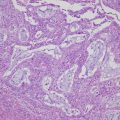
Fig. 8.1
Flowchart of fundamental strategies for the management of epithelial ovarian cancer. Cited from Komiyama et al. [3] with slight modifications
8.2 Surgical Management
8.2.1 Early (Localized to the Ovary)-Staged Ovarian Cancer
The primary aim of surgery for early ovarian cancer is to resect the tumor and define a precise pathological diagnosis to obtain definitive staging according to the International Federation of Gynecology and Obstetrics guidelines. Optimal staging laparotomy, which can reveal important information for subsequent treatment, includes bilateral salpingo-oophorectomy, total hysterectomy, omentectomy, peritoneal cytology, pelvic/para-aortic lymph node dissection (biopsy), and biopsies from sites in the abdominal cavity. Both retroperitoneal lymph node dissection up to the renal veins and intraperitoneal (IP) biopsy of the Douglas pouch, parietal peritoneum, surface of the diaphragm, intestinal tract, mesentery, and suspected lesions are informative factors for accurate staging. It is well known that the comprehensive surgical staging is important to disclose occult advanced disease [4, 5]. Therefore, if the final diagnosis of ovarian cancer is confirmed after initial surgery (incomplete surgery and/or staging), staging laparotomy by re-laparotomy should be performed [3]. Although retroperitoneal lymph node metastases have been observed in 5%–21% of patients with pT1 diseases, there is no strong evidence based on randomized clinical trials to indicate that lymph node dissections have any impact on the prognosis of early ovarian cancer [6].
The clinical requirement of preserving fertility in young patients with ovarian cancer may be present. The basic fertility-sparing surgical procedure for early ovarian cancer includes disease-side salpingo-oophorectomy, omentectomy, and peritoneal cytology with informed consent after providing detailed information about fertility preservation and the potential risk of disease recurrence [3]. In addition, staging laparotomy, including the biopsy of the contralateral ovary, pelvic/para-aortic lymph nodes, and sites in the abdominal cavity, should be considered to exclude the possibility of advanced disease. The basic indication for fertility-sparing surgery is stage IA disease with grade 1 or 2 of the serous, mucinous, or endometrioid histotype. In addition, stage IC (localized to one ovary with negative ascites cytology) with grade 1 or 2 of non-clear histotype or stage IA of clear cell histotype can also be considered for fertility-sparing surgery.
8.2.2 Advanced Stage (Stage II or More) Ovarian Cancer
Maximal debulking surgery to achieve complete visible disease resection is recommended for advanced ovarian cancer because no residual tumor at the end of surgery has been shown to be associated with prolonged patient survival [3, 7]. In general, complete surgery is defined if there is no residual tumor detectable by macroscopic evaluation, optimal surgery is defined as residual tumors of <1 cm in diameter, and suboptimal surgery is defined if the residual tumors are ≥1 cm in diameter. Surgical procedures that may lead to achieve complete resection include bowel resection, peritoneal stripping, diaphragm resection, bulky lymph node removal, splenectomy, and other procedures. Therefore, multidisciplinary expert surgical and medical management may be required. Conversely, indications for pelvic/para-aortic lymph node dissection in advanced ovarian cancer remain to be elucidated. A retrospective review of three randomized trials for advanced ovarian cancer indicated that lymphadenectomy might offer benefit mainly to patients with advanced ovarian cancer but without gross residual disease [8]. A multicenter randomized clinical trial, however, demonstrated that there was no difference in overall survival (OS) between patients with systemic lymphadenectomy and those with removed bulky nodes [9]. Altogether, systemic retroperitoneal lymphadenectomy could be considered if optimal surgery has been achieved in patients with advanced ovarian cancer.
If primary surgery for advanced ovarian cancer results in a suboptimal outcome, interval debulking surgery (IDS) should be considered as a treatment option during chemotherapy [3]. There have been two controversial randomized clinical trials about the value of this treatment strategy: the Gynecological Cancer Cooperative Group of the European Organization for Research and Treatment of Cancer (EORTC) trial, which showed IDS to have improved survival [10], and the Gynecologic Oncology Group phase III treatment trial, which reported negative effects of IDS for these patients [11].
Although the fundamental treatment strategy for advanced ovarian cancer has generally been primary debulking surgery (PDS) followed by chemotherapy, therapeutic benefit of neoadjuvant chemotherapy (NAC) followed by IDS is still debated. Till date, two large randomized clinical trials (the EORTC 55971/NCIC OV13 and CHORUS trials) have demonstrated that the prognosis of advanced ovarian cancer with NAC + IDS was not inferior to that of PDS followed by chemotherapy [12, 13]. In addition, a recent phase III noninferiority trial (the JCOG 0602 trial) comparing PDS with NAC + IDS conducted by the Japan Clinical Oncology Group supports the idea that NAC + IDS is becoming more widely accepted [14]. Based on these results, NAC + IDS could be considered as a treatment option for patients with advanced ovarian cancer in whom an optimal outcome by primary surgery cannot be expected because of its extensive dissemination and metastasis, poor patient condition, and serious complications [1–3]. The performance status and the American Society of Anesthesiologists (ASA) physical status classification are generally used for evaluating the patient’s general condition. Patient’s age (particularly of the elderly), general condition, nutrition status, and clinical stage should be taken into consideration for choosing appropriate surgery. It should be noted that the incidences of intraoperative and perioperative complications are frequent in elderly patients. Because it is thought that maximal debulking surgery should also be performed in elderly patients, NAC with the improvement of the general condition followed by IDS (hopefully complete surgery) should be considered in these patients [15].
8.2.3 Risk-Reducing Salpingo-Oophorectomy (RRSO)
Recent accumulating evidence has revealed that prophylactic bilateral salpingo-oophorectomy is associated with a reduced risk of breast, ovarian, fallopian tube, and primary peritoneal cancers in women with BRCA1 or BRCA2 mutations [16, 17]. Therefore, RRSO, under the institutional ethics committee approval, is recommended for the patients carrying BRCA1/2 mutations, along with genetic counseling by clinical geneticists and careful pathological review [3].
8.2.4 Laparoscope-Assisted Surgery
There is no difference in terms of the survival benefit for selected patients with early ovarian cancer between open laparotomy and minimally invasive procedures, such as laparoscope-assisted surgery, performed by experienced gynecologic oncologists [18]. In addition, it is noted that laparoscopic inspection for observing intraperitoneal cavity and for staging in patients with advanced ovarian cancer can be a useful method [19]. However, quite a few randomized trials of laparoscope-assisted surgery for ovarian cancer have been conducted till date, but laparoscope-assisted surgery is not currently recognized as a standard procedure that can replace open laparotomy [3]. In patients with advanced cancer, however, the minimally invasive procedure may be substituted for open laparotomy to observe the abdominal cavity and collect tissue samples [3]. Furthermore, in general, laparoscope-assisted approach can be used for prophylactic bilateral salpingo-oophorectomy.
8.2.5 Intraoperative Pathological Evaluation
Although the diagnosis of ovarian cancer may be made by preoperative evaluation and intraoperative findings, the judgment between benign and borderline malignancies is occasionally difficult. Intraoperative rapid pathological examination using frozen sections may help to select the optimal surgical procedure and avoid an unnecessary second surgical procedure in such cases [1–3].
8.3 Frontline Chemotherapy
8.3.1 Standard Chemotherapy
Standard frontline chemotherapies include (1) conventional TC therapy with paclitaxel (3-h intravenous infusion at 175 or 180 mg/m2) followed by carboplatin (1-h intravenous infusion of area under the curve [AUC] of 5 or 6) on day 1, given every 3 weeks for 6 cycles, and (2) dose-dense TC therapy with paclitaxel (1-h intravenous infusion at 80 mg/m2 on days 1, 8, and 15) plus carboplatin (1-h intravenous infusion at an AUC of 6 on day 1), given every 3 weeks for 6 cycles. Significant improvement in both progression-free survival (PFS) and overall survival (OS) with a dose-dense schedule when compared with conventional therapy in stage II–IV ovarian cancer was documented by the JGOG3016 trial [20, 21]. However, higher toxicity, which is a potential reason to discontinue treatment, was observed in dose-dense regimens.
As frontline chemotherapy, other than conventional TC therapy, DC therapy with docetaxel (1-h intravenous infusion at 70 or 75 mg/m2) followed by carboplatin (1-h intravenous infusion at an AUC of 5) on day 1, given every 3 weeks for 6 cycles, and also PLD-C therapy with pegylated liposomal doxorubicin (1-h intravenous infusion at 30 mg/m2) followed by carboplatin (1-h intravenous infusion at an AUC of 5) on day 1, given every 4 weeks for 6 cycles, can be considered as alternatives [3]. In addition, for frail and elderly patients who may not be able to tolerate these combination therapies, cisplatin or carboplatin monotherapy is recommended [3].
It has been suggested that response rates to standard first-line chemotherapy, which is conventionally used for high-grade serous carcinoma (HGSC), are less in rare ovarian cancer subtypes, such as low-grade serous carcinoma, clear cell carcinoma (CCC), and mucinous carcinoma [22]. However, at present, there is insufficient evidence to support the modification of standard chemotherapy according to tumor histopathology [3]. A randomized phase III trial (the JGOG3017/GCIG trial) of paclitaxel/carboplatin versus irinotecan/cisplatin as a first-line chemotherapy for stage IC-IV CCC showed no significant difference in 2-year PFS and OS rates [23].
Postoperative chemotherapy can be avoided for patients with stage IA or IB, grade 1 disease, as confirmed by optimal staging laparotomy [3], based on evidence from a Cochrane meta-analysis of five randomized clinical trials, including the ACTION and ICON1 trials. This meta-analysis aimed to evaluate the benefit of postoperative chemotherapy for early ovarian cancer and found that adjuvant platinum-based chemotherapy was effective in the majority of early ovarian cancer patients, except in the subpopulations involving patients with stage IA or IB, grade 1 disease [24].
8.3.2 Intraperitoneal Chemotherapy
IP chemotherapy after optimal surgery can be considered for advanced ovarian cancer [3], although this delivery method may have greater toxicity associated with catheter complications, such as infection, abdominal pain, and abdominal discomfort. The GOG172 trial demonstrated that IP chemotherapy conveyed a survival advantage to stage III ovarian cancer patients with no more than 1 cm of residual disease [25]. The IP chemotherapy regimen used in this trial was 24-h intravenous infusion of paclitaxel at 135 mg/m2 on day 1, followed by IP cisplatin at 100 mg/m2 on day 2, and IP paclitaxel at 60 mg/m2 on day 8, given every 3 weeks for 6 cycles. A recent Cochrane meta-analysis of nine randomized clinical trials reported reliable estimates of survival benefits for IP chemotherapy for advanced ovarian cancer [26].
8.3.3 After Primary Treatment
In general, observation rather than maintenance chemotherapy is recommended for patients who exhibit no evidence of disease progression (complete remission) after initial treatment because the usefulness of maintenance chemotherapy has not yet been demonstrated through several randomized clinical trials [27–30]. However, maintenance with molecular targeted drugs, which is described in a later section, has been shown to increase PFS when the agents were concurrently used with TC therapy followed by maintenance therapy. If complete remission is not achieved by initial treatment (partial remission or progression), additional treatment (second-line chemotherapy and radiotherapy), participation in a clinical trial, or best supportive care should be considered [1, 3].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree