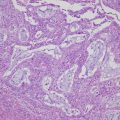
Fig. 9.1
Serous borderline tumor, micropapillary pattern. Non-hierarchial pattern is shown with micropapillary projection five times longer than width at least 5 mm in dimension with fibrous stalks
The prognosis of SBT is excellent in stage I tumor, and advanced-stage SBT with noninvasive implant still has 90% in 5-year survival rate. Nevertheless, longtime follow-up should be required, because recurrence may occur in longer period as about 20 years [7].
9.3 Characteristics of Mucinous Borderline Tumor and Seromucinous Borderline Tumor
Mucinous borderline tumor (MBT) is diagnosed by the proliferation of mucinous epithelial tumor cells with intermediate (variable) nuclear atypia and an absence of frank stromal invasion. In 2014 WHO tumor classification about mucinous tumors was revised. Only intestinal-type mucinous ovarian tumor was classified as mucinous tumor. And tumor with two or more epithelial types, such as endocervical-type mucinous, serous epithelium, and rarely endometrioid or squamous epithelium, was newly classified as seromucinous type [8]. These two tumors should be discriminated, because their clinical characteristics are apparently different [9]. MBT intestinal type is more frequently (85% of MBT), and usually large and multicystic tumor, and mostly confined to the ovary. Seromucinous BOT includes tumors which were used to be called as endocervical-like mucinous, mixed Müllerian mucinous, and mixed serous, endometrial, or squamous borderline epithelium. Prognosis of MBT was excellent in stage I tumor. Seromucinous BOT has 40% of bilateral tumors, and more than 20% are stage II–III tumors like SBT [4]. Also clinical behavior of seromucinous BOT resembles with SBT [10].
MBT has often heterogeneous histology, containing areas of cystadenoma or mucinous carcinoma. The discordant diagnosis of frozen section and permanent diagnosis occurs in 34% of MBT [11]. The prognosis of MBT is also excellent, but around 10% of MBT has recurred during 5–10 years period as mucinous carcinoma. Most recurrent cases have the possibility of sampling error at the primary tumor resection because of more heterogeneity (benign, borderline, intraepithelial carcinoma, microinvasion, invasive carcinoma) in huge mucinous tumor [12]. If borderline is suspicious, adequate pathologic sampling is needed. National Cancer Institute-sponsored ovarian tumor workshop proposed that one section per cm (<10 cm) and two sections per cm (>10 cm) should be obtained for the accurate diagnosis [13].
9.4 Surgical Management of BOT
9.4.1 Standard Surgical Procedure
Standard surgical procedure for BOT is staging laparotomy for ovarian cancer excepting systemic lymphadenectomy by open surgery. Lymphadenectomy can be omitted even for stage II and III disease, as there is no difference in the recurrence or survival rate between with and without lymphadenectomy [14]. No residuals at surgery would be very important as a favorite prognostic factor. If suspected peritoneal lesions are found by intra-abdominal examination, removing such lesions should be considered, or taking peritoneal biopsies from several sites should be considered if there are no suspected peritoneal lesions [15]. Appendectomy is to be added for MBT.
For patients who wish to preserve fertility, in addition to salpingo-oophorectomy on the affected side + omentectomy + peritoneal cytology, detailed intra-abdominal examination should be considered [15].
9.4.2 Laparoscopic Surgery and Restaging Surgery
BOT which was diagnosed accurately has excellent prognosis. Some surgical factors are related to recurrence of BOT, such as cystectomy, incomplete resection, and intraoperative spillage. Recently, laparoscopic surgery (LS) has become a standard procedure for benign ovarian tumor resection. LS was often employed for BOT with preoperative diagnosis as a benign tumor. LS has the potential risk of recurrence such as rupture of cyst, tumor cell dissemination, and trocar site metastasis. Most recurrent cases after LS had received conservative therapy. Nevertheless, LS itself had no relation with worse prognosis [16].
Restaging surgery is planned when unexpected final pathological result of BOT is obtained after primary surgery. The upstaging rate varies 7–40% among the studies, and it was always remarkably higher in SBT, especially SBT-MP histology has high risk of upstage [17]. Most positive findings of upstaged cases are peritoneal implant or positive washing cytology (Fig. 9.2). The standard procedure of restaging surgery for BOT is as follows. Disease-side unilateral salpingo-oophorectomy (USO), careful inspection of peritoneum, random biopsy at peritoneum, infracolic omentectomy, appendectomy (in case of MBT), and washing cytology should be performed. If peritoneal implant is found, fertility preservation may be abandoned in some cases (Fig. 9.3). On the other hand, MBT has low incidence of upstaged cases as 4% [17]. Therefore, in case of MBT intestinal type, restaging surgery may be not required, if at least USO was already performed. Nevertheless, recheck the pathology by full-sectioned specimen which should be done to avoid missing the worse prognostic findings, such as intraepithelial carcinoma, microinvasive carcinoma, or mucinous carcinoma. In seromucinous BOT, therapeutic strategies are almost same as SBT (Fig. 9.4).
Fig. 9.2
Peritoneal implant in serous borderline tumor. (a) Small nodule on Douglas pouch peritoneum showed peritoneal (non invasive) implant (b)