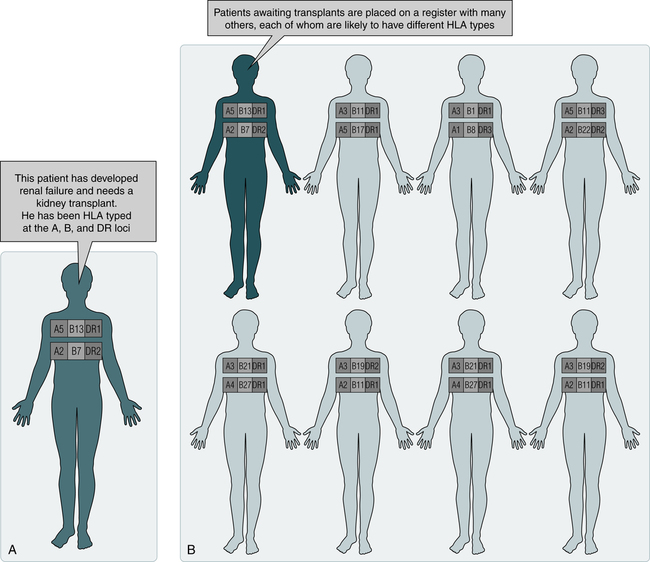
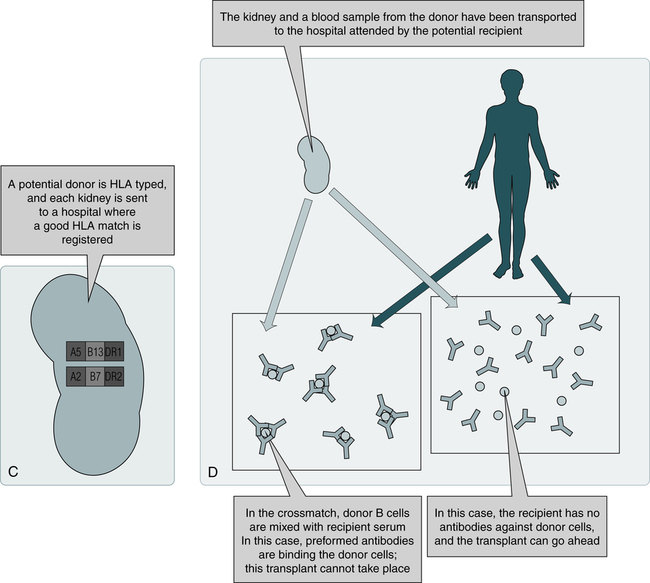
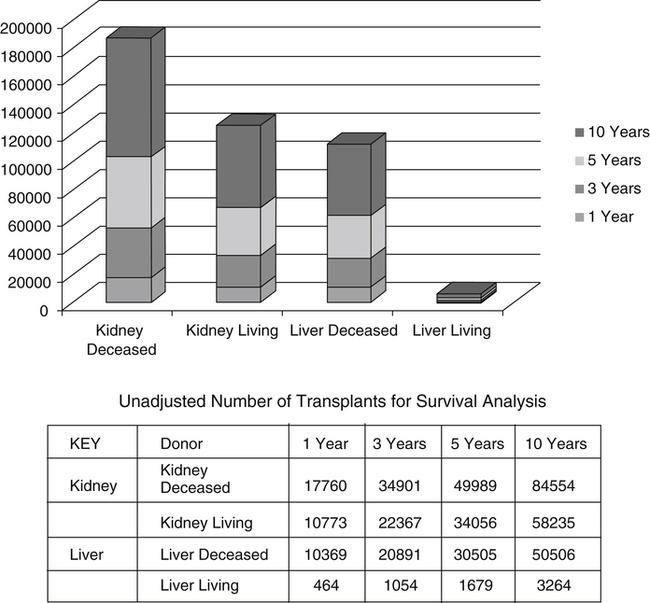
At the conclusion of this chapter, the reader should be able to: • Identify and describe the histocompatibility antigens. • Explain the clinical applications of histocompatibility antigens and human leukocyte antigens. • Identify and describe several laboratory methods for evaluating potential transplant recipients and donors. • List frequently used terms in transplantation. • Identify various types of transplants. • Define graft-versus-host disease. • Explain the etiology, epidemiology, signs and symptoms, manifestations, diagnosis, and prevention of graft-versus-host disease. • Describe the types of graft rejection. • Briefly explain the mechanism of organ or tissue rejection. • Identify and explain some methods of immunosuppression. • Analyze a representative transplantation case study. • Correctly answer case study related multiple choice questions. • Be prepared to participate in a discussion of critical thinking questions. • Explain the principle and application of the Longitudinal Assessment of Posttransplant Protocol. At present, a variety of tissues and organs are transplanted in human beings, including bone marrow, peripheral stem cells, bone matrix, skin, kidneys, liver, cardiac valves, heart, pancreas, corneas, and lungs. Transplantation is one of the areas, in addition to hypersensitivity (Chapter 26) and autoimmunity (Chapter 28), in which the immune system functions in a detrimental way. Transplantation presents the following two basic problems. • Genetic variation between donor and recipient • Recognition of genetic differences by a transplant recipient’s immune system that causes rejection of a transplanted organ The major histocompatibility complex (MHC) is a cluster of genes found on the short arm of chromosome 6 at band 21 (6p21; see Fig 2-1). These genes code for proteins that have a role in immune recognition. Each HLA allele has a unique four-, six-, or eight-letter or digit name (Table 31-1). The length of the allele designation depends on the sequence of the allele and that of its nearest relative. All alleles receive a four-letter or digit name; six- and eight-digit names are only assigned when necessary. Table 31-1 ∗As of June 2007, no alleles have been named with the “C” or “A” suffixes. The MHC is divided into four major regions (Table 31-2)—D, B, C, and A. The A, B, and C regions are the classic or class Ia genes that code for class I molecules. The D region codes for class II molecules. Class I includes HLA-A, B, and C. The three principal loci (A, B, and C) and their respective antigens are numbered 1, 2, 3, and so on. The class II gene region antigens are encoded in the HLA-D region and can be subdivided into three families, HLA-DR, HLA-DC (DQ), and HLA-SB (DP). Table 31-2 Examples of Nomenclature of HLA Alleles Adapted from Peakman M, Vergani D: Basic and clinical immunology, ed 2, New York, 2009, Churchill Livingstone. Structurally, there are two classes of HLA molecules, class I and class II (Table 31-3). Both classes are cell surface heterodimeric structures. Class I HLA molecules consist of an alpha chain, a highly polymorphic glycoprotein, encoded within the MHC on chromosome 6. This alpha chain noncovalently associates with beta-2 microglobulin, a nonpolymorphic glycoprotein, encoded by a non-HLA gene on chromosome 15. Class II HLA molecules are composed of alpha chains and beta chains encoded within the MHC. The conformation of class I and class II HLA molecules provides each with a groove in which linear peptides, consisting of 8 to 25 peptides, are displayed for recognition by the cell surface expression on lymphocytes of a transmembrane heterodimeric receptor. All nucleated cells of the body display transmembrane class I HLA molecules in association with the non–transmembrane beta-2 microglobulin molecule. Table 31-3 Comparison of Major Histocompatibility Complex Class I and Class II HLA testing has increasingly been used as a diagnostic and genetic counseling tool. Knowledge of HLA antigens and their linkage has become important because of the recognized association of certain antigens (Box 31-1) with distinct immunologic-mediated reactions, autoimmune diseases, some neoplasms, and other disorders; these disorders, although nonimmunologic, are influenced by non-HLA genes also located within the major MHC region. The estimated relative risks or chances of developing a disease if a given antigen is present may be elevated in individuals bearing certain HLA antigens compared to individuals who lack the antigen (Table 31-4). The HLA-B27 antigen is the only HLA antigen with a disease association strong enough to be useful in differential diagnosis. Although the degree of association between HLA antigens and other diseases may be statistically significant, it is not strong enough to be of diagnostic or prognostic value. Table 31-4 Relationship of Human Leukocyte Antigens to Risk of Disease ∗Increased risk of developing the disease over a lifetime. †Varies with ethnic group (e.g., 3× for Pima Indians and 300× for Japanese). Adapted from Ashman RF: Rheumatic diseases. In Lawlor GJ, Fischer TJ, editors: Manual of allergy and immunology, ed 2, Boston, 1998, Little, Brown. A potential recipient needs to have HLA typing (Fig. 31-1, A). A family search may be conducted for a suitable donor. If a suitable match is not found, the patient is placed on a waiting list (see Fig. 31-1, B). When an organ becomes available, the donor is HLA-typed and a computerized search is made for a suitable recipient (see Fig. 31-1, C). Because different individuals in a species carry different HLA antigens on their cell surfaces, introduction of foreign antigens can stimulate T cells. These T cells are prominently implicated in graft rejection, and they can also stimulate antibody formation under certain circumstances. Histocompatibility crossmatching is performed to rule out preexisting antibodies capable of causing hyperacute rejection (see Fig. 31-1, D). Single-cell analysis by flow cytometry is the most sensitive method for crossmatching and antibody identification (see Chapter 13). Tagged T or B lymphocytes are incubated with the patient’s serum to allow the formation of antigen-antibody complexes on the cell surface. Unbound proteins are washed away and the bound antibodies are detected with a second antibody, anti–human immunoglobulin G (IgG) labeled with a chromophore. An alternative flow cytometry format uses microparticles coated with HLA antigens of known specificity (obtained through recombinant techniques) instead of lymphocytes. How long a patient waits for a transplant depends on the following factors: • Blood type (some rarer than others) • Height and weight of transplant candidate • Distance between donor’s hospital and potential donor organ • Number of donors in local area over time • Transplantation center’s criteria for accepting organ offers Depending on the type of organ needed, some factors are more important than others. On March 22, 2012, the United Network for Organ Sharing patient waiting list contained 113,612 names. The list continues to grow because of the scarcity of organs (Box 31-2). Most of these registrants are waiting for a kidney transplant, followed by those waiting for a liver transplant and heart transplant. Other transplant registrants are waiting for lung, kidney and pancreas, pancreas, pancreatic islet cell, heart and lung, and intestine. Approximately 25% of patients waiting for a liver transplant are children younger than 10 years. The number of patients living with a function graft has generally increased over the last decade. Graft survival time depends on many factors, including the type of organ transplanted (Fig. 31-2 and Table 31-5). Table 31-5 Tx = year or inclusive years of tranplantation. Source: Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR). OPTN / SRTR 2010 Annual Data Report. Rockville, MD: Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation; 2011. www.srtr.org/annual_reports/2010 The transplanting or grafting of an organ or tissue ranges from self-transplantation, such as skin grafts from one part of the body to another to correct burn injuries, or hair transplants from one area of the scalp to another to correct pattern baldness, to the grafting of a body component from one species to another, such as transplanting a pig’s heart valve to a human. Table 31-6 defines the most recent terms used in transplantation. Table 31-6 Eleven different organs or human body parts can be transplanted—blood vessels, bone, bone marrow or stem cells (see Chapter 32), cornea, heart, kidneys, liver, lung, middle ear, pancreas, and skin. Successful organ transplants have increased since the advent of the immunosuppressive drug cyclosporine (cyclosporin A).
Solid Organ Transplantation
Histocompatibility Antigens
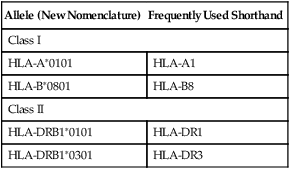
Nomenclature of Human Leukocyte Antigen Alleles
Nomenclature
Indicates
HLA
Human leukocyte antigen (HLA) region and prefix for an HLA gene
HLA-DRB1
Particular HLA locus (e.g., DRB1)
HLA-DRB1∗13
Group of alleles that encode the DR13 antigen
HLA-DRB1∗1301
Specific HLA allele
HLA-DRB1∗1301N
Null allele
HLA-DRB1∗130102
Allele that differs by a synonymous mutation
HLA-DRB1∗13010102
Allele that contains a mutation outside the coding region
HLA-A∗2409N
Null allele
HLA-A∗3014L
Allele encoding a protein with significantly reduced or low cell surface expression
HLA-A∗24020102L
Allele encoding a protein with significantly reduced or low cell surface expression, where the mutation is found outside the coding region
HLA-B∗44020102S
Allele encoding a protein expressed as a secreted molecule only
HLA-A∗3211Q
Allele that has a mutation previously shown to have a significant effect on cell surface expression, but where this has not been confirmed and its expression remains questionable
Major Histocompatibility Complex Regions
Allele (New Nomenclature)
Frequently Used Shorthand
Class I
HLA-A∗0101
HLA-A1
HLA-B∗0801
HLA-B8
Class II
HLA-DRB1∗0101
HLA-DR1
HLA-DRB1∗0301
HLA-DR3
Classes of Human Leukocyte Antigen Molecules
Parameter
Class I
Class II
Loci
HLA-A, B, and C
HLA-DN, DO, DP, DQ, and DR
Distribution
Most nucleated cells
B lymphocytes, macrophages, other antigen-presenting cells, activated T lymphocytes
Function
To present endogenous antigen to cytotoxic T lymphocytes
To present endogenous antigen to helper T lymphocytes
Human Leukocyte Antigen Applications
Antigen Present
Related Disease
Risk∗
B27
Ankylosing spondylitis
Reiter’s syndrome
Anterior uveitis
Arthritic infection with Yersinia or Salmonella
Psoriatic arthritis with spinal involvement
Spondylitis associated with inflammatory bowel disease
Juvenile chronic arthritis with spinal involvement
100׆
40×
25×
20×
11×
9×
5×
B8
Celiac disease
Addison’s disease
Myasthenia gravis
Dermatitis herpetiformis
Chronic active hepatitis
Sjögren’s syndrome
Diabetes mellitus (insulin dependent)
Thyrotoxicosis
9×
6×
5×
4×
4×
3×
2×
2×
B5
Behçet’s syndrome
6×
BW38
Psoriatic arthritis
7×
BW15
Diabetes mellitus (insulin-dependent)
3×
DR2
Goodpasture’s syndrome
Multiple sclerosis
16×
4×
DR3
Gluten-sensitive enteropathy
Dermatitis herpetiformis
Subacute cutaneous lupus erythematosus
Addison’s disease
Sjögren’s syndrome (primary)
21×
14×
12×
11×
10×
DR4
Pemphigus‡
Giant cell arthritis
Rheumatoid arthritis
Juvenile (insulin-dependent) diabetes mellitus
32×
8×
6×
5×
DR5
Pauciarticular juvenile arthritis
Scleroderma
Hashimoto’s thyroiditis
5×
5×
3×
Laboratory Evaluation of Potential Transplant Recipients and Donors
Human Leukocyte Antigen Typing
Histocompatibility Testing
Flow Cytometry
Facts About Solid Organ Transplantation
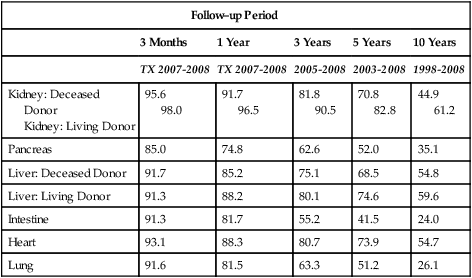
Follow–up Period
3 Months
1 Year
3 Years
5 Years
10 Years
TX 2007-2008
TX 2007-2008
2005-2008
2003-2008
1998-2008
Kidney: Deceased
Donor
Kidney: Living Donor
95.6
98.0
91.7
96.5
81.8
90.5
70.8
82.8
44.9
61.2
Pancreas
85.0
74.8
62.6
52.0
35.1
Liver: Deceased Donor
91.7
85.2
75.1
68.5
54.8
Liver: Living Donor
91.3
88.2
80.1
74.6
59.6
Intestine
91.3
81.7
55.2
41.5
24.0
Heart
93.1
88.3
80.7
73.9
54.7
Lung
91.6
81.5
63.3
51.2
26.1
Transplantation Terminology
Term
Definition
Autograft
Graft transferred from one position to another in the same individual (e.g., skin, hair, bone)
Syngraft
Graft transplanted between different but identical recipient and donor (e.g., kidney transplant between monozygous twins)
Allograft (homograft)
Graft between genetically different recipient and donor of the same species; grafted donor tissue or organ contains antigens not present in recipient
Xenograft (heterograft)
Graft between individuals of different species (e.g., pig heart valve to a human heart)
Types of Transplants
Solid Organ Transplantation