Figure 3.1
Placement of a collar skin incision 3 cm above the sternal notch is often the preferred position for subtotal parathyroidectomy in an elderly person, as this will leave a scar in the lower neck (arrow a). In younger individuals, access may be through a smaller incision (2.5–3 cm), placed slightly higher, at the level of the thyroid isthmus, to avoid keloid formation (arrow b)
3.2.2 Normal Parathyroid Anatomy
Autopsy studies have revealed the location of normal parathyroid glands (Fig. 3.2a, b) [1] and have indicated that patients subjected to parathyroid operations should always be considered to have at least four parathyroid glands. Nearly 15% of normal persons harbor supernumerary glands, which may be enlarged in patients with hyperplasia/MGD. Recognizing symmetry in location also can be of help in visualizing pathological glands, as the superior glands have contralateral symmetry in about 80% of cases, and the inferior glands in about 70%. Both pairs of glands can be above or below the junction of the recurrent nerve and inferior thyroid artery, however.
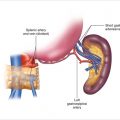
Figure 3.2
The localization areas of normal superior (a) and inferior (b) parathyroid glands. (Numbers represent percentages)
3.2.3 Fascial Layers
The strap muscles and the superficial cervical fascia are dissected from the thyroid surface, and the middle thyroid vein is divided and ligated to allow dissection within the “cotton-wool” plane lateral to the thyroid. In the lower neck, blunt dissection should safely push the thymus, the inferior parathyroid, and the recurrent laryngeal nerve towards the midline. The pretracheal fascia engulfs the thyroid in two layers, which laterally join to form the vascular sheath. The superficial fascial layer is dissected on the thyroid surface and traction is applied for visualization of the posterior border of the thyroid lobe (Fig. 3.3); on the right side, care is taken to avoid injury to a nonrecurrent laryngeal nerve. The fascia is distinct around the superior thyroid lobe but is more friable at the middle and lower thyroid. If the recurrent laryngeal nerve must be exposed, the covering thin fascia is cut longitudinally along the direction of the nerve to open up the posterior space. In children, this fascia layer over the recurrent laryngeal nerve is often distinct.
Figure 3.3
Visualization of the posterior border of the thyroid lobe, with typical locations of enlarged superior and inferior parathyroid glands
3.2.4 Exposure of Parathyroid Glands
When the thyroid lobe has been mobilized, the surgeon should inspect the most common locations of the parathyroids. The strategy of exposure is expressed as “not removing anything before seeing everything.” If the thyroid capsule has been exposed appropriately, palpation with an instrument may reveal glands sliding, together with lobules of fat, between the pretracheal fascia layers, from where they will be delivered when the ventral fascia has been transected on the thyroid lobe surface. For superior glands, the most pertinent area extends 1–2 cm around and above the nerve/artery junction; for inferior glands, the area is around the lower thyroid pole and the insertion of the thyrothymic ligament. The localization areas for normal superior and inferior parathyroid glands are depicted in Fig. 3.2, and typical locations of enlarged glands in Fig. 3.3. At operation, the enlarged pathological parathyroid glands can be identified by a brownish-reddish color (Fig. 3.3), glistening homogenous surface (easily separating from surrounding fat), and a palpable but soft consistency. The thyroid will generally appear more reddish, with a firm and nodular texture. Lymph nodes can be variable, either pale or reddish in color, and often lack a well-circumscribed texture; they generally will not separate as easily from surrounding fat.
Interest during this initial phase of the operation is focused also on exposure of normal-sized glands, as this will determine the appropriate strategy of parathyroidectomy. The color of normal glands will generally be yellow or brownish-yellowish; when the color is pale, the texture can help to distinguish a normal parathyroid from a tiny lobule of fat or the thymus (Fig. 3.4). At operation, the search for both pathological and normal parathyroid glands should be systematic.
Figure 3.4
The initial phase of the operation is focused also on exposure of normal-sized glands, as this will determine the appropriate strategy of parathyroidectomy. The color of normal glands will generally be yellow or brownish-yellowish; when the color is pale, the texture can help to distinguish a normal parathyroid from a tiny lobule of fat or the thymus
3.2.5 Superior Glands
The superior glands may be hidden in clefts on the thyroid surface, especially if the patient has a nodular goiter (Fig. 3.5), but are rarely deeply intrathyroidal in the superior thyroid lobe. The glands may be situated on or under the tubercle of Zuckerkandl, on or under artery branches or the recurrent laryngeal nerve, or they may be concealed close to (or even within) the ligament of Berry.
The glands can also be para-esophageal or retro-esophageal (Fig. 3.6), retro-pharyngeal, or located towards the tracheo-esophageal groove, but they will then generally be posterior to the recurrent nerve. A pathological gland can often be readily identified by palpation as a circumscribed but soft and movable tumor. The posterior branch of the superior thyroid artery often provides circulation to a superior parathyroid gland by a collateral to the inferior thyroid artery; the collateral can be spared by dissection close to the posterior thyroid border when preserving a normal parathyroid.
The superior glands can sometimes also be on the ventromedial side of the upper thyroid lobe, where they may be concealed by being flat and adherent to the surface of the thyroid capsule (Fig. 3.7). To reveal these glands, the posterior branch of the superior thyroid pedicle may have to be ligated, to allow medial rotation of the upper thyroid pole for exploration of its ventral surface. The posterior branch of the superior thyroid artery often provides collateral circulation to a superior parathyroid gland as described above.
Less than 1% of superior parathyroid glands are undescended, occurring up to 2 cm above the thyroid pole, typically medial to the vascular sheath and the carotid bifurcation. Such glands may be difficult to find, as they may be flattened out towards the pharyngeal wall and may be covered by pharyngeal muscles. A lateral approach between the sternocleidomastoid and strap muscles, anterior to the vascular sheath, can open this area.
As many as 30–40% of enlarged superior glands may be displaced by swallowing maneuvers to ectopic positions, by descending caudally in the tracheo-esophageal groove or along the esophagus towards the posterior mediastinum, in a compartment deep to the fascia and posterior to the nerve (Fig. 3.8a). The lower the gland descends towards the mediastinum, the more posterior becomes the location.
A gland may be identified by palpation after dividing the posterior sheath of the pretracheal fascia from the superior thyroid pole to the inferior thyroid artery, and introducing a finger along and behind the esophagus (Fig. 3.8b).
The gland may be pulled by traction along a prominent vascular stalk, turning caudally behind the inferior thyroid artery. These glands can be in the posterior superior mediastinum, and the space may have to be opened by incising the posterior fascia caudal to the inferior thyroid artery, carefully avoiding the recurrent nerve, which will be lateral to the compartment of descent. Occasionally, such glands may be in the midline, covered by a dense fascia, and may then be difficult to remove.
MIBI scintigraphy with SPECT can reveal the posterior and caudal displacement of these superior glands. It is crucial to distinguish them from inferior glands, which always have an anterior location in the cervical or mediastinal thymus. Table 3.1 outlines a strategy for locating a displaced superior gland.
Figure 3.5
The superior glands may be hidden in clefts on the thyroid surface, especially if the patient has a nodular goiter but are rarely deeply intrathyroidal in the superior thyroid lobe (arrow indicates a superior parathyroid glands partly hidden in the thyroid parenchyma)
Figure 3.6
Superior parathyroid gland with para-esophageal location
Figure 3.7




Superior parathyroid gland adherent to the ventromedial surface of the thyroid capsule
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree