Figure 19.1
Incisions used for small bowel neuroendocrine tumor (SBNET) resection. If only the small bowel tumor, regional nodes, and gallbladder are to be resected, then a 5- to 6-inch midline incision may be used (solid line). If more extensive surgery is required, including extended nodal dissection, removal of peritoneal implants, or hepatic cytoreduction, then a long midline incision is preferred (solid and dotted lines)
19.2.2 Exploring the Abdomen
Once the peritoneal cavity is entered, a thorough exploration is carried out. This exploration begins with division of the falciform ligament, followed by careful bimanual palpation of both the right and left lobes of the liver. Liver metastases are very common, occurring in 30% of cases of SBNETs in the Surveillance, Epidemiology, and End Results (SEER) Program registries [3] and in 77% of our patients at a tertiary referral center [2]. Compare the intraoperative findings with the results of preoperative imaging, including CT scans and octreoscans, where available. Assess whether the liver disease, if present, consists of relatively few, large lesions, which may be amenable to debulking, or whether there are numerous, small lesions in both lobes, where it will be difficult to make a substantive impact on reducing the tumor burden. Also assess whether many of the lesions are peripheral and subcapsular (and therefore amenable to enucleation) or deep, requiring formal resection or ablation.
Next, palpate the gallbladder for stones, palpate the hepatoduodenal ligament for enlarged nodes, and assess for aberrant hepatic arterial anatomy. Palpate the stomach and then the duodenum for any intramural or serosal nodules. Feel the peritoneal surfaces under each diaphragm for nodularity, and then run a hand down along the anterior peritoneum and lateral peritoneal surfaces, and then to the pelvis. Feel for the catheter balloon in the bladder, and then follow the sigmoid down for lesions known as drop metastases. When the peritoneal reflection is reached, feel anteriorly for the uterus and then each ovary in female patients. Enlarged, hard ovaries are likely to represent metastases and should be removed, especially in postmenopausal women. Follow the sigmoid colon with your hand up to the splenic flexure, palpating for lesions, then across the transverse colon, then down the ascending colon to the appendix.
Locate the ligament of Treitz; then pull the jejunum upward and carefully inspect and palpate the entire small bowel to the ileocecal valve, grasping the bowel between thumb and forefinger and methodically pulling the bowel through these fingers, palpating for intramural lesions (Fig. 19.2). Lesions as small as 1–2 mm can be detected, but most tumors will be between 5 and 15 mm in size. Pull 10–15 cm of bowel through the fingers of the left hand while firmly grasping the starting point with the right hand; then re-grasp the bowel distally with the right hand adjacent to the left, and pull the next 10–15 cm through; repeat until the ileocecal valve is encountered, which is generally 300–600 cm from the ligament of Treitz. Most lesions will be in the distal jejunum to the terminal ileum; it is rare to find lesions in the proximal part of the jejunum. Multiple lesions are found in 30–40% of patients; if several lesions are encountered, place a 3-0 silk suture in the serosa of the bowel adjacent to each one. If there are many lesions (the most I have found is 139), then place a suture just proximal and distal to the first and last ones. We measure and record the total length of the small bowel and the segment of bowel affected by both the tumor(s) and lymphadenopathy, which helps in planning the resection.
Palpate the mesentery supplying the bowel adjacent to the lesions you have found, to locate grossly enlarged nodes (Fig. 19.3). Assess their size and compare them with the preoperative CT scan, which commonly shows enlarged nodes with calcification in the small bowel mesentery. Carefully follow the mesenteric vessels on the CT scan and look for enlarged nodes proximally, which can extend up to the lower border of the pancreas and may encircle the SMV and SMA. Now assess the mesentery for the most proximal extent of enlarged or firm nodes, and note their relationship to major vascular branches (such as the ileocolic) versus more central and critical vessels such as the SMV and SMA. The nodes may be matted down and pulling loops of bowel into them, as well as being heavily calcified and thick. Determine the relationship between these nodes and the lesion(s) within the bowel, and how these will be removed together. If multiple loops of bowel are adherent to the nodes in the mesentery, it may be necessary to sharply dissect them off these nodes so that the extent of nodal involvement can be better appreciated.
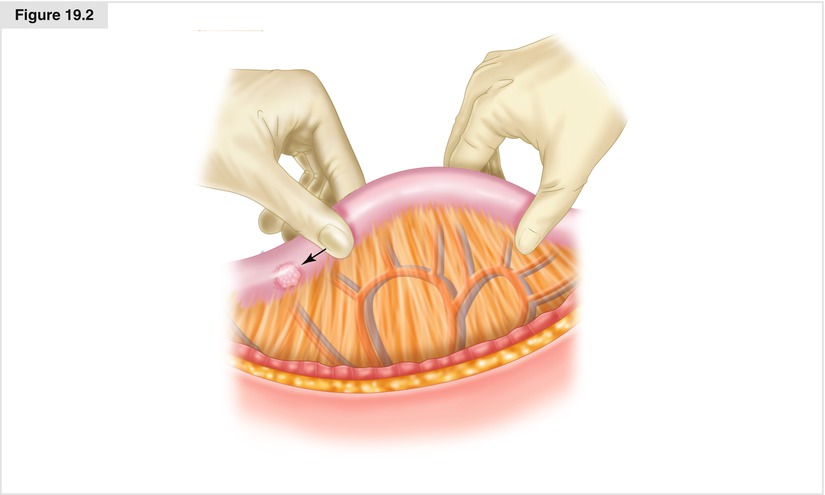
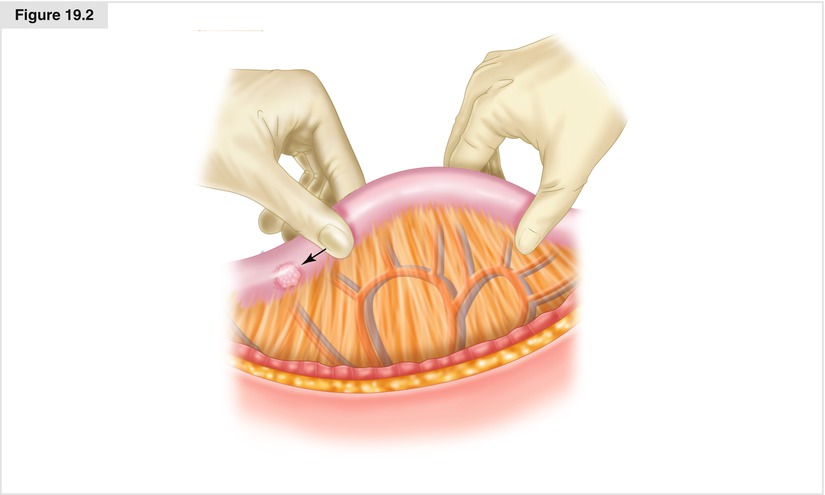
Figure 19.2
Palpation of the small bowel. Beginning at the ligament of Treitz, carefully pull the small bowel through thumb and forefinger to assess for lesions. Mark each lesion with a stitch, or mark the first and last lesions, if they are multiple
19.2.3 Small Bowel Resection and Lymphadenectomy
The extent of resection depends upon the number of lesions, the location of the lesions, and the extent of lymphadenopathy. Single lesions in the jejunum or proximal ileum require a segmental bowel resection and regional lymphadenectomy, to encompass those nodes draining along the segmental vessels supplying that portion of the small bowel (Fig. 19.4). If there is a single lesion without bulky central mesenteric lymphadenopathy, resection of approximately 30 cm of small bowel is generally required.
If there are multiple lesions, one must carefully consider how much bowel should be resected. It is generally preferable to remove one long segment and have one anastomosis, rather than removing multiple segments and having two or more anastomoses. If multiple resections and anastomoses are planned and an adequate lymphadenectomy is performed, one needs to take into account whether the blood supply to the intervening bowel segment may be compromised. Prior to resection, measure the length of bowel from the ligament of Treitz to the proposed site of transection, then from the distal resection margin to the ileocecal valve; carefully record these numbers. Also measure the length of bowel within the proposed lines of transection. Most patients will have 300–600 cm of small bowel, and even with multifocal tumor or significant involvement of the mesentery, we try to keep resections to less than 100 cm. Short-gut syndrome is a risk if one cannot preserve about 200 cm of bowel. Preservation of the ileocecal valve, if possible, can help the situation. If there are very small lesions distant from the main tumor(s), for which lymph node involvement would be unlikely (such as with lesions smaller than 2–4 mm), one might consider local excision of these lesions in order to preserve more bowel length.
Many lesions are found right at the ileocecal valve or in the terminal 30 cm of the ileum. To perform an adequate lymphadenectomy, the ileocolic artery and vein must be sacrificed (Fig. 19.4), so the terminal 20–30 cm of ileum, as well as the right colon, will be devascularized and must be removed. How much colon to remove will depend on the adequacy of flow from either the middle colic or right colic artery to the hepatic flexure. If a good pulse can be palpated in the adjacent mesentery, I try to save the hepatic flexure and perform an anastomosis of the proximal small bowel to the colon just below the right colic artery in the upper ascending colon.
Once the transection points of the bowel have been determined, create a small opening in the mesentery adjacent to the small bowel using electrocautery or a clamp. Place a GIA™-80 stapler (Medtronic–Covidien; Minneapolis, MN, USA) through this, then transect the bowel using a blue (3.5-mm) load. Repeat this procedure for the distal site of the transection in the colon or small bowel. Next, score the mesentery leading away from the point of transection, converging with a similar line from the other point of transection, carefully including the major segmental vessels and their lymph nodes. Make sure to include all these nodes and any others that appear enlarged. Divide the mesentery between clamps, then suture ligate with 2-0 silk sutures, or alternatively, use a device such as the LigaSure™ Impact (Medtronic–Covidien). Continue this dissection until the point where the segmental vessel comes off the SMA. There will often be nodes at this point, which can be carefully dissected from the base of this vessel by dividing the soft tissue over the surface of the vessel. I recommend holding the nodes and segmental vessel in one hand and pulling them away from the SMA; then take small amounts of the fibrofatty tissue at a time with electrocautery or the LigaSure™. Rotate the nodes while palpating the vessel to finish dividing the tissue, until the takeoff of the artery and vein from the SMA and SMV is directly visualized. Pull the nodes toward the specimen, freeing up the area 1 cm from the surface of the SMA and SMV; then doubly clamp the artery and vein (Fig. 19.5). Divide between the clamps and pass off the specimen. Suture ligate the segmental vessels with 2-0 silk without encroaching upon the main trunk of the SMA and SMV. When hemostasis has been achieved, assess the color of the bowel at the transection sites, and try to palpate a pulse in the subsegmental artery feeding each side. Sometimes an additional 5–10 cm of small bowel (usually proximally) should be resected if it has a congested appearance and there may be questions regarding inflow. As long as there is adequate length of bowel, one should have a low threshold to resect such segments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree