Chapter 7 SOCIAL ISSUES
INTRODUCTION
When exploring the mental health problems of older people, the extent to which they are exacerbated by social issues is as important as what results from biological factors. The opening section of this chapter concentrates on ageism and how this affects an older person’s self-esteem. This negative attitude directed at older people adds another layer of stress in an already stressful period of life. Women have a greater life expectancy than men, although the downside of this fact is having a greater propensity for the less desirable aspects of ageing, such as poor health and social isolation. Marital status also influences mental health outcomes for older people in relation to social and supportive relationships and how these interact. The chapter concludes with a discussion on mental health issues for non-heterosexual older people, an often-overlooked topic.
AGEISM
Understanding the concept of ageism and how it affects older people is one of the fundamental issues of working with older people. Butler (2009, p 211) describes ageism as ‘age prejudice’, which relates to the prejudice and stereotypes that are applied to older people solely on the basis of their age. This type of discrimination, where older people are seen as somehow inferior to others, is very prevalent and pervades all aspects of daily life. It includes disparaging remarks that dismiss and belittle older people, adverse media portrayals, the poor design of goods and services, and broader political agendas.
A good example of ageism was found in recent research conducted into mental health services by the UK Healthcare Commission (2009). This study revealed that older people have less access to psychological therapies, out-of-hours and crisis mental health services, and alcohol services. More damning were the findings that there was an ‘unjustified reluctance’ to take referrals for older people and particularly those with dementia. Ageism affects people personally, socially, culturally and economically. It prevents people from receiving adequate healthcare and reduces their opportunity to fully participate in their communities. This attitude is particularly prevalent in Western societies, and people from other cultural backgrounds are often surprised at the limited degree of respect afforded to older people in countries such as Australia.
Ageist attitudes are formed through stereotyping. A stereotype is:
… an exaggerated, superimposed and generalised portrayal of a group. It involves the adoption of an oversimplified, narrow and standardised image to explain the behaviour or characteristics of individuals and groups (Germov 1998, p 353).
Stereotypes can be positive or negative, and they can be damaging. Positive stereotyping can take the form of older people always being seen as wise and trustworthy with many life experiences to call upon in times of need. Negative stereotyping occurs when older people are seen as old fashioned, slow, demented, unproductive and incapable of making important decisions. Both positive and negative stereotyping can create problems when caring for older people. As a mental health worker, it is necessary to examine one’s own values and beliefs in relation to this topic. This can be done through professional supervision or undertaking value clarification exercises, which are available on the internet or in textbooks (Stein-Parbury 2009).
Identifying, not accepting, and challenging ageism should be the cornerstone for community-based care. Other strategies include valuing and respecting individuality, being mindful of older people’s dignity, being committed to equality and diversity, showing kindness and compassion about any abnormal behaviours, communicating effectively and respectfully, and promoting a healthy lifestyle for older people (Nursing and Midwifery Council 2009).
GENDER
With regard to social issues, the differences between older men and older women are quite marked. First, women have a longer life expectancy than men. For the age group 65–85 years of age, women outnumber men by three to one, and this ratio increases in the 85+ age group where women outnumber men by six to one. The life expectancy for women is 86.1 years of age, whereas it is 82.5 years for men (Australian Institute of Health and Welfare 2007). A longer life expectancy can mean greater exposure to losses associated with health, family and friends, and living a significant period of life with some form of chronic disability or illness. For a man, living longer could mean finding himself in a world surrounded by women, which may not concern some men, but finding someone to share confidences may be difficult, thereby increasing a sense of isolation.
A significant number of older women have poor socioeconomic circumstances and often live below the poverty line (Butler 2009). This is usually a reflection of an absent work history or one characterised by low wages, interrupted careers for the purposes of childbearing and rearing, and lower superannuation entitlements. Widowhood, living alone and inadequate income are all predictors of poorer psychological outcomes in later life.
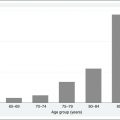
An overrepresentation of women will be particularly noticeable in the ‘old old’ age group (>80 years of age). It is predicted that this group will double in size over the next two decades and triple during the next 50 years to comprise more than 9% of the Australian population or 2.3 million people in 2051. In 2008, there were 3400 people aged 100 years and over, and this figure alone is projected to grow to 40,000 people by 2051 (Australian Bureau of Statistics 2008). This group of very old people will have special needs in relation to physical and mental health.
In regard to their mental health, older people commonly underreport their symptoms or express distress through somatic symptoms like headache or tiredness, and therefore often do not receive an appropriate diagnosis. Although women are more likely than men to seek help in relation to difficulties created by mental health problems, when compared with their younger counterparts (24–65-year-olds), older women are less likely to seek treatment and, when they do get treatment, it is often given at a lesser level. Treatment is usually sought in the general healthcare sector, rather than the specialised mental health services (Australian Institute of Health and Welfare 2008).
This difference between men and women is also reflected in specific disorders, such as anxiety and depression, where prevalence rates are twice as high for women as for men (Australian Bureau of Statistics 1997, Bergdahl et al 2007). In relation to dementia, it is thought the higher prevalence in women can be explained by the fact that many more women live to the age when dementia is more prevalent and women with dementia tend to live longer as well (Australian Institute of Health and Welfare 2006). One area where men feature more predominantly is with suicide rates. For many years, older men had the highest rates of suicide, which has only recently been surpassed by 15–34-year-old males (De Leo et al 2001).
Older women are also more prone to late-onset schizophrenia than older men (Castle 2005). This gender disparity has not yet been fully explained, but it usually occurs in socially isolated women who have remained undiagnosed for a considerable period of time. The symptom profile is generally mild. These older women usually only come to the attention of mental health services when neighbours become worried or the police are called on a regular basis because, for example, the older woman believes she has an ‘intruder’, which is really symptomatic of a persecutory delusion. Although the symptoms are usually distressing, they can be treated pharmacologically with good outcomes. However, this should be done cautiously and with some form of social support. Hassett (1998) gave a classic example of such a situation in her paper about an older lady who believed she had a plumber in her roof. Hassett warned against being too aggressive in treatment. Dealing with the ‘delusion’ often occupies a lot of time for the older person and, once this is removed, they can lose a sense of purpose and become vulnerable to depression.
Just as important as diagnosed disorders are the underdiagnosed disorders. For example, older women are often undiagnosed in the areas of alcohol abuse, and prescription (especially benzodiazepines) and over-the-counter medication abuse. The Australian National Drug Strategy Household Survey (Australian Bureau of Statistics 2001) found that on a daily basis, 40% of older women consumed over-the-counter medications. Such medications could easily be taken for psychological distress as well as physical problems. For men, on the other hand, excess alcohol consumption remains a major form of substance abuse, which often occurs with a mood disorder.
Women are the primary users of mental health services. They have twice the rate of anxiety and depression and are more willing to seek treatment. Traditionally, men negate concerns about their health and therefore their usage of health services is much lower than women. This not only happens when they are acutely ill, but they are also less likely to take preventive health actions or comply with health regimes. Reasons for this are embedded in how a society constructs the notion of masculinity (e.g. men should be in control of their emotions and not succumb to sickness). A depressive illness can be particularly damaging for the male psyche because the symptoms of the illness make a presentation that is in opposition to the stereotypical image of a ‘male’ (Emslie et al 2006).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree