] and decides on the position of the cut line in the lesser curvature (Fig. 10.2). For a whole stomach conduit, the cut line is on the esophagogastric junction; for a subtotal stomach tube, the cut line is a line connecting the points where the left gastric peripheral arteries enter the gastric wall; and for a narrow stomach tube, the cut line is 3–4 cm from the greater curvature (Fig. 10.3). Generally the lesser curvature is divided by a linear stapler several times and seromuscular sutures are added. When the lesser curvature is divided, the right and left cardiac nodes (No. 1 and No. 2) and the nodes along the lesser curvature (No. 3) are removed together. The gastric tube is put into a narrow vinyl bag and brought up to the cervical portion through the selected route. If the length of the gastric tube is insufficient, procedures such as mobilization of the duodenum, circular cutting in the seromuscular layer of the gastric tube, changing the reconstruction route to a shorter one, and hand sewing on the lesser curvature instead of stapling are useful.