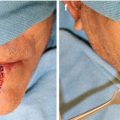
Fig. 4.1
A centrally located lower lip squamous cell carcinoma in a patient with fair skin and red hair. Note the rolled border and necrotic center typical of squamous cell carcinoma
There is a linear relationship between the incidence of skin cancer and geographic latitude. UVR exposure is greater in latitudes closer to the equator and a direct correlation has been demonstrated in the incidence of both squamous cell carcinoma and basal cell carcinoma. Supporting this hypothesis is an inverse relationship whereby cancer incidence decreases as one moves further from the equator [24]. Latitude and measured UVB radiation has a stronger causative relationship with SCC than BCC [8]. Data from populations that have migrated have illustrated several at-risk populations and furthermore confirmed the cumulative effect of sun exposure. English and Welsh migrants to New Zealand developed higher rates of lip cancer [27]. On the other hand, English migrants to Australia developed less cancer than native Australians, implicating cumulative sun exposure as a risk factor as well. People living in regions with high levels of UVR and remain there over time are more likely to develop multiple non-melanomatous skin cancers. It has been posited that childhood exposure alone is a critical factor in the development of skin cancer; however, Wei-Passanese et al. clearly demonstrate that continued adult exposure to UVR is essential in the development of skin cancer [29].
Ultraviolet radiation has long been known to be critical element in the evolution of non-melanomatous skin and lip cancer through its demonstrable mutagenic effects. UVR is likely responsible for all the carcinogenic effects of sunlight [12]. The exact wavelength of light that induces cancer through genetic alterations is unclear. Visible light and UVR reach the earth, with some wavelengths being filtered through atmospheric transmission. UVA and UVB light have both been considered in the pathogenesis of skin cancer. However, UVB (280–315 nm) appears to be much more effective at producing DNA damage and cancer in animals than UVA (315–400 nm). Wavelengths of 340 nm and greater are far less potent in causing cancer in experimental animals than wavelengths of about 295 nm [8]. Epidemiologic studies do not allow for stratification of wavelengths of light and incidence of cancer, and sunlight is generically substituted for UVB/UVA exposure in most retrospective studies.
The pathway from sun-damaged skin to the development of SCC of the lip is frequently met with a phenotypic lesion presenting as solar or actinic keratosis (AK). AK represents an early clinical stage of cutaneous premalignancy which may ultimately progress to cancer; likewise, actinic or solar cheiloses (AC) represent actinic keratosis occurring on the lip vermilion. AKs are frequently multiple and on average individuals harbor 6–8 lesions which are found on sun-exposed regions of the body and are sometimes comingled with histologically confirmed SCC. AKs and ACs both arise from cumulative exposure to UVR. Malignant transformation rate estimates vary widely 0.15–80 % illustrating diversity in tumor behavior and host response [22].
Malignant transformation frequently involves tumor suppressor gene(s) mutation or inactivation and proto-oncogene(s) activation. The number of accumulated genetic mutations required for malignant transformation for each tumor is not known, but is thought to be as few as two in models of human skin cancer [6]. The molecular consequences of UVR have been partially elucidated. DNA photoproducts are chemical changes within the structure of DNA, which if not repaired prior to cell division portent mutagenic potential. The most common mutations are DNA base changes at dipyrimidine sites [13]. p53 mutations, perhaps the mostly ubiquitous tumor suppressor implicated in human malignancies, occur in nearly 90 % of SCC and half of BCC [31]. UVB has been implicated in the induction of genomic instability of p53, and nearly 60 % of SCC contain signature base change transitions [4]. p53 mutations are also known to occur in dysplastic tissues as well as otherwise histological normal epithelium. Such tumor suppressor mutations are directly correlation with sun-exposed skin. Nearly three-quarters of sun-exposed skin harbor p53 mutations compared to 5 % in nonexposed skin [18]. Other relevant pathways include the abnormal activation of the epidermal growth factor receptor (EGFR) and the SFK family of tyrosine kinases, which are thought to alter p53 [15]. It has also been shown that loss of heterozygosity occurs prior to malignant transformation and is found in the dysplastic stage of AK [23].
The role of tobacco in the development of lip cancer is less clearly defined, yet the general consensus is that to some degree it increases the risk of developing lip cancer. There does appear to be a relationship between both cigarette use and pipe use in developing lip cancer. Spitzer et al. reported a higher incidence of lip cancer in pipe smokers than users of other types of tobacco [26]. It has further been postulated that the heat effect of pipe smoking may be a contributing factor. More recent evidence has confirmed an independent effect of tobacco smoking that is dose related. The habit of leaving the cigarette in contact with the lip while smoking is a unique risk factor that is independent on the amount smoked or types cigarette (filter/non-filtered) [20]. Right-handed smokers tend to develop cancer on the right region of the lower lip. Alcohol consumption has synergistic effect in developing SCC with smoking in the oral cavity, and this may be extrapolated for lip cancers [3]. It is likely that tobacco, alcohol, and sun-exposure all play a role in lip cancer in susceptible individuals moreover that UVR may increase the mutagenic effects of tobacco.
Immunosuppression either acquired or medically induced has been shown to be a risk factor for lip and skin cancers. The risk is increased 60- to 100-fold in solid organ transplant patients [2]. Lip cancer is the most common tumor found in renal transplant recipients with an incidence that ranges from 2 to 22.9 % [17]. Lip cancer is considered by some to be an immunodeficiency-related cancer; furthermore, cessation of immunotherapy reverses the risk incurred by antirejection medications [28]. Risk appears related to the type of immunotherapy, dose, and duration. Azathioprine and cyclosporine are common drugs used in the post-transplant setting to prevent organ rejection. Azathioprine has been shown to increase UVA light photosensitivity, and while UVA does not directly cause lip or skin cancer, it is thought that it induces a state of increased oxidative stress giving rise to mutagenic free radicals [19]. Cyclosporine has a tumorigenic effect that is independent of its immunomodulating properties. The mechanism by which cyclosporine increased lip cancer is not fully understood; however, it has been shown to counteract p53-dependant cellular senescence [30]. There is no current evidence to suggest that HIV/AIDS patients incur additional risk for skin or lip cancer given their immunosuppressed state.
Recently, additional commonly used pharmaceutical agents have come under scrutiny in their putative role in the development of lip and skin cancer. Voriconazole, a second-generation triazole antifungal agent, does not have known immunomodulating properties, but is commonly employed in the immunosuppressed population. A case-control study of lung transplant recipients has implicated voriconazole in the development of some skin cancers. The mechanism is unclear; however, it has been posited that voriconazole may exhibit a drug-mediated photosensitivity through a primary metabolite that can absorb both UVA and UVB wavelengths [5]. Photosensitizing antihypertensive drugs including thiazide diuretics, triamterene, and some angiotensin-converting enzyme inhibitors have recently been evaluated in relation to lip cancer in non-Hispanic males. These drugs are thought to induce genetic mutations through the generation of free radicals produced when they absorb both visible light and UVR. In a matched-case controlled study, Freidman et al. showed increase risk of lip cancer ranging from 2.5 to 4.22 in patients taking photosensitizing antihypertensive drugs either alone or in combination form.
4.3 Staging
Lip cancer per se includes neoplasms of the vermilion border of lip, the oral commissure, and labial mucosa, but specifically excludes lesions arising primarily from the skin of lip. Oncologic staging for lip cancers follows the common accepted regimen from the American Joint Committee on Cancer (AJCC) and is grouped with oral cancers. The value of any staging system can be measured by several factors. The current AJCC staging manual groups two very different diseases together based on anatomic proximity. The multitude of differences between oral cavity and lip cancer begs the value of separate staging regimens. The incidence of lip cancer according to the most recent SEER analysis (2003–2007) showed an incidence of 0.7/100,000 per year; the male to female ratio was 4:1, and a worldwide decline has been seen in most registries in the world. The majority of lip cancers are preceded by a preexisting lesion. The early clinical manifestation can be subtle and are often ignored by patients despite their accessibility for daily examination. The most common clinical presentation of AC is a white, dry, scaling plaque that has tactile similarity to sandpaper, even through a gloved finger [14]. Other signs of underlying suspicious lesions include loss of normal lip architecture and the inability to identify the vermilion. Plaques of variable color including white, gray, or brown should also raise suspicion (Fig. 4.2). Nodular or ulcerative lesions in any form should raise the concern for SCC. Lesions that fail to heal or bleed, either spontaneously or with little manipulation, should also be considered high risk (Fig. 4.3). The transformation risk of AC is greater than its cutaneous counterpart. Interestingly, the risk of cervical metastasis in SCC arising in AC is less than those that arise de novo [1]. Early diagnosis and treatment can prevent malignant transformation yielding higher survival rates.