Cervix Uteri, Corpus Uteri, Ovary, Vagina, Vulva, Gestational Trophoblastic Tumors, and Fallopian Tube
In 1976, the American Joint Committee adopted the classification of the International Federation of Gynecology and Obstetrics (FIGO), which is the format used in the Annual Report on the Results of Treatment in Carcinoma of the Uterus, Vagina and Ovary , which is published every 3 years. This report has used the FIGO classification with periodic modifications since 1937, the last being 2009. Numerous institutions throughout the world contribute their statistics for inclusion in this voluntary collaborative presentation of data.
The cervix and corpus uteri were among the first anatomic sites to be classified by the TNM system. This uses extent of primary tumor (T), nodal metastasis (N), and distant metastasis (M) status to stage cancers. This system has been approved by the American Joint Committee on Cancer (AJCC) and the International Union Against Cancer (UICC). FIGO has worked closely for many years with the AJCC and UICC in the classification of cancer at gynecologic sites. Staging of malignant tumors is essentially the same, and stages are comparable in the two (FIGO and TNM) systems regarding categories and details.
Anatomy and Classification by Sites of Malignant Tumors of the Female Pelvis
Cervix Uteri
Anatomy
- 1.
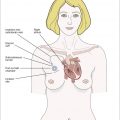
Primary site: The cervix is the lower third of the uterus. It is roughly cylindrical in shape, projects through the upper anterior vaginal wall, and communicates with the vagina through an orifice called the external os. Cancer of the cervix may originate on the vaginal surface or in the canal.
- 2.
Nodal stations : The cervix is drained by preureteral, postureteral, and uterosacral routes into the following first station nodes: parametrial, hypogastric (obturator), external iliac, presacral, and common iliac. Paraaortic nodes are second station and are considered metastases.
- 3.
Metastatic sites: The most common sites of distant spread include the aortic and mediastinal nodes, the lungs, and the skeleton.
Rules for Classification
- 1.
Clinical-diagnostic staging: Staging of cervical cancer is based on clinical evaluation; therefore, careful clinical examination should be performed in all cases by an experienced examiner, preferably with the patient under anesthesia. The clinical staging must not be changed because of subsequent findings. When there is doubt as to which stage a particular cancer should be allocated, the earlier stage is mandatory. The following examinations are permitted: palpation, inspection, colposcopy, endocervical curettage, hysteroscopy, cystoscopy, proctoscopy, intravenous urography, and radiographic examination of the lungs and skeleton. Suspected bladder or rectal involvement should be confirmed by biopsy and histologic evidence. Findings of optional examinations, such as lymphangiography, arteriography, venography, laparoscopy, computed tomography (CT) scan, and magnetic resonance imaging are valuable for planning therapy; however, because these are not generally available and the interpretation of results varies, the findings of such studies should not be the basis for changing the clinical staging.
- 2.
Surgical-evaluative staging: Surgical evaluation is applicable only after laparotomy or laparoscopy and examination of tumor and nodes. Fine-needle aspiration (FNA) of scan-detected suspicious lymph nodes may be helpful when planning treatment. Conization or amputation of the cervix is regarded as a clinical examination. Invasive cancers thus identified should be included in the reports (see no. 4 below).
- 3.
Postsurgical treatment — pathologic staging: In patients treated with surgical procedures, the pathologist’s findings in the removed tissues can be the basis for extremely accurate statements on the extent of disease. The findings should not be allowed to change the clinical staging but should be recorded in the manner described for the pathologic staging of disease. The TNM nomenclature is appropriate for this purpose. Infrequently, it happens that hysterectomy is carried out in the presence of unsuspected extensive invasive cervical carcinoma. Such cases cannot be clinically staged or included in therapeutic statistics, but it is desirable that they be reported separately. Only if the rules for clinical staging are strictly observed will it be possible to present comparable results between clinics and by differing modes of therapy.
- 4.
Retreatment staging: Complete examination using the procedures cited in no. 2, including a search for distant metastases, is recommended in cases known or suspected to recur. Biopsy and histologic confirmation are particularly desirable when induration and fibrosis from previously treated disease are present.
- 5.
Only if the rules for clinical staging are strictly observed will it be possible to compare results among clinics and by differing modes of therapy.
Staging Classification
| Stage I | The carcinoma is strictly confined to the cervix (extension to the corpus would be disregarded). |
| Stage IA | Invasive carcinoma that can be diagnosed only by microscopy. All macroscopically visible lesions—even with superficial invasion—are allotted stage IB carcinomas. Invasion is limited to a measured stromal invasion with a maximal depth of 5 mm and a horizontal extension of no more than 7 mm. Depth of invasion should not be more than 5 mm related to the basis of the epithelium of the original tissue (superficial or glandular). The involvement of vascular spaces—venous or lymphatic—should not change the stage allotment. |
| Stage IA1 | Measured stromal invasion of no more than 3 mm in depth and extension of no more than 7 mm |
| Stage IA2 | Measured stromal invasion of more than 3 mm and no more than 5 mm with an extension of no more than 7 mm |
| Stage IB | Clinically visible lesions limited to the cervix, uteri, or preclinical cancers greater than stage IA |
| Stage IB1 | Clinically visible lesions no larger than 4 cm |
| Stage IB2 | Clinically visible lesions larger than 4 cm |
| Stage II | The carcinoma extends beyond the cervix but has not extended to the pelvic wall or to the lower third of the vagina. |
| Stage IIA | No obvious parametrial involvement |
| Stage IIA 1 | Clinically visible lesion ≤4.0 cm in greatest dimension |
| Stage IIA 2 | Clinically visible lesion >4.0 cm in greatest dimension |
| Stage IIB | Obvious parametrial involvement |
| Stage III | The carcinoma has extended to the pelvic wall. On rectal examination, there is no cancer-free space between the tumor and the pelvic wall and/or involves the lower third of the vagina and/or causes hydronephrosis or nonfunctioning kidney. |
| Stage IIIA | No extension to the pelvic wall |
| Stage IIIB | Extension to the pelvic wall and/or hydronephrosis or a nonfunctioning kidney |
| Stage IV | The carcinoma has extended beyond the true pelvis or has clinically involved the mucosa of the bladder or rectum. A bullous edema as such does not permit a case to be allotted to stage IV. |
| Stage IVA | Spread of the growth to adjacent organs |
| Stage IVB | Spread to distant organs |
Notes About the Staging
All macroscopically visible lesions, even with superficial invasion, are allotted to stage IB carcinomas. The diagnosis of stages IA 1 and IA 2 should be based on microscopic examination of removed tissue, preferably a cone, which must include the entire lesion. The depth of invasion should not be more than 5 mm, taken from the base of the epithelium—either surface or glandular—from which it originates. The second dimension, the horizontal spread, must not exceed 7 mm. Vascular space involvement, either venous or lymphatic, should not alter the staging but should be specifically recorded because it may affect treatment decisions in the future. Larger lesions should be staged as IB. As a rule, it is impossible to estimate clinically if a cancer of the cervix has extended to the corpus. Extension to the corpus should therefore be disregarded.
A patient with a growth fixed to the pelvic wall by a short and indurated but not nodular parametrium should be allotted to stage IIB. It is impossible at clinical examination to decide whether a smooth and indurated parametrium is truly cancerous or only inflammatory. Therefore, the case should be placed in stage III only if the parametrium is nodular to the pelvic wall or if the growth itself extends to the pelvic wall.
The presence of hydronephrosis or nonfunctioning kidney resulting from stenosis of the ureter by cancer permits a case to be allotted to stage III even if according to the other findings the case should be allotted to stages I or II.
The presence of bullous edema, as such, should not permit a case to be allotted to stage IV. Ridges and furrows into the bladder wall should be interpreted as signs of submucous involvement of the bladder if they remain fixed to the growth at palposcopy (ie, examination from the vagina or the rectum during cystoscopy). Finding malignant cells in cytologic washings from the urinary bladder requires further examination and a biopsy from the wall of the bladder.
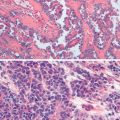
Histopathology
Cases should be classified as carcinomas of the cervix if the primary growth is in the cervix. All histologic types must be included. Grading by any of several methods is encouraged but is not a basis for modifying the stage groupings. When surgery is the primary treatment, the histologic findings permit the case to have pathologic staging as described in Rules for Classification, no. 2. All tumors are to be microscopically verified.
Histopathologic Types
Squamous cell carcinoma in situ
Squamous cell carcinoma
Keratinizing
Nonkeratinizing
Verrucous
Adenocarcinoma in situ
Adenocarcinoma in situ, endocervical type
Endometrioid adenocarcinoma
Clear cell adenocarcinoma
Adenosquamous carcinoma
Adenoid cystic carcinoma
Small cell carcinoma
Undifferentiated carcinoma
Histopathologic Grade
| G1 | Well differentiated |
| G2 | Moderately differentiated |
| G3 | Poorly differentiated |
| G4 | Undifferentiated |
Stage Grouping for the Cervix
| FIGO/AJCC/UICC | T | N | M |
|---|---|---|---|
| 0 | Tis | N0 | M0 |
| IA1 | T1A1 | N0 | M0 |
| IA2 | T1A2 | N0 | M0 |
| IB1 | T1B1 | N0 | M0 |
| IB2 | T1B2 | N0 | M0 |
| IIA | T2A | N0 | M0 |
| IIB | T2B | N0 | M0 |
| IIIA | T3A | N0 | M0 |
| IIIB | T1 | N1 | M0 |
| T2 | N1 | M0 | |
| T3 | N1 | M0 | |
| T3B | Any N | M0 | |
| IVA | T4 | Any N | M0 |
| IVB | Any T | Any N | M1 |
Corpus
Anatomy
1.1 Primary site: The upper two-thirds of the uterus above the level of the internal cervical os is called the corpus. The fallopian tubes enter at the upper lateral corners of a pear-shaped body. The portion of the muscular organ that is above a line joining the tubouterine orifices is often referred to as the fundus.
1.2 Nodal stations: The major lymphatic trunks are the utero-ovarian (infundibulopelvic), parametrial, and presacral, which drain into the hypogastric, external iliac, common iliac, presacral, and paraaortic nodes.
1.3 Metastatic sites: The vagina and lung are the common metastatic sites.
Rules for Classification
The FIGO committee on gynecologic oncology agreed on the system for surgical staging for carcinoma of the corpus uteri at the meeting in Rio de Janeiro in October 1988 with modification made in 2009.
Surgical Staging Classification
| Stage I | Cancer confined to the corpus uteri, including carcinosarcoma | |
| Stage IA | G123 | No or less than half myometrial invasion |
| Stage IB | G123 | Invasion equal to or more than half of the myometrium |
| Stage II | G123 | Tumor invades cervical stroma but does not extend beyond the uterus (endocervical glandular involvement only should be considered as stage I) |
| Stage III | G123 | Local and/or regional spread of the tumor |
| Stage IIIA | G123 | Tumor invades serosa of the corpus uteri and/or adnexa |
| Stage IIIB | G123 | Vaginal metastases and/or parametrial involvement |
| Stage IIIC | G123 | Metastases to pelvic and/or paraaortic lymph nodes |
| Stage IIIC1 | Positive pelvic node | |
| Stage IIIC2 | Positive paraaortic lymph nodes with or without positive pelvic lymph nodes | |
| Stage IV | G123 | Tumor invades bladder and/or bowel mucosa and/or distant metastases |
| Stage IVA | G123 | Tumor invasion of bladder and/or bowel mucosa |
| Stage IVB | Distant metastases, including intraabdominal metastases and/or inguinal lymph nodes |
Notes: Tumor grade, cell type, and presence or absence of malignant cytology in pelvic washings should be reported along with stage.
Abdominal and pelvic peritoneal metastases are stage IVB.
Notes About the Staging
Histopathology—degree of differentiation.
Cases of carcinoma of the corpus should be grouped with regard to the degree of differentiation of the adenocarcinoma as follows:
G1: ≤5% of a nonsquamous or nonmorular solid growth pattern
G2: 6% to 50% of a nonsquamous or nonmorular solid growth pattern
G3: >50% of a nonsquamous or nonmorular solid growth pattern
Notes on Pathologic Grading
- 1.
Notable nuclear atypia, inappropriate for the architectural grade, raises the grade of a grade 1 or 2 tumor by 1.
- 2.
In serous and clear cell adenocarcinomas, nuclear grading takes precedence.
- 3.
Adenocarcinomas with squamous differentiation are graded according to the nuclear grade of the glandular component.
Rules Related to Staging
- 1.
Because corpus cancer is now surgically staged, procedures previously used for determination of stages are no longer applicable, such as the finding of fractional dilatation and curettage (D&C) to differentiate between stages I and II.
- 2.
It is understood that there may be a few patients with corpus cancer who will be treated primarily with radiation therapy. If that is the case, the clinical staging adopted by FIGO in 1971 would still apply, but designation of that staging system would be noted.
- 3.
Ideally, the width of the myometrium should be measured along with the width of tumor invasion.
Histopathology
The histopathologic types are:
- •
Endometrioid carcinoma
- •
Adenocarcinoma
- •
Adenocanthoma (adenocarcinoma with squamous metaplasia)
- •
Adenosquamous carcinoma (mixed adenocarcinoma and squamous cell carcinoma)
- •
Mucinous adenocarcinoma
- •
Serous adenocarcinoma
- •
Clear cell adenocarcinoma
- •
Squamous cell adenocarcinoma
- •
Undifferentiated adenocarcinoma
| FIGO/AJCC/UICC | T | N | M |
|---|---|---|---|
| 0 | Tis | N0 | M0 |
| IA | T1A | N0 | M0 |
| IB | T1B | N0 | M0 |
| IC | T1C | N0 | M0 |
| IIA | T2A | N0 | M0 |
| IIB | T2B | N0 | M0 |
| IIIA | T3A | N0 | M0 |
| IIIB | T3B | N0 | M0 |
| IIIC | T1 | N1 | M0 |
| T2 | N1 | M0 | |
| T3A | N1 | M0 | |
| T3B | N1 | M0 | |
| IVA | T4 | Any N | M0 |
| IVB | Any T | Any N | M1 |
Ovary, Fallopian Tube, and Peritoneal
Anatomy
1.1 Primary site: Ovaries are a pair of solid bodies, flattened ovoids that are 2 to 4 cm in diameter; they are connected by a peritoneal fold to the broad ligament and by the infundibulopelvic ligament to the lateral wall of the pelvis.
1.2 Nodal stations: The lymphatic drainage occurs by the utero-ovarian and round ligament trunks and an external iliac accessory route into the following regional nodes: external iliac; common iliac; hypogastric; lateral sacral; and paraaortic nodes; and, rarely, inguinal nodes.
1.3 Metastatic sites: The peritoneum, including the omentum and pelvic and abdominal viscera, is a common site for seeding. Diaphragmatic involvement and liver metastases are common. Pulmonary and pleural involvement is often seen.
Rules for Classification
Ovarian cancer is surgically staged. Operative findings before tumor debulking determine the stage, which may be modified by histopathologic as well as clinical or radiologic evaluation. Laparotomy and resection of the ovarian mass, as well as hysterectomy, form the basis for staging. Biopsies of all suspicious sites, such as the omentum, mesentery, liver, diaphragm, pelvic, and paraaortic nodes, are required. The final histologic findings after surgery (and cytologic ones when available) should be considered in the staging. Clinical studies, if carcinoma of the ovary is diagnosed, include routine radiology of the chest. CT scanning may be helpful in initial staging and follow-up of tumors.
- 1.
Clinical-diagnostic staging: Although clinical studies similar to those for other sites may be used, the establishment of a diagnosis most often requires a laparotomy, which is most widely accepted in surgical-pathologic staging. Clinical studies, if carcinoma of the ovary is diagnosed, include routine radiography of the chest and abdomen, liver studies, and hemograms.
- 2.
Surgical-evaluative staging: Laparotomy and biopsy of all suspected sites of involvement provide the basis for this type of staging; this staging is often identical to postsurgical staging. Histologic and cytologic data are required.
- 3.
Postsurgical treatment—pathologic staging: This treatment should include laparotomy and resection of ovarian masses as well as a hysterectomy. Biopsies of all suspicious sites, such as the omentum, mesentery, liver, diaphragm, and pelvic and paraaortic nodes, are required. Pleural effusions should be documented by cytology.
- 4.
Retreatment staging: Second-look laparotomies and laparoscopy are being evaluated because of the limitation of routine pelvic and abdominal examinations in detecting early recurrence. Other optional and investigative procedures include ultrasonography and CT scanning. All suspected recurrences need biopsy confirmation.
Staging Classification
Staging is based mainly on findings seen at surgical exploration. Clinical evaluation and imaging studies should be done when appropriate. These findings may affect final staging. The histology is to be considered in the staging, as is cytology as far as effusions are concerned. It is desirable that a biopsy be taken from suspicious areas outside of the pelvis.
| Stage I | Growth limited to the ovaries |
| Stage IA | Growth limited to one ovary; no ascites present containing malignant cells; no tumor on the external surface; capsule intact |
| Stage IB | Growth limited to both ovaries; no ascites present containing malignant cells; no tumor on the external surfaces; capsules intact |
| Stage IC * | Tumor stage IA or IB but with tumor on the surface of one or both ovaries or with capsule ruptured or with ascites present containing malignant cells or with positive peritoneal washings.
|
| Stage II | Growth involving one or both ovaries with pelvic extension |
| Stage IIA | Extension and/or metastases to the uterus and/or tubes |
| Stage IIB | Extension to other pelvic tissues |
| Stage III | Tumor involving one or both ovaries with peritoneal implants outside the pelvis and/or positive retroperitoneal or inguinal nodes; superficial liver metastases equal to stage III; tumor limited to the true pelvis but with histologically proven malignant extension to the small bowel or omentum |
| Stage IIIA | Tumor grossly limited to the true pelvis with negative nodes but with histologically confirmed microscopic seeding of the abdominal peritoneal surfaces and/or retroperitoneal positive retroperitoneal nodes
|
| Stage IIIB | Tumor of one or both ovaries with histologically confirmed implants of abdominal peritoneal surfaces, none exceeding 2 cm in diameter, plus or minus nodes |
| Stage IIIC | Abdominal implants >2 cm in diameter and/or positive retroperitoneal or inguinal nodes. Includes extension to the capsule of the liver or spleen |
| Stage IV | Growth involving one or both ovaries with distant metastases. If pleural effusion is present, there must be positive cytology to allot a case to stage IV. Parenchymal liver metastasis equals stage IV. IVA Pleural effusion only with positive cytology IVB Hepatic and or splenic parenchymal metastasis, metastasis to extraabdominal organs (including inguinal lymph nodes and lymph nodes outside of the abdominal cavity) |
* To evaluate the impact on prognosis of the different criteria for allotting cases to stages IC or IIC, it would be useful to know whether rupture of the capsule was spontaneous or caused by the surgeon and if the source of malignant cells was peritoneal washings or ascites.
Histopathology
The task force of the AJCC endorses the histologic typing of ovarian tumors, as presented in the World Health Organization publication no. 9, 1973, and recommends that all ovarian epithelial tumors be subdivided according to a simplified version. The types recommended are as follows: serous tumors, mucinous tumors, endometrioid tumors, clear cell (mesonephroid) tumors, undifferentiated tumors, and unclassified tumors.
- •
Serous tumors
- •
Benign serous cystadenomas
- •
Of borderline malignancy: serous cystadenomas with proliferating activity of the epithelial cells and nuclear abnormalities but with no infiltrative destructive growth (carcinomas of low potential malignancy)
- •
Serous cystadenocarcinomas
- •
Mucinous tumors
- •
Benign mucinous cystadenomas of borderline malignancy: mucinous cystadenomas with proliferating activity of the epithelial cells and nuclear abnormalities but with no infiltrative destructive growth (carcinomas of low potential malignancy)
- •
Mucinous cystadenocarcinomas
- •
Endometrioid tumors
- •
Benign endometrioid cystadenomas
- •
Endometrioid tumors with proliferating activity of the epithelial cells and nuclear abnormalities but with no infiltrative destructive growth (carcinomas of low potential malignancy)
- •
Endometrioid adenocarcinomas
- •
Clear cell tumors
- •
Benign clear cell tumors
- •
Clear cell tumors with proliferating activity of the epithelial cells and nuclear abnormalities but with no infiltrative destructive growth (low potential malignancy)
- •
Clear cell cystadenocarcinomas
- •
Brenner
- •
Benign Brenner
- •
Borderline malignancy
- •
Malignant
- •
Transitional cell
- •
Undifferentiated carcinomas
- •
A malignant tumor of epithelial structure that is too poorly differentiated to be placed in any other group
- •
Mixed epithelial tumors
These tumors consist of two or more of the five major cell types of common epithelial tumors (types should be specified).
Cases with intraperitoneal carcinoma in which the ovaries appear to be incidentally involved and not the primary origin should be labeled as extraovarian peritoneal carcinoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree