Fig. 8.1
A surgical stapler is used to divide the stomach from a point just proximal to the pylorus up to the esophageal hiatus. Note the bougie within the gastric lumen and the stapler dividing just lateral to it. (Adapted from [36])
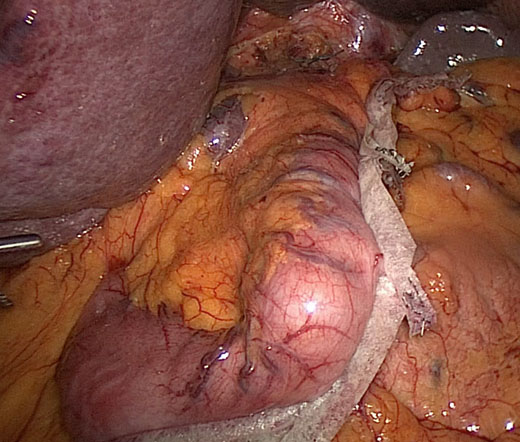
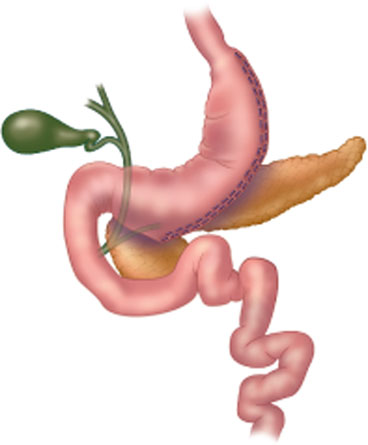
Fig. 8.3
Intraoperative view of completed sleeve gastrectomy, with manufactured buttress material used along the staple line. (Courtesy: Cedars-Sinai Medical Center)
Postoperative Management
Early
In-Hospital Care
Immediate postoperative care includes monitoring of vital signs, urine output, and pain. Inpatient staff assess for signs of dehydration, bleeding, sepsis, pulmonary embolism, and deep venous thrombosis . In some centers, postoperative esophagram swallow study is routinely performed to assess the staple line prior to initiating a diet. Others perform esophagram selectively. Though there is no data specifically on the use of routine imaging studies following sleeve gastrectomy, we can draw a corollary from the gastric bypass literature in which research suggests there is no need for imaging unless clinically indicated [14] (Fig. 8.4).


Fig. 8.4
Normal upper gastrointestinal soluble contrast study following sleeve gastrectomy. There is a radiopaque drain seen overlying the stomach as well as several clips surrounding the sleeve gastrectomy. (Courtesy: Cedars-Sinai Medical Center)
Dietary Progression
Dietary progression begins with a sugar-free liquid diet on postoperative day 1–2. This consists of sugar-free juices, broth, protein shakes, and gelatin. This diet continues for the first 1–2 weeks, then progresses over the following 4–5 weeks from pureed to soft foods. Regular diet is usually reached around 6 weeks after surgery [15] (Table 8.1).
Time postoperatively | Week 1–2 | Week 3–4 | Week 5 | Week 6 and maintenance |
|---|---|---|---|---|
Texture | Liquid | Pureed | Soft solid | Solid |
Acceptable foods | Thin broth, juice, skim milk, sugar-free gelatin, protein shakes | Pudding, oatmeal, yogurt, and pureed meats, fruits, and vegetables | Cooked vegetables, canned fruits, moist cooked meats, soft noodles | Whole grains, tender meats, raw and cooked vegetables and fruits |
Dry or more fibrous foods do not pass easily through the sleeve. Items such as chicken or raw vegetables, if not chewed well, will be regurgitated. Patients are advised to chew their food thoroughly and wait between bites. At mealtime, protein-based foods should be prioritized, with carbohydrate- or fat-rich foods later in the meal. This will ensure that protein malnutrition does not develop. Liquids, especially carbonated ones, should be avoided during meals, as they fill up space in the small sleeve. To avoid daytime hunger, protein-based snacks should be taken in small amounts between meals.
Dehydration is common in the early postoperative period due to the small volume of the sleeve. The patient must be persistent in drinking liquids throughout the day to ensure adequate hydration. As postoperative gastric edema decreases, the capacity of the sleeve becomes larger and dehydration less common.
Late
Micronutrient supplementation is advised for all bariatric surgery patients [16, 17], though little has been published on specific postoperative deficiencies in sleeve gastrectomy patients. Consensus guidelines recommend supplementation with a multivitamin, calcium with vitamin D, folic acid, elemental iron, and vitamin B12, with regular monitoring of micronutrient levels postoperatively [12]. Vitamin B12 deficiency is thought to be due to insufficient production of intrinsic factor and inadequate B12 intake, while iron absorption may be affected by alterations in acid production [15]. Thiamine deficiency resulting in Wernicke’s encephalopathy has been described in case reports following sleeve gastrectomy [18] (Table 8.2).
Supplement | Recommended daily amount | Timing | Laboratory tests to follow |
|---|---|---|---|
Chewable multivitamin | One | Take with meal, protein drink, or milk to improve tolerance | Thiamine, folate, zinc, copper, vitamin A, B6, E, K |
Chewable or liquid calcium with vitamin D | 1000–1500 mg calcium 400–800 mg vitamin D | Do not take with iron to improve absorption | Vitamin D, PTH, calcium, phosphorous |
Sublingual B12 | 500 μg | Take with MVI | Vitamin B12 |
Chewable elemental iron | 325 mg | Do not take with calcium to improve absorption | Ferritin, iron, total iron-binding capacity, CBC |
Regular postoperative visits to the surgeon and dietician are designed to recognize complications such as nutritional deficiencies, but also to help eliminate poor dietary choices and avoid weight regain. Visits occur every 3 months for the first year, then annually thereafter. Many bariatric centers host regular seminars for their postoperative patients to encourage good dietary habits.
Outcomes
Weight Loss
Weight loss is rapid following surgery. In the bariatric literature, weight goals are measured as the percent of excess weight lost (%EWL) . This measurement takes in to account the starting body weight, current body weight, and ideal body weight. At 12 months postoperatively, average %EWL is between 55 and 75 % [19–21], but has been reported as high as 84.8 % [22]. Peak weight loss is seen between 12 and 24 months (average 18 months) after surgery, with some patients experiencing an increase in weight thereafter. Braghetto et al. reported weight regain in 30 % of patients at 5 years postoperatively, with average %EWL of 57.3 [22]. Bohdjalian found similar results, with 19 % of patients regaining weight and %EWL falling to 55.0 % at 5 years [23]. This was corroborated by a review of the published data by Gagner et al. [24] (Table 8.3).
Table 8.3
Percent excess weight loss (%EWL) at 12, 24, and 36 months following sleeve gastrectomy
Article | %EWL 12 months | %EWL 24 months | %EWL 36 months |
|---|---|---|---|
Braghetto [22] | 84.8 | 71.5 | |
Yaghoubian [19] | 72.0 | ||
Carlin [20] | 60 | 60 | 56 |
Himpens [34] | 57.7 | 66 | |
Bohdjalian [23] | 57.5 | 60.3 | 60.0 |
Pequignot [28] | 54.2 | 57.7 | |
Eisenberg [21] | 61 |
Weight regain may be a result of dilation of the sleeve over time, which results in less restriction. Patients find that they can eat larger volumes of food several years after surgery. While this may be the natural history of the sleeve gastrectomy, it can likely be prevented by avoiding carbonated liquids and mixing of solids and liquids, both of which stretch the pouch over time. Emphasis should be placed on prevention; however should medical management and counseling fail, surgical revision as a salvage maneuver remains an option. Revision from sleeve gastrectomy to gastric bypass addresses both weight regain and reflux disease [25]. Resizing or narrowing of the sleeve has also been described [26], as well as placement of an adjustable gastric band around the sleeve [27] .
Effect on Comorbidities
Sleeve gastrectomy has proven to be very effective treatment for obesity-related comorbidities. Most studies report resolution or improvement of diabetes, hypertension, and hyperlipidemia in greater than 60 % of patients at 3–5-year follow-up [20, 22, 28]. Pequignot et al. found that comorbidities continued to improve between years 1 and 2 after surgery, despite no change in %EWL. In multivariate analysis, preoperative elevated systolic blood pressure was the only negative predictive factor for resolution of metabolic syndrome [28]. Studies report resolution of diabetes in 70–100 % of patients [22].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree