Primary tumor (T)
TX
Primary tumor cannot be assessed
T0
No evidence of primary tumor
Tis
Carcinoma in situ
T1
Tumor = 2 cm in greatest dimension
T2
Tumor > 2 cm but not more than 4 cm in greatest dimension
T3
Tumor > 4 cm in greatest dimension or extension to lingual surface of the epiglottis
T4a
Tumor invades the larynx, deep/extrinsic muscle of the tongue, medial pterygoid, hard palate, or mandible
T4b
Tumor invades lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, or skull base or encases the carotid artery
Regional lymph nodes (N)
NX
Regional nodes cannot be assessed
N0
No regional lymph node metastasis
N1
Metastasis in a single ipsilateral lymph node = 3 cm in greatest dimension
N2a
Metastasis in a single ipsilateral lymph node > 3 cm but not more than 6 cm in greatest dimension
N2b
Metastasis in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension
N2c
Metastasis in bilateral or contralateral lymph nodes, none > 6 cm in greatest dimension
N3
Metastasis in a lymph node > 6 cm in greatest dimension
Distant metastasis (M)
M0
No distant metastasis
M1
Distant metastasis
Table 2
Cancer stage grouping in OSCC
Stage | T | N | M |
|---|---|---|---|
0 | Tis | N0 | M0 |
I | T1 | N0 | M0 |
II | T2 | N0 | M0 |
III | T3 | N0 | M0 |
T1 | N1 | M0 | |
T2 | N1 | M0 | |
T3 | N1 | M0 | |
IVA | T4a | N0 | M0 |
T4a | N1 | M0 | |
T1 | N2 | M0 | |
T2 | N2 | M0 | |
T3 | N2 | M0 | |
T4a | N2 | M0 | |
IVB | T Any | N3 | M0 |
T4b | N Any | M0 | |
IVC | T Any | N Any | M1 |
2 Clinical Differences in HPV-Related OSCC
In addition to molecular-genetic differences, different epidemiology and etiology, HPV relation in OSCC affects the clinical presentation of the patients. For example, secondary primary tumours are reported to be rare in patients with HPV-positive OSCC (Jain et al. 2013), possibly influencing the outcome and recommendations for screening and follow-up in this group of patients. In a retrospective work-up of 232 patients 64 % of toxicity and failure events occurred within the first 6 months of follow-up and the event incidence at each subsequent follow-up has been reported to be below 2 (Frakes et al. 2016). However, some differences reported between HPV- and non-HPV related cohorts are inconsistent. In some published series, patients with HPV-positive cancers were younger (Smith et al. 2004; Klussmann et al. 2003), however, in other reports, the patients were older (Lindel et al. 2001). Summarized, patients with HPV positive OSCC probably are younger by approximately 5 years when compared with HPV negative patients. According to gender, men are reported to be at equal risk to women, however, slightly higher proportions of males or females in HPV-positive OSCC patients have both been reported. The majority of HPV-positive tumors usually arise from the lateral and anterior wall of oropharynx, compared with other anatomic subsites. Histopathologically, HPV-positive tumors tend to reveal a poorly differentiated, frequently basaloid and nonkeratinizing histology. The patients have commonly a shorter history of tobacco and alcohol consumption and usually have a better performance status compared to the HPV-negative patients.
3 TNM Staging: Clinical Presentation in HPV-Related OSCC
A common presentation of HPV-related OSCC is represented by a small primary tumor along with advanced nodal disease (Fig. 1). Nodal disease in HPV-related OSCC is often predominantly cystic on imaging (Goldenberg et al. 2008). However, HPV-positive OSCC have also been reported to have lower T-category (Porceddu et al. 2011) or to show no difference in size of the primary tumor (Hafkamp et al. 2009). Concerning regional metastases, most studies have noted higher nodal involvement in HPV-positive tumors but some authors have found no difference in N classification. In the majority of published papers HPV-related OSCC presents with a more advanced clinical stage, particularly with higher nodal involvement, when compared to non-HPV driven counterparts. According to this, HPV-related primary tumors may remain clinically occult, and often present with lymph node metastases only. For instance, tonsil SCCs are long known to present with early lymph node metastases (Thompson and Heffner 1998).
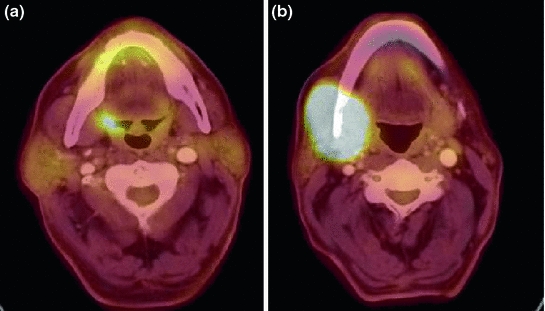
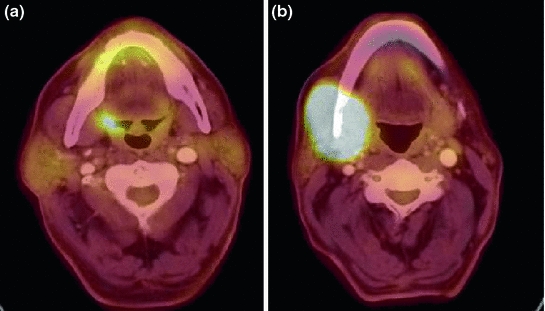
Fig. 1
Clinical presentaion of HPV-related OSCC typically includes a small primary tumor (a) in combination with advanced regional disease (b)
In our series of consecutive patients between 2000 and 2009, HPV-positive tumors had more often limited T-stages and advanced N- and M-stages (Table 3). In a further analysis of 266 patients, the differences of TNM staging according to HPV status has also been described. Patients with HPV-positive tumors were more likely to present with stage III/IV tumors (HPV-positive 93 % vs. HPV-negative 65 %; p < 0.001). A difference in T-classification was respectively not described, however, advanced stage HPV-positive OSCC were more likely to be either T1 or T2 than those that were HPV-negative (Ward et al. 2015). In agreement with both reports, the advanced stage in HPV-related OSCC is predominantly a result of nodal involvement. The study population of a large cohort treated with radiotherapy with or without chemotherapy consisted of 573 HPV-related OSCC yielding AJCC stages: I/n = 8; II/n = 25; III/n = 79; IV/n = 461). This fact later has been criticised, because only eight (1 %) patients had stage I disease and 25 (4 %) patients had stage II disease, which raised the question of whether the sample sizes for stages I and II were adequate. However, this rarity of stage I and II may particularly represent the nature of HPV-related OSCC. In a different analysis of almost 2000 OSCC patients, only 2 and 4 % were stage I and II, and stage I and II were also uncommon among >13,000 OSCCs in the SEER database (Setton et al. 2015; Keane et al. 2015).
Table 3
Tumor characteristics according to HPV-association (n = 396)
All (N = 396) | HPV-unrelated (N = 305) | HPV-related (N = 75) | p-value* | |||
|---|---|---|---|---|---|---|
N | % | N | % | |||
T–stage | ||||||
T1-2 | 187 (47.2 %) | 132 | 72.1 | 51 | 27.9 | 0.009 |
T3 | 88 (22.2 %) | 76 | 87.4 | 11 | 12.6 | |
T4a/b | 115 (29.0 %) | 93 | 88.6 | 12 | 11.4 | |
Unknown | 6 (1.5 %) | |||||
N–stage | ||||||
N0 | 103 (26.0 %) | 88 | 88.9 | 11 | 11.1 | 0.010 |
N+ | 283 (71.5 %) | 209 | 76.8 | 63 | 23.2 | |
Unknown | 10 (2.5 %) | |||||
M–stage
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| ||||||