Starting a Palliative Care Program
Hannah I. Lipman
Diane E. Meier
Introduction: Why Palliative Care?
The Case for Palliative Care
Palliative care is comprehensive medical care focused on relieving the suffering of patients facing serious or life-threatening illness and that of their families. It is provided across the continuum of illness from first diagnosis until death, should it occur, and bereavement. Curative or life-prolonging treatment may be provided concurrently with palliative care, as appropriate. An interdisciplinary team may provide palliative care in all medical settings: inpatient, outpatient, in the home, in long-term care, and in the emergency department.
The field of palliative care has expanded rapidly over the last two decades. This has been in response to the challenge to our health care system to provide high-quality care to increasing numbers of older patients with multiple chronic illnesses in recognition of the fact that symptom control, advance care planning and shared decision making, coordination of care across settings, and care of the dying patients are integral to the care of all seriously ill patients.
Clinical Imperative for Palliative Care
There is a high burden of pain and other symptoms among hospitalized patients (1), chronically ill patients in the community (2), and dying patients in all care settings (3). Most deaths occur in the hospital (50%) and nursing home (25%), despite most people’s stated preference for dying at home (4). As the population ages and the burden of chronic illness increases, the number of seriously ill patients who are in the oldest old age group increases. The use of nonbeneficial life-sustaining treatments for these patients is high despite preferences for care focused on quality and quantity of life (5).
Interviews with chronically ill patients show that the factors they value most are relief from physical symptoms, shared decision making with clinicians, avoiding a prolonged dying process, lessening the burden on caregivers, and strengthening personal relationships (6, 7, 8, 9). However, caregivers of dying patients report dissatisfaction with the quality of care in these areas at end of life (3, 10).
Most people with serious or chronic illness require assistance with care at home. This burden falls on their families (11). Caregivers are more likely to be depressed, face significant economic stress, and have a higher morbidity and mortality rate than age-matched controls (12). Physicians and policy makers, as well as the general public, express concern about the ability of the medical system to address the care needs of the chronically ill (13). Taken together, these factors have driven the rapid growth in palliative care programs in recent years.
Financial Imperative for Palliative Care
A striking 68% of all Medicare dollars are spent on 23% of all beneficiaries who have five or more chronic medical conditions (14). One fourths of all Medicare dollars are spent in the last year of life (15). Medical spending on those who die in any given year is not significantly different from spending on patients with similar illness burden who do not die in that year (15). This emphasizes the difficulty in prognosticating life expectancy accurately. Therefore, palliative care should be delivered throughout the continuum of illness on the basis of need and independent of prognosis, addressing the high utilization and the need for care for all patients with multiple chronic illnesses.
Educational Imperative for Palliative Care
To meet the challenges detailed in the preceding text, current and future generations of medical students and house staff must be educated in palliative care, the quality management of complex chronic illness. At present, medical education takes place primarily in acute care hospitals. The growth of palliative care programs in teaching hospitals aims to ensure that medical students and house staff are taught the core skills of palliative care: pain and symptom management, expert communication about care alternatives and decision support, and a sophisticated ability to help patients and families manage a complex and fragmented health care system. In 2000, 26% of a random sample of 100 teaching hospitals had a palliative care consultation service or inpatient unit (16). By 2003, according to data from the American Hospital Association survey, 68% of hospitals belonging to the American Association of Medical Colleges Council of Teaching Hospitals reported a palliative care program (17). The number of physicians trained to provide specialist-level palliative care is also increasing. As of 2005, there are currently over 50 palliative medicine fellowship programs and 1891 physicians are certified in the subspecialty in the United States (18). Progress is being made toward
recognition of the specialty by the American Board of Medical Specialties (19).
recognition of the specialty by the American Board of Medical Specialties (19).
How to Approach Starting a Palliative Care Program
Starting a new palliative care program in a health care institution is a challenging but rewarding task. The recommendations contained in this chapter are drawn from the data and experience of the Center to Advance Palliative Care (CAPC), an organization committed to increasing the number and quality of palliative care programs in the United States through the provision of technical assistance. Further details, links to relevant resources, and A Guide to Building a Hospital-Based Palliative Care Program (20), a publication of the CAPC may be found at http://www.capc.org (21).
Leadership
An effective leader to act as program champion throughout the planning and implementation process is critical to success. In addition to commitment to the mission of palliative care to relieve suffering, improve communication and care across settings, and meet the system-wide challenges of an aging population with chronic illness, the ideal program champion should be an experienced leader, an effective communicator, command respect throughout the institution, and have credibility with key institutional decision makers. The professional discipline of the program champion is less important than these personal leadership qualities. Whether the champion is a physician, a nursing leader, an administrator, or some other professional will depend on local institutional factors.
Building the Case at Your Institution
Securing Support
A successful program must be aligned with the mission, priorities, needs, and culture of the home institution. Taking the time to thoroughly understand these institutional characteristics before planning the program will pay off later. The institution’s mission statement and annual report are good sources of information about the hospital’s goals and clinical and financial strengths. Informal interviews with leaders of other recently implemented new programs may be informative about how to negotiate the approval and funding processes in the institution.
The new palliative care program will have an impact on the care provided by and work environment of clinicians from other medical services with similar goals, skills, and patient base, such as anesthesia pain, oncology, critical care, and geriatrics, as well various other hospital staff, including social work services, pharmacy, and nutrition. Meeting informally with representatives from these areas, as well as with key institution decision makers, provides an early opportunity to assess their needs, knowledge, and misconceptions about palliative care, as well as to educate them about what palliative care is and how it can successfully integrate with their work. Barriers to smooth implementation of the new service are therefore identified and may be overcome early in the planning process through this informal interviewing process.
These informal meetings may also identify candidates for the planning team, which will need to continue to build support within the hospital. Team members should have some of the same leadership qualities as the program champion, be committed to a collaborative effort, and represent the range of disciplines that provide palliative care. The team should also include at least one community representative invested in the success of the new program, such as a leader from an established and respected local hospice or a member of the institution’s Board of Trustees. The planning team will be responsible for conducting the system and needs assessment (see next section) that will yield quantitative and qualitative data about clinical care at and financial status of the hospital, including both strengths and opportunities for improvement, and will help recruit palliative care providers when the program is to be implemented. This core planning team projects an attitude of enthusiasm for seizing opportunities for positive change, advocates for the program in their spheres of influence, and works to overcome the inevitable barriers that face any new clinical service.
System and Needs Assessment
The purpose of the system and needs assessment is to thoroughly review and document the existing strengths and opportunities for improvement specific to the home institution before the design and implementation of the new program. A structured system assessment yields information about current institutional strengths and resources, which the palliative care program will build on. Examples of such resources are physicians, nurses, social workers, chaplains, and other providers who have expertise or interest in palliative care, elements of clinical infrastructure such as an electronic medical record or billing system, a strong anesthesia pain service, an efficient discharge planning or case management team, and productive relationships with local hospice leaders and community philanthropic leaders.
A structured needs assessment answers the question: does this institution need a palliative care program and, if yes, on what services and which patient populations can the new program have a biggest positive impact? Baseline data on the number of annual deaths, their mean and median length of stay, and their Diagnosis Related Group (DRG) categories will be the basis for comparison to data collected after program implementation to demonstrate success. Examples of institutional needs identified with system assessment are the prevalence of untreated or undertreated pain and other symptoms, patient and family satisfaction, nursing and staff satisfaction and turnover, number of patients exceeding national benchmark length of stay for DRG, costs per day for such outliers, discharge delays, and pharmacy costs.
Adequate access to hospital data is necessary to conduct thorough system and needs assessments. Sources of data include the hospital information technology and financial records departments, results of ongoing quality-improvement initiatives, and patient and family satisfaction surveys mandated by the Joint Commission on Accreditation of Healthcare Organizations. The planning team may design and conduct its own surveys and informal interviews to supplement existing data. See Table 60.1 for a list of data to be gathered for the system and needs assessment.
Making the Financial Case
Palliative care improves the financial health of the institution primarily by cost avoidance, as opposed to revenue generation. Under Medicare, the major insurer of the chronically ill, hospitals are reimbursed for an inpatient stay according the DRG. The average length of stay and costs for the admission
diagnosis determine the appropriate DRG. Given this system, it is in the financial interest of the hospital, assuming that enough care has been provided to justify the designated DRG, to limit both length of stay and costs per day (22, 23, 24). The palliative care team facilitates timely clarification of goals of care, which often allows discharge to a less acute level of care, thereby shortening length of stay (25), and avoidance of nonbeneficial procedures, tests, and medications, thereby reducing daily hospital pharmacy, imaging, and ancillary costs.
diagnosis determine the appropriate DRG. Given this system, it is in the financial interest of the hospital, assuming that enough care has been provided to justify the designated DRG, to limit both length of stay and costs per day (22, 23, 24). The palliative care team facilitates timely clarification of goals of care, which often allows discharge to a less acute level of care, thereby shortening length of stay (25), and avoidance of nonbeneficial procedures, tests, and medications, thereby reducing daily hospital pharmacy, imaging, and ancillary costs.
Table 60.1 Useful Data for Palliative Care Programs | |||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
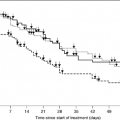
Clinical research data support these claims. One case– control study showed that daily hospital charges were reduced by 66% after transfer to a palliative care unit compared to the charges before transfer and by 59% compared to matched controls, without increasing mortality (26). Another study of palliative care for patients with cancer showed a decrease in proportion of patients dying in the hospital from 39% to 21% (27).
Interventions designed to identify patients in the intensive care unit (ICU) unlikely to benefit from critical care, improve physician–patient communication, and decrease delay in
clarification of goals of care (28, 29, 30, 31). have been shown to decrease ICU length of stay, decrease overall hospital days, and limit use of nonbeneficial life-sustaining treatment in critically ill patients without increasing mortality when compared to a control group. Over 80% of patients/surrogate, nurse, and physician participants in one study (30) found the intervention helpful. A detailed financial analysis (32) conducted by Gilmer et al. of their study (30) on ethics consultation (decision support similar to that provided by palliative care consultants) in the ICU showed reduced total costs through a reduction in length of stay among patients who did not survive to hospital discharge and a decrease in the number of patients with hospital stays of 10 or more days.
clarification of goals of care (28, 29, 30, 31). have been shown to decrease ICU length of stay, decrease overall hospital days, and limit use of nonbeneficial life-sustaining treatment in critically ill patients without increasing mortality when compared to a control group. Over 80% of patients/surrogate, nurse, and physician participants in one study (30) found the intervention helpful. A detailed financial analysis (32) conducted by Gilmer et al. of their study (30) on ethics consultation (decision support similar to that provided by palliative care consultants) in the ICU showed reduced total costs through a reduction in length of stay among patients who did not survive to hospital discharge and a decrease in the number of patients with hospital stays of 10 or more days.
Studies of comprehensive outpatient palliative care also show a decrease in system-wide costs driven by a decrease in the use of acute care services including emergency department visits, hospital days (33), and outpatient primary care and urgent visits (34).
To make this financial case clear to the hospital administration, the planning team must show how these findings apply to the home institution. The needs assessment has identified specific opportunities for cost saving. Study data from the CAPC provide estimates of the probable financial impact of palliative care. The following example illustrates how these data can be integrated to show how the new program will impact the institution in a real way.
First, estimate referral volume to show how many patients the new palliative care team will impact. Applying the national inpatient average death rate of 2.5% to the total annual hospital admissions will yield the approximate number of expected inpatient deaths in the institution per year. Approximately half of all referrals to inpatient palliative care consultation programs die in the hospital. Therefore, the potential number of referrals to the program annually can be estimated at 5% of all hospital admissions. This estimate should be compared to the institution’s actual inpatient mortality rate and adjusted accordingly if it deviates significantly from the national average of 2.5%. It is reasonable to assume that perhaps 20% of these potentially appropriate patients will be referred in the first year of the program. For example, 5% of a hypothetical 16,000 annual admissions yields 800 possible palliative care referrals. Assuming that only 20% of appropriate referrals will actually come to the service in the first year, the service can anticipate 160 referrals in this period (Table 60.2). This is only one method of estimating referral volume. Please refer to the CAPC Web site at http://www.capc.org for a detailed alternative and downloadable spread sheets for these financial projections and other interactive tools (21).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree